Interaction Between Hydrogen Sulfide, Nitric Oxide, and Carbon Monoxide Pathways in the Bovine Isolated Retina
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hydrogen Sulfide Public Health Statement
PUBLIC HEALTH STATEMENT Hydrogen Sulfide Division of Toxicology and Human Health Sciences December 2016 This Public Health Statement summarizes what is known about hydrogen sulfide such as possible health effects from exposure and what you can do to limit exposure. The U.S. Environmental Protection Agency (EPA) identifies the most serious hazardous waste sites in the nation. These sites make up the National Priorities List (NPL) and are sites targeted for long-term federal clean-up activities. U.S. EPA has found hydrogen sulfide in at least 34 of the 1,832 current or former NPL sites. The total number of NPL sites evaluated for hydrogen sulfide is not known. But the possibility remains that as more sites are evaluated, the sites at which hydrogen sulfide is found may increase. This information is important because these future sites may be sources of exposure, and exposure to hydrogen sulfide may be harmful. If you are exposed to hydrogen sulfide, many factors determine whether you’ll be harmed. These include how much you are exposed to (dose), how long you are exposed (duration), and how you are exposed (route of exposure). You must also consider the other chemicals you are exposed to and your age, sex, diet, family traits, lifestyle, and state of health. WHAT IS HYDROGEN SULFIDE? Hydrogen sulfide (H2S) is a flammable, colorless gas that smells like rotten eggs. People usually can smell hydrogen sulfide at low concentrations in air, ranging from 0.0005 to 0.3 parts hydrogen sulfide per million parts of air (ppm). At high concentrations, a person might lose their ability to smell it. -

H2CS) and Its Thiohydroxycarbene Isomer (HCSH
A chemical dynamics study on the gas phase formation of thioformaldehyde (H2CS) and its thiohydroxycarbene isomer (HCSH) Srinivas Doddipatlaa, Chao Hea, Ralf I. Kaisera,1, Yuheng Luoa, Rui Suna,1, Galiya R. Galimovab, Alexander M. Mebelb,1, and Tom J. Millarc,1 aDepartment of Chemistry, University of Hawai’iatManoa, Honolulu, HI 96822; bDepartment of Chemistry and Biochemistry, Florida International University, Miami, FL 33199; and cSchool of Mathematics and Physics, Queen’s University Belfast, Belfast BT7 1NN, Northern Ireland, United Kingdom Edited by Stephen J. Benkovic, The Pennsylvania State University, University Park, PA, and approved August 4, 2020 (received for review March 13, 2020) Complex organosulfur molecules are ubiquitous in interstellar molecular sulfur dioxide (SO2) (21) and sulfur (S8) (22). The second phase clouds, but their fundamental formation mechanisms have remained commences with the formation of the central protostars. Tempera- largely elusive. These processes are of critical importance in initiating a tures increase up to 300 K, and sublimation of the (sulfur-bearing) series of elementary chemical reactions, leading eventually to organo- molecules from the grains takes over (20). The subsequent gas-phase sulfur molecules—among them potential precursors to iron-sulfide chemistry exploits complex reaction networks of ion–molecule and grains and to astrobiologically important molecules, such as the amino neutral–neutral reactions (17) with models postulating that the very acid cysteine. Here, we reveal through laboratory experiments, first sulfur–carbon bonds are formed via reactions involving methyl electronic-structure theory, quasi-classical trajectory studies, and astro- radicals (CH3)andcarbene(CH2) with atomic sulfur (S) leading to chemical modeling that the organosulfur chemistry can be initiated in carbonyl monosulfide and thioformaldehyde, respectively (18). -
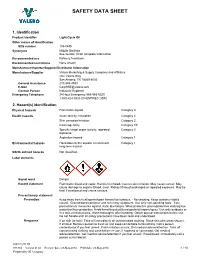
Safety Data Sheet
SAFETY DATA SHEET 1. Identification Product identifier Light Cycle Oil Other means of identification SDS number 106-GHS Synonyms Middle Distillate See section 16 for complete information. Recommended use Refinery feedstock. Recommended restrictions None known. Manufacturer/Importer/Supplier/Distributor information Manufacturer/Supplier Valero Marketing & Supply Company and Affiliates One Valero Way San Antonio, TX 78269-6000 General Assistance 210-345-4593 E-Mail [email protected] Contact Person Industrial Hygienist Emergency Telephone 24 Hour Emergency 866-565-5220 1-800-424-9300 (CHEMTREC USA) 2. Hazard(s) identification Physical hazards Flammable liquids Category 3 Health hazards Acute toxicity, inhalation Category 4 Skin corrosion/irritation Category 2 Carcinogenicity Category 1B Specific target organ toxicity, repeated Category 2 exposure Aspiration hazard Category 1 Environmental hazards Hazardous to the aquatic environment, Category 1 long-term hazard OSHA defined hazards Not classified. Label elements Signal word Danger Hazard statement Flammable liquid and vapor. Harmful if inhaled. Causes skin irritation. May cause cancer. May cause damage to organs (Blood, Liver, Kidney) through prolonged or repeated exposure. May be fatal if swallowed and enters airways. Precautionary statement Prevention Keep away from heat/sparks/open flames/hot surfaces. - No smoking. Keep container tightly closed. Ground/bond container and receiving equipment. Use only non-sparking tools. Take precautionary measures against static discharges. Wear protective gloves/protective clothing/eye protection/face protection. Avoid breathing dust/fume/gas/mist/vapors/spray. Use only outdoors or in a well-ventilated area. Wash thoroughly after handling. Obtain special instructions before use. Do not handle until all safety precautions have been read and understood. -

