Antileishmanial Compounds from Nature - Elucidation of the Active Principles of an Extract from Valeriana Wallichii Rhizomes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Academy of Strategic and Organizational Leadership
Allied Academies National Conference Myrtle Beach, South Carolina April 7-11, 1999 Academy of Strategic and Organizational Leadership Proceedings Affiliates Journals International Academy for Case Studies Journal of the International Academy for Case Studies Academy of Entrepreneurship Academy of Entrepreneurship Journal and the Entrepreneurial Executive Academy of Accounting and Financial Studies Academy of Accounting and Financial Studies Journal Academy of Managerial Communications Academy of Managerial Communications Journal Academy of Educational Leadership Academy of Educational Leadership Journal Academy of Marketing Studies Academy of Marketing Studies Journal Academy of Strategic and Organizational Leadership Academy of Strategic and Organizational Leadership Journal Academy of Free Enterprise Education The Journal of Entrepreneurship Education Academy of Information and Management Sciences Academy of Information and Management Sciences Journal Academy for Studies in Business Law Academy for Studies in Business Law Journal Academy for Economics and Economic Education Economics and Economic Education Research Journal Allied Academies, Inc. PO Box 2689, Cullowhee, NC 28723 An International Non Profit Association Voice 828-293-9151; FAX 828-293-9407 of Scholars and Practitioners www.alliedacademies.org Allied Academies National Conference page ii Volume 4, Number 1 1999 Proceedings of the Academy of Strategic and Organizational Leadership April 7-11, 1999 Myrtle Beach, South Carolina Jo Ann and Jim Carland Co-Editors Western Carolina University The Proceedings of the Academy of Strategic and Organizational Leadership are published by the Allied Academies, Inc., PO Box 2689, Cullowhee, NC, 28723. The Academy of Strategic and Organizational Leadership is an affiliate of the Allied Academies, an international, non-profit association of scholars whose purpose is to support and encourage the exchange of knowledge. -
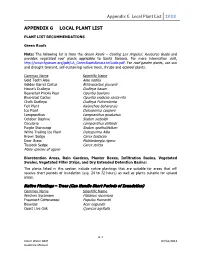
Appendix G Local Plant List 2013 APPENDIX
Appendix G Local Plant List 2013 APPENDIX G LOCAL PLANT LIST PLANT LIST RECOMMENDATIONS Green Roofs Note: The following list is from the Green Roofs – Cooling Los Angeles: Resource Guide and provides vegetated roof plants applicable to Santa Barbara. For more information visit, http://www.fypower.org/pdf/LA_GreenRoofsResourceGuide.pdf. For roof garden plants, use sun and drought tolerant, self-sustaining native trees, shrubs and ecoroof plants. Common Name Scientific Name Gold Tooth Aloe Aloe nobilis Golden Barrel Cactus Echinocactus grusonii Hasse’s Dudleya Dudleya hassei Beavertail Prickly Pear Opuntia basilaris Blue-blad Cactus Opuntia violacea santa-rita Chalk Dudleya Dudleya Pulverulenta Felt Plant Kalanchoe beharensis Ice Plant Delosperma cooperii Lampranthus Lampranthus productus October Daphne Sedum sieboldii Oscularia Lampranthus deltoids Purple Stonecrop Sedum spathulifolium White Trailing Ice Plant Delosperma Alba Brown Sedge Carex testacea Deer Grass Muhlenbergia rigens Tussock Sedge Carex stricta Many species of agave Bioretention Areas, Rain Gardens, Planter Boxes, Infiltration Basins, Vegetated Swales, Vegetated Filter Strips, and Dry Extended Detention Basins: The plants listed in this section include native plantings that are suitable for areas that will receive short periods of inundation (e.g. 24 to 72 hours) as well as plants suitable for upland areas. Native Plantings – Trees (Can Handle Short Periods of Inundation) Common Name Scientific Name Western Sycamore Platanus racemosa Freemont Cottonwood Populus fremontii -

