Evaluation of TGFBI Corneal Dystrophy and Molecular Diagnostic Testing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(TGFBI) Function and Paclitaxel Response in Ovarian Cancer Cells David a Tumbarello1,2, Jillian Temple1 and James D Brenton1*
Tumbarello et al. Molecular Cancer 2012, 11:36 http://www.molecular-cancer.com/content/11/1/36 RESEARCH Open Access β3 integrin modulates transforming growth factor beta induced (TGFBI) function and paclitaxel response in ovarian cancer cells David A Tumbarello1,2, Jillian Temple1 and James D Brenton1* Abstract Background: The extracellular matrix (ECM) has a key role in facilitating the progression of ovarian cancer and we have shown recently that the secreted ECM protein TGFBI modulates the response of ovarian cancer to paclitaxel-induced cell death. Results: We have determined TGFBI signaling from the extracellular environment is preferential for the cell surface αvβ3 integrin heterodimer, in contrast to periostin, a TGFBI paralogue, which signals primarily via a β1 integrin-mediated pathway. We demonstrate that suppression of β1 integrin expression, in β3 integrin-expressing ovarian cancer cells, increases adhesion to rTGFBI. In addition, Syndecan-1 and −4 expression is dispensable for adhesion to rTGFBI and loss of Syndecan-1 cooperates with the loss of β1 integrin to further enhance adhesion to rTGFBI. The RGD motif present in the carboxy-terminus of TGFBI is necessary, but not sufficient, for SKOV3 cell adhesion and is dispensable for adhesion of ovarian cancer cells lacking β3 integrin expression. In contrast to TGFBI, the carboxy-terminus of periostin, lacking a RGD motif, is unable to support adhesion of ovarian cancer cells. Suppression of β3 integrin in SKOV3 cells increases resistance to paclitaxel-induced cell death while suppression of β1 integrin has no effect. Furthermore, suppression of TGFBI expression stimulates a paclitaxel resistant phenotype while suppression of fibronectin expression, which primarily signals through a β1 integrin-mediated pathway, increases paclitaxel sensitivity. -

Datasheet: VPA00676 Product Details
Datasheet: VPA00676 Description: RABBIT ANTI TGFBI Specificity: TGFBI Format: Purified Product Type: PrecisionAb™ Polyclonal Isotype: Polyclonal IgG Quantity: 100 µl Product Details Applications This product has been reported to work in the following applications. This information is derived from testing within our laboratories, peer-reviewed publications or personal communications from the originators. Please refer to references indicated for further information. For general protocol recommendations, please visit www.bio-rad-antibodies.com/protocols. Yes No Not Determined Suggested Dilution Western Blotting 1/1000 PrecisionAb antibodies have been extensively validated for the western blot application. The antibody has been validated at the suggested dilution. Where this product has not been tested for use in a particular technique this does not necessarily exclude its use in such procedures. Further optimization may be required dependant on sample type. Target Species Human Product Form Purified IgG - liquid Preparation Rabbit polyclonal antibody purified by affinity chromatography Buffer Solution Phosphate buffered saline Preservative 0.01% Thiomersal Stabilisers 1% Bovine Serum Albumin <50% Glycerol Immunogen Recombinant protein encompassing part of the middle region of human TGFBI External Database Links UniProt: Q15582 Related reagents Entrez Gene: 7045 TGFBI Related reagents Synonyms BIGH3 Specificity Rabbit anti Human TGFBI antibody recognizes the transforming growth factor-beta-induced protein ig-h3, also known as RGD-containing collagen-associated protein (RGD-CAP), beta ig-h3, Page 1 of 2 kerato-epithelin or transforming growth factor, beta-induced 68 kDa. TGFBI gene encodes an RGD-containing protein that binds to type I, II and IV collagens. The RGD motif is found in many extracellular matrix proteins modulating cell adhesion and serves as a ligand recognition sequence for several integrins. -

Supplementary Figures and Tables
SUPPLEMENTARY DATA Supplementary Figure 1. Isolation and culture of endothelial cells from surgical specimens of FVM. (A) Representative pre-surgical fundus photograph of a right eye exhibiting a FVM encroaching on the optic nerve (dashed line) causing tractional retinal detachment with blot hemorrhages throughout retina (arrow heads). (B) Magnetic beads (arrows) allow for separation and culturing of enriched cell populations from surgical specimens (scale bar = 100 μm). (C) Cultures of isolated cells stained positively for CD31 representing a successfully isolated enriched population (scale bar = 40 μm). ©2017 American Diabetes Association. Published online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db16-1035/-/DC1 SUPPLEMENTARY DATA Supplementary Figure 2. Efficient siRNA knockdown of RUNX1 expression and function demonstrated by qRT-PCR, Western Blot, and scratch assay. (A) RUNX1 siRNA induced a 60% reduction of RUNX1 expression measured by qRT-PCR 48 hrs post-transfection whereas expression of RUNX2 and RUNX3, the two other mammalian RUNX orthologues, showed no significant changes, indicating specificity of our siRNA. Functional inhibition of Runx1 signaling was demonstrated by a 330% increase in insulin-like growth factor binding protein-3 (IGFBP3) RNA expression level, a known target of RUNX1 inhibition. Western blot demonstrated similar reduction in protein levels. (B) siRNA- 2’s effect on RUNX1 was validated by qRT-PCR and western blot, demonstrating a similar reduction in both RNA and protein. Scratch assay demonstrates functional inhibition of RUNX1 by siRNA-2. ns: not significant, * p < 0.05, *** p < 0.001 ©2017 American Diabetes Association. Published online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db16-1035/-/DC1 SUPPLEMENTARY DATA Supplementary Table 1. -