Exploring the Potential of Nitric Oxide and Hydrogen Sulfide (NOSH)
City University of New York (CUNY) CUNY Academic Works Publications and Research City College of New York 2020 Exploring the Potential of Nitric Oxide and Hydrogen Sulfide (NOSH)-Releasing Synthetic Compounds as Novel Priming Agents against Drought Stress in Medicago sativa Plants Chrystalla Antoniou Cyprus University of Technology Rafaella Xenofontos Cyprus University of Technology Giannis Chatzimichail Cyprus University of Technology Anastasis Christou Agricultural Research Institute Khosrow Kashfi CUNY City College See next page for additional authors How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/cc_pubs/777 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] Authors Chrystalla Antoniou, Rafaella Xenofontos, Giannis Chatzimichail, Anastasis Christou, Khosrow Kashfi, and Vasileios Fotopoulos This article is available at CUNY Academic Works: https://academicworks.cuny.edu/cc_pubs/777 biomolecules Article Exploring the Potential of Nitric Oxide and Hydrogen Sulfide (NOSH)-Releasing Synthetic Compounds as Novel Priming Agents against Drought Stress in Medicago sativa Plants Chrystalla Antoniou 1, Rafaella Xenofontos 1, Giannis Chatzimichail 1, Anastasis Christou 2, Khosrow Kashfi 3,4 and Vasileios Fotopoulos 1,* 1 Department of Agricultural Sciences, Biotechnology and Food Science, Cyprus University of Technology, 3603 Lemesos, Cyprus; [email protected] -

Hydrogen Sulfide Fact Sheet
Hydrogen Sulfide Fact Sheet What is hydrogen sulfide? Hydrogen sulfide (H 2S) occurs naturally in crude petroleum, natural gas, volcanic gases, and hot springs. It can also result from bacterial breakdown of organic matter. It is also produced by human and animal wastes. Bacteria found in your mouth and gastrointestinal tract produce hydrogen sulfide from bacteria decomposing materials that contain vegetable or animal proteins. Hydrogen sulfide can also result from industrial activities, such as food processing, coke ovens, kraft paper mills, tanneries, and petroleum refineries. Hydrogen sulfide is a flammable, colorless gas with a characteristic odor of rotten eggs. It is commonly known as hydrosulfuric acid, sewer gas, and stink damp. People can smell it at low levels. What happens to hydrogen sulfide when it enters the environment? • Hydrogen sulfide is released primarily as a gas and spreads in the air. • Hydrogen sulfide remains in the atmosphere for about 18 hours. • When released as a gas, it will change into sulfur dioxide and sulfuric acid. • In some instances, it may be released as a liquid waste from an industrial facility. How might I be exposed to hydrogen sulfide? • You may be exposed to hydrogen sulfide from breathing contaminated air or drinking contaminated water. • Individuals living near a wastewater treatment plant, a gas and oil drilling operation, a farm with manure storage or livestock confinement facilities, or a landfill may be exposed to higher levels of hydrogen sulfide. • You can be exposed at work if you work in the rayon textiles, petroleum and natural gas drilling and refining, or wastewater treatment industries. -

