Your Benefit Guide New State Health Plan PPO for Employees Hired Or Rehired on Or After April 1, 2010
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Alliance Formation Puzzle in Contests with Capacity-Constraints: a Test Using American Football Reception-Coverage Contest Data
PLOS ONE RESEARCH ARTICLE The alliance formation puzzle in contests with capacity-constraints: A test using American football reception-coverage contest data 1 2 1 Justin Ehrlich , Matthew Harmon , Shane SandersID * 1 Syracuse University, Syracuse, NY, United States of America, 2 NFL.com, NFL, Syracuse, NY, United States of America * [email protected] a1111111111 a1111111111 a1111111111 a1111111111 Abstract a1111111111 We utilize a contest-theoretic model to demonstrate a version of the alliance formation puz- zle that aligns with reception-coverage contests in American football. Namely, secondary defenders can opt for single-coverageÐ1 v 1 contest. Alternatively, they can choose to ally Ðform double-coverage or 2 v 1 contest with exogenous intra-alliance prize divisionÐwhen OPEN ACCESS defending a given receiver. In our theoretical treatment, we find that defenses have a lower Citation: Ehrlich J, Harmon M, Sanders S (2020) equilibrium success rate in preventing the receiver from ªgetting openº under double-cover- The alliance formation puzzle in contests with capacity-constraints: A test using American football age than under single-coverage in the absence of capacity constraints. We also find that reception-coverage contest data. PLoS ONE 15(3): this success rate paradox is a necessary condition for the alliance formation puzzle. We e0227750. https://doi.org/10.1371/journal. then test the theoretical treatment by analyzing 8,508 plays of NCAA and NFL game data pone.0227750 within a set of fixed effects, logistic regression models that control for receiver, level-of-play, Editor: Jason Anthony Aimone, Baylor University, and season-of-play. We find that equilibrium level of defensive success rises significantly UNITED STATES and substantially (p-value < 0.01 and marginal effect of between 13 and 17 percentage Received: May 17, 2019 points) when moving from single-coverage to double-coverage, ceteris paribus. -

The Ice Bowl: the Cold Truth About Football's Most Unforgettable Game
SPORTS | FOOTBALL $16.95 GRUVER An insightful, bone-chilling replay of pro football’s greatest game. “ ” The Ice Bowl —Gordon Forbes, pro football editor, USA Today It was so cold... THE DAY OF THE ICE BOWL GAME WAS SO COLD, the referees’ whistles wouldn’t work; so cold, the reporters’ coffee froze in the press booth; so cold, fans built small fires in the concrete and metal stands; so cold, TV cables froze and photographers didn’t dare touch the metal of their equipment; so cold, the game was as much about survival as it was Most Unforgettable Game About Football’s The Cold Truth about skill and strategy. ON NEW YEAR’S EVE, 1967, the Dallas Cowboys and the Green Bay Packers met for a classic NFL championship game, played on a frozen field in sub-zero weather. The “Ice Bowl” challenged every skill of these two great teams. Here’s the whole story, based on dozens of interviews with people who were there—on the field and off—told by author Ed Gruver with passion, suspense, wit, and accuracy. The Ice Bowl also details the history of two legendary coaches, Tom Landry and Vince Lombardi, and the philosophies that made them the fiercest of football rivals. Here, too, are the players’ stories of endurance, drive, and strategy. Gruver puts the reader on the field in a game that ended with a play that surprised even those who executed it. Includes diagrams, photos, game and season statistics, and complete Ice Bowl play-by-play Cheers for The Ice Bowl A hundred myths and misconceptions about the Ice Bowl have been answered. -