Amer-Sports-Annual-Report-2008.Pdf
CONTENT Amer Sports in brief and key fi gures . .1 CEO’s review . .8 Strategy . .12 Mission and values. .14 Vision. .15 Financial targets . .16 Global landscape . .18 Business segments Winter and Outdoor . .24 Ball Sports . .34 Fitness . .42 R&D. .46 Award winning products . .48 Sales and channel management . .54 Supply chain and IT . .56 Human resources . .58 Social responsibility . .62 Board of Directors report and fi nancial statements . .68 Corporate governance . .136 Board of Directors . .146 Executive Board . .148 Amer Sports key brands . .152 Information for investors . .212 Contact information . .213 NET SALES, EUR MILLION EBIT, EUR MILLION 1,732 *) 1,793 1,652 1,577 117.1*) 120.2 100.5 92.2**) 1,036 78.9 04 05 06 07 08 04 05 06 07 08 *) Pro forma *) Pro forma **) Before non-recurring items EQUITY RATIO, % GEARING, % 56 121 112 115 105 34 32 31 31 29 04 05 06 07 08 04 05 06 07 08 NET SALES BY NET SALES BY BUSINESS SEGMENT GEOGRAPHICAL SEGMENT 1 Winter and Outdoor 55% 1 EMEA 46% 2 Ball Sports 31% 2 Americas 43% 3 Fitness 14% 3 Asia Pacific 11% 123 123 1 Amer Sports is the world’s leading sports equipment company We offer technically-advanced products that improve the performance of sports participants. Our major brands include Salomon, Wilson, Precor, Atomic, Suunto, Mavic and Arc’teryx. The company’s business is balanced by our broad portfolio of sports and our presence in all major markets. Amer Sports was founded in 1950 in Finland. It has KEY BRANDS: been listed on the NASDAQ OMX Helsinki Ltd since • Salomon – the mountain sports company 1977. -

Fort Ord Natural Reserve Plant List
UCSC Fort Ord Natural Reserve Plants Below is the most recently updated plant list for UCSC Fort Ord Natural Reserve. * non-native taxon ? presence in question Listed Species Information: CNPS Listed - as designated by the California Rare Plant Ranks (formerly known as CNPS Lists). More information at http://www.cnps.org/cnps/rareplants/ranking.php Cal IPC Listed - an inventory that categorizes exotic and invasive plants as High, Moderate, or Limited, reflecting the level of each species' negative ecological impact in California. More information at http://www.cal-ipc.org More information about Federal and State threatened and endangered species listings can be found at https://www.fws.gov/endangered/ (US) and http://www.dfg.ca.gov/wildlife/nongame/ t_e_spp/ (CA). FAMILY NAME SCIENTIFIC NAME COMMON NAME LISTED Ferns AZOLLACEAE - Mosquito Fern American water fern, mosquito fern, Family Azolla filiculoides ? Mosquito fern, Pacific mosquitofern DENNSTAEDTIACEAE - Bracken Hairy brackenfern, Western bracken Family Pteridium aquilinum var. pubescens fern DRYOPTERIDACEAE - Shield or California wood fern, Coastal wood wood fern family Dryopteris arguta fern, Shield fern Common horsetail rush, Common horsetail, field horsetail, Field EQUISETACEAE - Horsetail Family Equisetum arvense horsetail Equisetum telmateia ssp. braunii Giant horse tail, Giant horsetail Pentagramma triangularis ssp. PTERIDACEAE - Brake Family triangularis Gold back fern Gymnosperms CUPRESSACEAE - Cypress Family Hesperocyparis macrocarpa Monterey cypress CNPS - 1B.2, Cal IPC -

OCR Document
UNIVERSIDADE FEDERAL DO RIO GRANDE DO SUL CENTRO DE BIOTECNOLOGIA DO ESTADO DO RIO GRANDE DO SUL PROGRAMA DE PÓS-GRADUAÇÃO EM BIOLOGIA CELULAR E MOLECULAR PRODUÇÃO DE VALEPOTRIATOS EM CULTURAS LÍQUIDAS DE PLANTAS DE Valeriana glechomifolia Meyer (VALERIANACEAE) DENISE RUSSOWSKI Tese submetida ao Programa de Pós- Graduação em Biologia Celular e Molecular do Centro de Biotecnologia da Universidade Federal do Rio Grande do Sul como quesito parcial para obtenção do título de Doutor em Ciências Orientador: Prof. Dr. Arthur Germano Fett-Neto Co-Orientadora: Profª Drª Sandra Beatriz Rech Porto Alegre, Março de 2007. 2 INSTITUIÇÕES E FONTES FINANCIADORAS O desenvolvimento deste projeto ocorreu nos seguintes laboratórios: • Laboratório de Fisiologia Vegetal do Departamento de Botânica e Centro de Biotecnologia do Estado do Rio Grande do Sul– UFRGS • Laboratório de Biotecnologia Vegetal do Departamento de Produção de Matéria-Prima – Faculdade de Farmácia – UFRGS • Central Analítica da Faculdade de Farmácia – UFRGS A Comissão de Aperfeiçoamento de Pessoal de Ensino Superior (CAPES) foi responsável pela concessão de bolsa, sendo o apoio financeiro fornecido pelo Programa de Apoio ao Desenvolvimento Científico e Tecnológico (PADCT), Fundação de Amparo à Pesquisa no Estado do Rio Grande do Sul (FAPERGS) e Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) – Grant pesquisador ao orientador. 3 AGRADECIMENTOS Ao orientador Prof. Arthur G. Fett-Neto que me transformou, não geneticamente, mas em um profissional seguramente melhor. Sua orientação irretocável dispensa quaisquer outros comentários. À co-orientadora Profª. Sandra B. Rech pela valiosa ajuda na confecção das amostras para o HPLC, cedência de suas bolsistas e, principalmente, pelos ensinamentos e dedicação. -