Hydrogen Sulfide and Nitric Oxide Are Mutually Dependent in The
Hydrogen sulfide and nitric oxide are mutually SEE COMMENTARY dependent in the regulation of angiogenesis and endothelium-dependent vasorelaxation Ciro Colettaa, Andreas Papapetropoulosa,b, Katalin Erdelyia, Gabor Olaha, Katalin Módisa, Panagiotis Panopoulosb, Antonia Asimakopouloub, Domokos Geröa, Iraida Sharinac, Emil Martinc, and Csaba Szaboa,1 aDepartment of Anesthesiology, University of Texas Medical Branch and Shriners Burns Hospital for Children, Galveston, TX 77555; bLaboratory of Molecular Pharmacology, Department of Pharmacy, University of Patras, 26504 Patras, Greece; and cDivision of Cardiology, Department of Internal Medicine, University of Texas Medical School at Houston, Houston, TX 77030 Edited by Solomon H. Snyder, The Johns Hopkins University School of Medicine, Baltimore, MD, and approved April 10, 2012 (received for review February 17, 2012) fi Hydrogen sulfide (H2S) is a unique gasotransmitter, with regula- of vascular tone and have signi cant implications for the patho- tory roles in the cardiovascular, nervous, and immune systems. genetic and therapeutic roles of both NO and H2S. Some of the vascular actions of H2S (stimulation of angiogenesis, relaxation of vascular smooth muscle) resemble those of nitric Results oxide (NO). Although it was generally assumed that H2S and NO H2S-Induced Angiogenesis Requires NO Biosynthesis. H2S resulted in exert their effects via separate pathways, the results of the current a concentration-dependent increase in bEnd3 microvascular en- A B study show that H2S and NO are mutually required to elicit angio- dothelial cell proliferation (Fig. S1 ) and migration (Fig. S1 and C), as well as microvessel sprouting from rat aortic rings (Fig. genesis and vasodilatation. Exposure of endothelial cells to H2S D increases intracellular cyclic guanosine 5′-monophosphate (cGMP) S1 ). -

Hydrogen Sulfide Capture: from Absorption in Polar Liquids to Oxide
Review pubs.acs.org/CR Hydrogen Sulfide Capture: From Absorption in Polar Liquids to Oxide, Zeolite, and Metal−Organic Framework Adsorbents and Membranes Mansi S. Shah,† Michael Tsapatsis,† and J. Ilja Siepmann*,†,‡ † Department of Chemical Engineering and Materials Science, University of Minnesota, 421 Washington Avenue SE, Minneapolis, Minnesota 55455-0132, United States ‡ Department of Chemistry and Chemical Theory Center, University of Minnesota, 207 Pleasant Street SE, Minneapolis, Minnesota 55455-0431, United States ABSTRACT: Hydrogen sulfide removal is a long-standing economic and environ- mental challenge faced by the oil and gas industries. H2S separation processes using reactive and non-reactive absorption and adsorption, membranes, and cryogenic distillation are reviewed. A detailed discussion is presented on new developments in adsorbents, such as ionic liquids, metal oxides, metals, metal−organic frameworks, zeolites, carbon-based materials, and composite materials; and membrane technologies for H2S removal. This Review attempts to exhaustively compile the existing literature on sour gas sweetening and to identify promising areas for future developments in the field. CONTENTS 4.1. Polymeric Membranes 9785 4.2. Membranes for Gas−Liquid Contact 9786 1. Introduction 9755 4.3. Ceramic Membranes 9789 2. Absorption 9758 4.4. Carbon-Based Membranes 9789 2.1. Alkanolamines 9758 4.5. Composite Membranes 9790 2.2. Methanol 9758 N 5. Cryogenic Distillation 9790 2.3. -Methyl-2-pyrrolidone 9758 6. Outlook and Perspectives 9791 2.4. Poly(ethylene glycol) Dimethyl Ether 9759 Author Information 9792 2.5. Sulfolane and Diisopropanolamine 9759 Corresponding Author 9792 2.6. Ionic Liquids 9759 ORCID 9792 3. Adsorption 9762 Notes 9792 3.1. -