Mentor 1 the Matchup
@SIHSSports sihsathletics sihssports 2019 GAME NOTES WEEK TWO: IGNATIUSWILDCATS.COM MENTOR 1 THE MATCHUP Team Information Saint Ignatius High School: 1-0 OHSAA Division I, Region 1 Head Coach: Chuck Kyle ‘69 Record at School: 354-90-1 at Overall Record: 354-90-1 Mentor Cardinals: 1-0 OHSAA Division I, Region 1 Saint Ignatius Mentor Head Coach: Steve Trivisonno Record at School: 197-69 WILDCATS CARDINALS Overall Record: 197-69 September 6, 2019 Media Information Jerome T. Osborne Sr. Stadium For information and credential Kickoff: 7 pm requests, contact: Joe Ginley ‘12 Saint Ignatius Schedule Communications Coordinator for Athletics Date Opponent Time/Score (P): 216-651-0222 x242 8/31 @ Loyola Academy (IL) W, 27-10 email: [email protected] 9/6 @ Mentor 7:00 pm For full coverage of the Wildcats, 9/13 @ Archbishop Hoban 7:00 pm visit ignatiuswildcats.com. 9/21 @ DeMatha Catholic (MD) 1:00 pm 9/28 vs. Clarkson Football North (ONT) 5:00 pm Broadcast Information 10/5 vs. Rockledge (FL) 8:00 pm 10/12 @ St. Edward 7:00 pm Saint Ignatius Broadcasting 10/19 @ Archbishop Moeller 2:00 pm Network 10/26 vs. St. Xavier 2:00 pm Play-by-Play: Jack O’Rourke ’20 Color Analyst: Nick Fletcher ’20 11/2 vs. West Toronto Prep (ONT) 7:00 pm Analyst/Show Host: Max Marazzi ’20 Moderator: Joe Ginley ’12 / Follow the Wildcats on social media for full Jeff McCormick ’83 coverage of every Saint Ignatius team. (P): 216-651-0222 email: [email protected] [email protected] @SIHSSports sihsathletics sihssports And also visit .. -

State of Wisconsin Group Health Insurance Program Agreement
State of Wisconsin Group Health Insurance Program Agreement Issued by the State of Wisconsin Department of Employee Trust Funds On behalf of the Group Insurance Board Release Date: October 19, 2018 TABLE OF CONTENTS Table of Contents ..................................................................................................................... 2 000 Definitions ......................................................................................................................... 7 100 General .............................................................................................................................11 105 Introduction .....................................................................................................................11 110 Objectives .......................................................................................................................11 115 General Requirements ....................................................................................................12 120 Board Authority ...............................................................................................................16 125 Eligibility ..........................................................................................................................17 125A General .....................................................................................................................17 125B Dependent Coverage Eligibility ..................................................................................20 -

Apba Football
APBA FOOTBALL Conducting Season Replays & Tips for Solitaire Play Introduction • Preparation • Standardization • Setup • Method of Play (Neutral Downs) • Method of Play (Trick Plays) • Method of Play (Situational Downs) Preparation • Recommend using Phil Milloy’s “Dice Range Calculator” as an alternative to Section III of the APBA rule book • Determine Receiver, Sack, & Interception Allocations for every team • Accurately reflects the substitutions within all personnel packages – Pro-Set, 2TEs, 3WR, Standard, Nickel & Dime Defenses • Speeds up play – Only one dice roll required instead of rolling until a starter is selected – Eliminates having to “rotate” players • Reserve players are active participants Dice Range Calculator Preparation • Optional Innovations – “Fletch67” Defensive Ratings (S.Fletcher) – H. Ahlskog’s “Forced Fumble & Recovery” Charts – H. Ahlskog’s “Fumble Frequency Number” for skill/special teams players – Sack Modification (Barath) • Upon sack, determine defender through “Allocation” system • Roll dice, if dice roll is between 11 – 51, award defender full sack. • If dice roll is 52 -66, roll dice again and check for new defender via “Allocation” system. • If same player, award defender full sack. If different defender, each player is awarded ½ a sack. Proprietary to Mark Zarb • Optional Innovations – “Sack & Interception” Ratings • Based off each team’s sack & interception per attempt – "Yards Per Catch" (YPC) Receiver Ratings • Distinguishes between deep threats, possession receivers and RBs catching out of backfield -
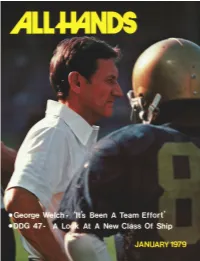
George Welsh, Is Thesubject of a Feature Beginning on Page 16
Ohio, the nation’s,first Trident mi.ssile,firing.suh- rnarine, clwarfi the SSN 688-class attack suh- marine Jacksonville (SSN 699) ufloat in graving ~l~~~~k,follo~~inglaunc~hingin Nvvenlher at Groton. Conn. Ohio i.s .schetlulecl,fi~r/aunc,hinR this year. (General Dvnarnic,.s photo.) ALL WIND6 MAGAZINE OF THE US. NAW"56th YEAR OF PUBLICATION JANUARY 1979 NUMBER 744 Chief of Naval Operations: ADM Thomas B. Hayward Chief of Information: RADM .David M. Cooney OIC Navy Internal Relations Act.: CAPT James E. Wentz Features 6 DDG 47"SHE MAY LOOK THE SAME BUT ... A look at a new class of ship for the 1980s Page 10 10 FAMILY ADVOCACYPROGRAM Expanded program deals with spouse as well as child 13 NAW RELIEFHITS 75 Dispensing aid without benefit of a budget 16 GEORGEWELSH-"IT'S BEEN A TEAM EFFORT" His thoroughness is his mark of excellence 24 ENERGYCONSERVATION EFFORTS REAP AWARDS Sea and shore commands win SecNav Energy Awards 28 GREATLAKES CRUISE Mid-America responds to visits by three destroyers 30 SOUNDFOCUSING ON BLOODSWORTH ISLAND Chesapeake Bay range has served Navy since 1942 34 MEDICAL AND HEALTHCARE Second in a new series of Navy Rights and Benefits 42 MINORITY RECRUITMENTAT INDIAN HEAD One individual's novel approach to a difficult task 46 PLANNING FOR TOMORROW Paae 34 What's new and better aboard Pacific Fleet ships Departments Currents-2; Bearings-22; Mail Buoy-48 Covers Front: Navy's winning football coach, George Welsh, is thesubject of a feature beginning on page 16. Photo by D.B. Eckard. Back Sunset on Bloodsworth Island. -