44959350027.Pdf
Revista de Biología Tropical ISSN: 0034-7744 ISSN: 2215-2075 Universidad de Costa Rica Rondón, María; Velasco, Judith; Rojas, Janne; Gámez, Luis; León, Gudberto; Entralgo, Efraín; Morales, Antonio Antimicrobial activity of four Valeriana (Caprifoliaceae) species endemic to the Venezuelan Andes Revista de Biología Tropical, vol. 66, no. 3, July-September, 2018, pp. 1282-1289 Universidad de Costa Rica DOI: 10.15517/rbt.v66i3.30699 Available in: http://www.redalyc.org/articulo.oa?id=44959350027 How to cite Complete issue Scientific Information System Redalyc More information about this article Network of Scientific Journals from Latin America and the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Project academic non-profit, developed under the open access initiative Antimicrobial activity of four Valeriana (Caprifoliaceae) species endemic to the Venezuelan Andes María Rondón1, Judith Velasco2, Janne Rojas1, Luis Gámez3, Gudberto León4, Efraín Entralgo4 & Antonio Morales1 1. Organic Biomolecular Research Group. Faculty of Pharmacy and Bioanalysis. University of Los Andes, Mérida, Venezuela; [email protected], [email protected], [email protected] 2. Microbiology and Parasitology Department, Faculty of Pharmacy and Bioanalysis. University of Los Andes, Mérida, Venezuela; [email protected] 3. Faculty of Forestry and Environmental Science. University of Los Andes, Mérida, Venezuela; [email protected] 4. Faculty of Economic and Social Sciences, Statistics School, University of Los Andes, Mérida, Venezuela; [email protected], [email protected] Received 11-II-2018. Corrected 23-V-2018. Accepted 25-VI-2018. Abstract: Valeriana L. genus is represented in Venezuela by 16 species, 9 of these are endemic of Venezuelan Andes growing in high mountains at 2 800 masl. -

ASTERACEAE Christine Pang, Darla Chenin, and Amber M
Comparative Seed Manual: ASTERACEAE Christine Pang, Darla Chenin, and Amber M. VanDerwarker (Completed, April 17, 2019) This seed manual consists of photos and relevant information on plant species housed in the Integrative Subsistence Laboratory at the Anthropology Department, University of California, Santa Barbara. The impetus for the creation of this manual was to enable UCSB graduate students to have access to comparative materials when making in-field identifications. Most of the plant species included in the manual come from New World locales with an emphasis on Eastern North America, California, Mexico, Central America, and the South American Andes. Published references consulted1: 1998. Moerman, Daniel E. Native American ethnobotany. Vol. 879. Portland, OR: Timber press. 2009. Moerman, Daniel E. Native American medicinal plants: an ethnobotanical dictionary. OR: Timber Press. 2010. Moerman, Daniel E. Native American food plants: an ethnobotanical dictionary. OR: Timber Press. Species included herein: Achillea lanulosa Achillea millefolium Ambrosia chamissonis Ambrosia deltoidea Ambrosia dumosa Ambrosia eriocentra Ambrosia salsola Artemisia californica Artemisia douglasiana Baccharis pilularis Baccharis spp. Bidens aurea Coreopsis lanceolata Helianthus annuus 1 Disclaimer: Information on relevant edible and medicinal uses comes from a variety of sources, both published and internet-based; this manual does NOT recommend using any plants as food or medicine without first consulting a medical professional. Achillea lanulosa Family: Asteraceae Common Names: Yarrow, California Native Yarrow, Common Yarrow, Western Yarrow, Mifoil Habitat and Growth Habit: This plant is distributed throughout the Northern Hemisphere. It is native in temperate areas of North America. There are both native and introduced species in areas creating hybrids. Human Uses: This plant has a positive fragrance making it desired in gardens. -