Fact Sheet: Hydrogen Sulfide from Landfills
Fact Sheet: Hydrogen Sulfide from Landfills How might I be exposed to hydrogen sulfide from a landfill? Hydrogen sulfide is a flammable, colorless gas with a characteristic odor of rotten eggs. It is heavier than air and is commonly known as hydrosulfuric acid, sewer gas, and stink damp. Hydrogen sulfide occurs both naturally and from industrial processes. Hydrogen sulfide can be released from landfills and people living near landfills may be exposed to it by breathing it in. How can hydrogen sulfide affect my health? Exposure to low concentrations within the range of 30 parts of hydrogen sulfide in one billion parts of air (ppb) may cause irritation to the eyes, nose, or throat. It may also cause difficulty breathing for some individuals with respiratory problems, such as asthmatics. DOH uses the Minimal Risk Levels (MRLs) developed by the federal Agency for Toxic Substances and Disease Registry (ATSDR) to assess the possibility of non-cancer health effects. An MRL is an estimate of the daily human exposure to a hazardous substance, at or below which, that substance is unlikely to pose a measurable risk of adverse, non-cancer health effects. These particular values have many safety factors built in and the actual levels where health effects would be observed are much higher. The acute MRL, which represents short time periods of exposure (less than 15 days), is 70 ppb. Per the study that established this acute MRL, it should be noted that the actual level where health effects (respiratory problems and headaches) were observed was 2,000 ppb. The intermediate MRL is defined for exposure periods of 15 to 365 days. -

Methane and Hydrogen Sulfide Combustion
ineering ng & E P l r a o c i c e m s e s Journal of h T C e f c h o Gargurevich, J Chem Eng Process Technol 2016, 7:1 l ISSN: 2157-7048 n a o n l o r g u y o J Chemical Engineering & Process Technology DOI: 10.4172/2157-7048.1000280 ReviewResearch Article Article OpenOpen Access Access Chemical Kinetics Illustrations: Methane and Hydrogen Sulfide Combustion Ivan A Gargurevich* Chemical Engineering Consultant, Combustion and Process Technologies, 32593 Cedar Spring Court, Wildomar, CA 92595, USA Abstract Methane combustion has to be one of the most studied systems but nevertheless because of the dependence of many of the rates of elementary reactions in the mechanism on pressure and temperature (unimolecular or chemically activated reactions) as well as combustion conditions, fuel-rich or lean, discrepancies can always be found between two close but different combustion mechanisms authored by different investigators(both in the kinetic coefficients of reactions as well as the results of modeling). Nevertheless, the major chemical pathways are well known. Keywords: Chemical reaction; Chemical kinetics combustion carbon dioxide. CO + OH < = = > CO + H Introduction 2 As mentioned above the formation of C intermediates is an Methane combustion model assembly 2 important event in fuel-rich flames. Methyl radical again plays an In this section an attempt will made to present the approach to important role, developing the major features for the combustion of methane based on CH + CH + M < = = C H + M the concepts presented in previous chapters. The starting point is the 3 3 2 6 understanding that methane combustion involves (1) a chain reaction Then by a sequence of reactions involving the small radicals H, mechanism and (2) that its chemistry obeys the Hierarchical structure OH, O, and molecular Oxygen O2, ethane is broken down to C2H2 of Hydrocarbon combustion. -

Hydrogen Sulfide and Carbon Monoxide Tolerance in Bacteria
antioxidants Review Hydrogen Sulfide and Carbon Monoxide Tolerance in Bacteria Sofia S. Mendes †, Vanessa Miranda † and Lígia M. Saraiva *,† Instituto de Tecnologia Química e Biológica António Xavier, Universidade Nova de Lisboa, Avenida da República, 2780-157 Oeiras, Portugal; [email protected] (S.S.M.); [email protected] (V.M.) * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: Hydrogen sulfide and carbon monoxide share the ability to be beneficial or harmful molecules depending on the concentrations to which organisms are exposed. Interestingly, humans and some bacteria produce small amounts of these compounds. Since several publications have summarized the recent knowledge of its effects in humans, here we have chosen to focus on the role of H2S and CO on microbial physiology. We briefly review the current knowledge on how bacteria produce and use H2S and CO. We address their potential antimicrobial properties when used at higher concentrations, and describe how microbial systems detect and survive toxic levels of H2S and CO. Finally, we highlight their antimicrobial properties against human pathogens when endogenously produced by the host and when released by external chemical donors. Keywords: bacteria; hydrogen sulfide; carbon monoxide; CORMs 1. Introduction Citation: Mendes, S.S.; Miranda, V.; Hydrogen sulfide (H2S) and carbon monoxide (CO) are small molecules that are Saraiva, L.M. Hydrogen Sulfide and historically related with environmental industrial pollution. However, the two compounds Carbon Monoxide Tolerance in have long been recognized as also being produced by mammalian and bacterial cells in Bacteria. Antioxidants 2021, 10, 729. low amounts that mediate important physiological processes [1,2]. -