Axiomatic Design of a Football Play-Calling Strategy
Axiomatic Design of a Football Play-Calling Strategy A Major Qualifying Project Report Submitted to the Faculty of the WORCESTER POLYTECHNIC INSTITUTE in partial fulfillment of the requirements for the Degree of Bachelor of Science in Mechanical Engineering by _____________________________________________________________ Liam Koenen _____________________________________________________________ Camden Lariviere April 28th, 2016 Approved By: Prof. Christopher A. Brown, Advisor _____________________________________________________________ 1 Abstract The purpose of this MQP was to design an effective play-calling strategy for a football game. An Axiomatic Design approach was used to establish a list of functional requirements and corresponding design parameters and functional metrics. The two axioms to maintain independence and minimize information content were used to generate a final design in the form of a football play card. The primary focus was to develop a successful play-calling strategy that could be consistently repeatable by any user, while also being adaptable over time. Testing of the design solution was conducted using a statistical-based computer simulator. 2 Acknowledgements We would like to extend our sincere gratitude to the following people, as they were influential in the successful completion of our project. We would like to thank Professor Christopher A. Brown for his advice and guidance throughout the yearlong project and Richard Henley for sharing his intellect and thought process about Axiomatic Design and the role -

Supervisor's Guide
If you have issues viewing or accessing this file contact us at NCJRS.gov. Manual for Police Traffic Services Volume II Personnel Performance Evaluation System Supervisor's Guide September 1977 ., r- '" I - "- L \J , I ---.,- V) \f) ¢ Manual for Police Traffic Services Volume Personnel Performan(:e II Evaluation System Supervisor's Guide -----------------------------------.,,:, September 1977 U.S. Department of Transportation National Highway Traffic Safety Administration Washington, D.C. 20590 Foreword The National Highway Traffic Safety Administration has a mandated responsibility for improvement and maintenance of traffic safety on our country's highways. In carrying out this responsibility, NHTSA sponsors a wide range of research and develop ment activities, each of which in some way relates to highway traffic safety. The evaluation system described in this Manual was developed under NHTSA spon sorship and has a direct relationship to highway safety through law enforcement agen cies that provide police traffic services. The use of this system will help such agencies determinie if the quantity and quality of the Police Traffic Services (PTS) that they provide are at acceptable levels. Obv10usly, when a. sufficient amount of appropriate services is applied, it can be anticipated that traffic law compliance and, thus, safety will increase. This system has been designed to provide a reasonably precise measure of a patrol man's actual performance of police traffic services. This is an important characteristic. The measures are of specific, defined parts of the patrolman's job and they are quantita tive. The measures are not subjective. In addition, the system provides for the evaluation of the quality of performance by means of a systematic assessment of all of the tasks the patrolman must perform in carrying out each major part of traffic services; Basi cally, this system produces information about the performance of an individual patrol man. -

Offensive Philosophy in Front Office Football
Offensive Philosophy in Front Office Football When you first play Front Office Football, the game handles your depth charts and game plans. If you want to do this yourself, you need to change the settings through the Controls – Options menu, using the Edit Single-Player Options screen. In multi-player leagues, commissioners control these settings for the entire league using the Edit Multi-Player Options screen. Once the AI is turned off, the changes you make using the Game Day – Planning menu are used during simulated games. If you’re accustomed to the way Front Office Football used to handle offense, many fundamental concepts have changed. As Front Office Football evolves, as it has for nearly 20 years now, so has professional football. Player Positions and Skills In Front Office Football, offensive players are closely tied to their positions. When a player gains experience, he gains experience specific to his position. You can change a player’s primary position, but it might change his ratings significantly. You’ll get an idea of how much the ratings will change when you make the position change. Offensive players can play out of position and gain experience for that new position, but they generally are more effective when their position matches their assigned position. This is very different from the defensive system, where defensive players can switch positions and play out of position without penalty. Some positions are closely related. Offensive linemen can play anywhere on the line. Running backs and fullbacks share many attributes, as do flankers and split ends (X and Z receivers). -