UJPAH 2018 Final JOURNAL(14-06-2018)
RNI No. DEL/1998/4626 ISSN 0973-3507 UUnniivveerrssiittiieess'' JJoouurrnnaall ooff PPhhyyttoocchheemmiissttrryy aanndd AAyyuurrvveeddiicc HHeeiigghhttss Vol. I No. 24 June 2018 Mangifera indica (Mango) Syzygium cumini (Jamun) Cinnamomum zeylanicum (Dalchini) Cinnamomum tamala (Tejpatta) Abstracted and Indexed by NISCAIR Indian Science Abstracts Assigned with NAAS Score Website : www.ujpah.in UJPAH Vol. I No. 24 JUNE 2018 Editorial Board Dr. Rajendra Dobhal Dr. S. Farooq Dr. I.P Saxena Dr. A.N. Purohit Chairman, Editorial Board Chief Editor Editor Patron Director, UCOST, Director, International Instt. Ex. V.C. H.N.B. Garhwal Univ'., Ex. V.C. H.N.B. Garhwal Univ'., Dehradun, UK, India of Medical Science, Srinagar, Garhwal, Srinagar, Garhwal, Dehradun, UK, India UK., India UK., India Advisory Board Dr. Himmat Singh : Chairman, Advisory Board Former Advisor, R N D, BPCL, Mumbai, India Dr. B.B. Raizada : Former Principal, D.B.S College, Dehradun, UK., India Dr. Maya Ram Uniyal : Ex-Director, Ayurved (Govt. of India) and Advisor, Aromatic and Medicinal Plant (Govt. of Uttarakhand), India Ms. Alka Shiva : President and Managing Director, Centre of Minor Forest Products (COMFORPTS), Dehradun, UK., India Dr. Versha Parcha : Head, Chemistry Department, SBSPGI of Biomedical Sciences and Research, Dehradun, UK., India Dr. Sanjay Naithani : Ex-Head, Pulp and Paper Division, FRI, Dehradun, UK., India Dr. Iqbal Ahmed : Reader, Department of Agriculture Microbiology, A.M.U., Aligarh, U.P, India Dr. Syed Mohsin Waheed : Associate Professor, Department of Biotechnology, Graphic Era University, Dehradun, Uk., India Dr. Atul Kumar Gupta : Head, Department of Chemistry, S.G.R.R (P.G) College, Dehradun, UK., India Dr. Sunita Kumar : Associate Professor, Department of Chemistry, MKP College, Dehradun, UK., India Dr. -

Brown's Island Plants
Brown’s Island Plants A photographic guide to wild plants of Brown’s Island Regional Preserve Sorted by Scientific Name Photographs by Wilde Legard Botanist, East Bay Regional Park District Revision: February 23, 2007 More than 2,000 species of native and naturalized plants grow wild in the San Francisco Bay Area. Most are very difficult to identify without the help of good illustrations. This is designed to be a simple, color photo guide to help you identify some of these plants. The selection of plants displayed in this guide is by no means complete. The intent is to expand the quality and quantity of photos over time. The revision date is shown on the cover and on the header of each photo page. A comprehensive plant list for this area (including the many species not found in this publication) can be downloaded at the East Bay Regional Park District’s wild plant download page at: http://www.ebparks.org. This guide is published electronically in Adobe Acrobat® format to accommodate these planned updates. You have permission to freely download, distribute, and print this pdf for individual use. You are not allowed to sell the electronic or printed versions. In this version of the guide, the included plants are sorted alphabetically by scientific name. Under each photograph are four lines of information, based on upon the current standard wild plant reference for California: The Jepson Manual: Higher Plants of California, 1993. Scientific Name Scientific names revised since 1993 are NOT included in this edition. Common Name These non-standard names are based on Jepson and other local references. -

Thermally Induced Actinidine Production in Biological Samples Qingxing Shi, Yurong He, Jian Chen,* and Lihua Lu*
pubs.acs.org/JAFC Article Thermally Induced Actinidine Production in Biological Samples Qingxing Shi, Yurong He, Jian Chen,* and Lihua Lu* Cite This: https://dx.doi.org/10.1021/acs.jafc.0c02540 Read Online ACCESS Metrics & More Article Recommendations *sı Supporting Information ABSTRACT: Actinidine, a methylcyclopentane monoterpenoid pyridine alkaloid, has been found in many iridoid-rich plants and insect species. In a recent research on a well-known actinidine- and iridoid-producing ant species, Tapinoma melanocephalum (Fabricius) (Hymenoptera: Formicidae), no actinidine was detected in its hexane extracts by gas chromatography−mass spectrometry analysis using a common sample injection method, but a significant amount of actinidine was detected when a solid injection technique with a thermal separation probe was used. This result led us to hypothesize that heat can induce the production of actinidine in iridoid-rich organisms. To test our hypothesis, the occurrence of actinidine was investigated in four iridoid-rich organisms under different sample preparation temperatures, including two ant species, T. melanocephalum and Iridomyrmex anceps Roger (Hymenoptera: Formicidae), and two plant species, Actinidia polygama Maxim (Ericales: Actinidiaceae) and Nepeta cataria L. (Lamiales: Lamiaceae). Within a temperature range of 50, 100, 150, 200, and 250 °C, no actinidine was detected at 50 °C, but it appeared at temperatures above 100 °C for all four species. A positive relationship was observed between the heating temperature and actinidine production. The results indicate that actinidine could be generated at high temperatures. We also found that the presence of methylcyclopentane monoterpenoid iridoids (iridodials and nepetalactone) was needed for thermally induced actinidine production in all tested samples. -