Co-Treatment of Hydrogen Sulfide and Methanol in a Single-Stage Biotrickling Filter Under Acidic Conditions
Co-treatment of hydrogen sulfide and methanol in a single-stage biotrickling filter under acidic conditions Yaomin Jin, María C. Veiga, Christian Kennes Chemosphere Volume 68, Issue 6, June 2007, Pages 1186–1193 DOI: 10.1016/j.chemosphere.2007.01.069 Abstract Biofiltration of waste gases is cost-effective and environment-friendly compared to the conventional techniques for treating large flow rates of gas streams with low concentrations of pollutants. Pulp and paper industry off-gases usually contain reduced sulfur compounds, such as hydrogen sulfide and a wide range of volatile organic compounds (VOCs), e.g., methanol. It is desirable to eliminate both of these groups of compounds. Since the co-treatment of inorganic sulfur compounds and VOCs in biotrickling filters is a relatively unexplored area, the simultaneous biotreatment of H2S and methanol as the model VOC was investigated. The results showed that, after −3 −1 adaptation, the elimination capacity of methanol could reach around 236 g m h with the simultaneous complete removal (100%) of 12 ppm H2S when the empty bed residence time is 24 s. The pH of the system was around 2. Methanol removal was hardly affected by the presence of hydrogen sulfide, despite the low pH. Conversely, the presence of the VOC in the waste gas reduced the efficiency of H2S biodegradation. The maximal methanol removal decreased somewhat when increasing the gas flow rate. This is the first report on the degradation of methanol at such low pH in a biotrickling filter and on the co-treatment of H2S and VOCs under such conditions. Keywords Acidophiles; pH; Fungi; Substrate competition; Oxygen limitation 1. -

The Effects of Hydrogen, Hydrogen Sulfide, and Ammonia on the Exzatated Temperature Detekcomtion of Metals and Algoys in Carbonaceous Gas Environments
THE EFFECTS OF HYDROGEN, HYDROGEN SULFIDE, AND AMMONIA ON THE EXZATATED TEMPERATURE DETEKCOMTION OF METALS AND ALGOYS IN CARBONACEOUS GAS ENVIRONMENTS A THESIS Presented to The Faculty of the Graduate Division by Harry Marshall Thron , Jr . In Partial F'ulfillment of the Requirement:; for the Degree Master of Science in Metallurgy I iiiI2 Georgia Institute of Technology September, 1968 In presenting the dissertation as a partial fulfillment of the requirements for an advanced d.egree from the Georgia Institute of Technology, I agree that the Library of the Institute shall make it available for inspection and circulation in accordance with its regulations governing materials of this type. I agree that permission to copy from, or to publish from, this dissertation may be granted. by the professor under whose direction it.was written, or, in his absence, by the Dean of the Graduate Division when such copying or publication is solely for scholarly purposes and. does not involve potential financial gain. It is under- stood that any copying from, or publication of, this dis- sertation which involves potential financial gain will not be allowed without written permission. THE EFFECTS OF HYDROGEN, HYDROGEN SULFIDE, AND AMMONIA ON THE ELEVATED TEMPER11TURE DETERIORATION OF METALS AND ,ALLOYS IN CARBONACEOUS GAS IDJVIRONMENTS Approved: A Date approved by Chairman: 11/15/68 I would like to express appreciation to my faculty advisor, Dr. R. F. Hochtmn, and to my reading co&tt.ee, Dr. N. N. Engel and Dr, H. V. Grubb, for their assistance and suggestions. My sincere appreciation is extended to Texaco, Incorporated, for the provision of a Research Fellowship and to Mr.