Strat-O-Matic Football Rules
Strat-O-Matic Football Rules 2014 Card Season Revised 12-17-2015 01/10/2015 Page 1 01/10/2015 Page 2 2014 Season Cards This set of rules encompasses all rules previously found in the rule booklet and on the roster sheets, as well as the newly introduced rules and optional rules adopted by the League Rules Committee. In addition some rules found within the official Strat-O-Matic Computer rules have been deleted or modified to better suit play within this league. INTRODUCTION First and foremost all rules of football apply. If a conflict occurs concerning a particular aspect of the game use common sense to resolve the dispute applying the rules of the NFL. If the exact rule is not known at that time try to find the answer in a timely manner and if a solution is not reached resolve the dispute by a die roll and continue play. It is after all just a game. TABLE OF CONTENTS 2013 Season Cards ..................................................................................................................................................................................... 3 INTRODUCTION ..................................................................................................................................................................................... 3 TABLE OF CONTENTS ........................................................................................................................................................................... 3 IMPORTANT CHANGES TO THE RULES FROM THE PAST SEASONS......................................................................................... -

Bailey: ‘Barring Any Setbacks, I’Ll Be out There’
Bailey: ‘Barring Any Setbacks, I’ll Be Out There’ By Stuart Zaas DenverBroncos.com November 27, 2013 Cornerback Champ Bailey talked about his status for this week’s game at Kansas City. ENGLEWOOD, Colo. – After missing the past four games with a foot injury, cornerback Champ Bailey feels he’s getting closer to making his return this week at Kansas City. Bailey sat out the first five games of the season with a foot injury before reinjuring the foot at Indianapolis in Week 7. The patience required to let the foot heal is something that hasn’t come easily for the 15th-year veteran. “That’s the hardest thing for me,” Bailey said. “Any time something goes wrong, I want to be in there to try to help. But, I have to make sure I take care of my body. The foot is feeling a lot better. I’m going to keep progressing through the week to make sure that I’m ready for Sunday.” Bailey returned to practice on Wed., Nov. 13 and has been limited in each session since. He was listed as doubtful for the Week 11 game versus Kansas City and then questionable for Week 12 at New England. This week, he said his prognosis could be more positive. “I feel like barring any setbacks, I’ll be out there," Bailey said. "That’s the way I’m preparing myself this week – to play. And if nothing goes wrong, I’ll be there.” Bailey has been listening to the doctors’ advice as well as his own body as he rehabilitates the foot. -

Fire Service Consultants 9 Heritage Rd
KRAMER & ASSOCIATES GROUP Fire Service Consultants 9 Heritage Rd. Blue Ash, OH 45241 513-678-2279 and Analysis of Fire Department Facilities and Operations Feb. 2, 2016 SMITHFIELD, RHODE ISLAND Project Team Leader: William M. Kramer, Ph.D. Project Team Associates: Nestor Melnyk, AIA NCARB Randall W. Hanifen, Ph.D. Michael Washington, B.S. Cari A. Kramer, B.B.A. EMT-P Daniel Montgomery, AIA LEED A SMITHFIELD, RHODE ISLAND Analysis of Fire Department Facilities and Operations Table of Contents I. FOREWORD........................................................................... P 4 II. EXECUTIVE SUMMARY .................................................... P 8 III. HISTORICAL PERSPECTIVE .......................................... P 12 IV. SMITHFIELD OVERVIEW ............................................... P 15 V. BALANCING FIRE AND EMS RESPONSES .................. P 16 VI. RESPONSE DATA ............................................................... P 18 VII. BRYANT UNIVERSITY AS A FACTOR .......................... P 21 VIII. INTRO: ARCHITECTURAL REVIEW OF STATIONS P 27 IX. FIRE STATION LOCATIONS ............................................ P 32 X. REPLACING FIRE STATIONS ......................................... P 47 XI. INVESTING IN NEW FACILITIES ................................. P 50 XII. SMITHFIELD FIRE DEPT. APPARATUS .................... P 54 XIII. ORGANIZATIONAL LEADERSHIP ............................... P 68 XIV. FUTURE SCHEDULING ................................................... P 74 XV. COMMUNICATIONS AND DISPATCH ........................