Valeriana Officinalis L., Valeriana
plants Article Comparative and Functional Screening of Three Species Traditionally used as Antidepressants: Valeriana officinalis L., Valeriana jatamansi Jones ex Roxb. and Nardostachys jatamansi (D.Don) DC. Laura Cornara 1, Gabriele Ambu 1, Domenico Trombetta 2 , Marcella Denaro 2, Susanna Alloisio 3,4, Jessica Frigerio 5, Massimo Labra 6 , Govinda Ghimire 7, Marco Valussi 8 and Antonella Smeriglio 2,* 1 Department of Earth, Environment and Life Sciences, University of Genova, 16132 Genova, Italy; [email protected] (L.C.); [email protected] (G.A.) 2 Department of Chemical, Biological, Pharmaceutical and Environmental Sciences, University of Messina, Via Giovanni Palatucci, 98168 Messina, Italy; [email protected] (D.T.); [email protected] (M.D.) 3 ETT Spa, via Sestri 37, 16154 Genova, Italy; [email protected] 4 Institute of Biophysics-CNR, 16149 Genova, Italy 5 FEM2 Ambiente Srl, Piazza della Scienza 2, 20126 Milan, Italy; [email protected] 6 Department of Biotechnology and Bioscience, University of Milano-Bicocca, Piazza della Scienza 2, 20126 Milan, Italy; [email protected] 7 Nepal Herbs and Herbal Products Association, Kathmandu 44600, Nepal; [email protected] 8 European Herbal and Traditional Medicine Practitioners Association (EHTPA), Norwich 13815, UK; [email protected] * Correspondence: [email protected]; Tel.: +39-0906-764-039 Received: 6 July 2020; Accepted: 2 August 2020; Published: 5 August 2020 Abstract: The essential oils (EOs) of three Caprifoliaceae species, the Eurasiatic Valeriana officinalis (Vo), the Himalayan Valeriana jatamansi (Vj) and Nardostachys jatamansi (Nj), are traditionally used to treat neurological disorders. Roots/rhizomes micromorphology, DNA barcoding and EOs phytochemical characterization were carried out, while biological effects on the nervous system were assessed by acetylcholinesterase (AChE) inhibitory activity and microelectrode arrays (MEA). -

Auction Categories
2019 Goods & Services Auction Auction Categories 100s Live Auction Page 27 200s Want to Get Away? Page 31 300s Eat, Drink and Be Merry Page 32 400s For Touro Eyes Only Page 35 500s Got Game? Page 40 600s Family Fun Zone Page 43 700s …And All the Rest Page 45 26 2019 Goods & Services Auction Live Auction Lot 100 New York, New York Lenny Feld, Linda Weissman, Marc MacNaughton This is how you’re supposed to do New York City! Start with two premier tickets to a top Broadway show. Then, dine at the Three-Star Michelin restaurant, Le Bernardin, where your $300 gift certificate will allow you to explore the delicious flavors of Executive Chef Eric Ripert! When you’re stuffed with all the gourmet seafood you can eat, collapse in your room at the European-style boutique Michelangelo Hotel ($300 gift certificate). Value: $1,000 Minimum Bid: $450 Lot 101 Sweet Baby James Provost Patricia Salkin and Howard Gross You've got a friend! On July 3, 2019 you and a friend will join Provost Patricia Salkin and her husband Howard Gross to see James Taylor perform from your "shed" seats at Tanglewood, home of the Boston Symphony Orchestra, in the Berkshires, MA. In addition to an overnight stay at Partricia Salkin's home, enjoy an unforgettable Tanglewood picnic dinner. Value: Priceless Minimum Bid: $300 Lot 102 What Happens In Vegas…. Jack Grossman '88 Go all in - this is no bluff! Enjoy a 5 night stay at a studio condo in the Trump Hotel Las Vegas (sleeps 2).