DF7015-TGFBI Antibody
Affinity Biosciences website:www.affbiotech.com order:[email protected] TGFBI Antibody Cat.#: DF7015 Concn.: 1mg/ml Mol.Wt.: 68kDa Size: 100ul,200ul Source: Rabbit Clonality: Polyclonal Application: WB 1:500-1:2000, IHC 1:50-1:200, IF/ICC 1:100-1:500, ELISA(peptide) 1:20000-1:40000 *The optimal dilutions should be determined by the end user. Reactivity: Human,Mouse,Rat Purification: The antiserum was purified by peptide affinity chromatography using SulfoLink™ Coupling Resin (Thermo Fisher Scientific). Specificity: TGFBI Antibody detects endogenous levels of total TGFBI. Immunogen: A synthesized peptide derived from human TGFBI, corresponding to a region within N-terminal amino acids. Uniprot: Q15582 Description: TGFBI is a RGD-containing protein that binds to type I, II and IV collagens. The RGD motif is found in many extracellular matrix proteins modulating cell adhesion and serves as a ligand recognition sequence for several integrins. TGFBI plays a role in cell-collagen interactions and may be involved in endochondrial bone formation in cartilage. TGFBI is induced by transforming growth factor-beta and acts to inhibit cell adhesion. Storage Condition and Rabbit IgG in phosphate buffered saline , pH 7.4, 150mM Buffer: NaCl, 0.02% sodium azide and 50% glycerol.Store at -20 °C.Stable for 12 months from date of receipt. Western blot analysis of extracts from MCF7, using TGFBI Antibody. The lane on the left was treated with blocking peptide. 1 / 2 Affinity Biosciences website:www.affbiotech.com order:[email protected] Western blot analysis of Hela cell lysates, using TGFBI Antibody. The lane on the left was treated with the antigen- specific peptide. -
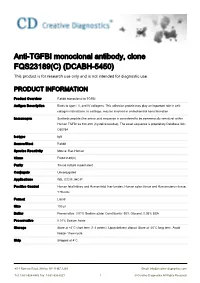
Anti-TGFBI Monoclonal Antibody, Clone FQS23189(C) (DCABH-5450) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-TGFBI monoclonal antibody, clone FQS23189(C) (DCABH-5450) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Rabbit monoclonal to TGFBI Antigen Description Binds to type I, II, and IV collagens. This adhesion protein may play an important role in cell- collagen interactions. In cartilage, may be involved in endochondral bone formation. Immunogen Synthetic peptide (the amino acid sequence is considered to be commercially sensitive) within Human TGFBI aa 100-200 (Cysteine residue). The exact sequence is proprietary.Database link: O60784 Isotype IgG Source/Host Rabbit Species Reactivity Mouse, Rat, Human Clone FQS23189(C) Purity Tissue culture supernatant Conjugate Unconjugated Applications WB, ICC/IF, IHC-P Positive Control Human fetal kidney and Human fetal liver lysates, Human colon tissue and Human uterus tissue, Y79 cells Format Liquid Size 100 μl Buffer Preservative: 0.01% Sodium azide; Constituents: 50% Glycerol, 0.05% BSA Preservative 0.01% Sodium Azide Storage Store at +4°C short term (1-2 weeks). Upon delivery aliquot. Store at -20°C long term. Avoid freeze / thaw cycle. Ship Shipped at 4°C. 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved GENE INFORMATION Gene Name TGFBI transforming growth factor, beta-induced, 68kDa [ Homo sapiens ] Official Symbol TGFBI Synonyms TGFBI; transforming growth factor, beta-induced, 68kDa; CSD1, CSD2, CSD3, LCD1, transforming -

The Effects of Genetic Variants on Protein Structure and Their Associations with Preeclampsia
The Effects of Genetic Variants on Protein Structure and their Associations with Preeclampsia Elizabeth Geena Woo Undergraduate Honors Thesis April 20, 2020 Thesis Advisor: Alper Uzun, PhD Second Reader: James Padbury, MD A thesis submitted in partial fulfillment for the degree of Bachelor of Arts With Honors in Computational Biology 1 Table of Contents Introduction......................................................................................................................................3 Methods and Materials.....................................................................................................................4 Results and Discussion....................................................................................................................8 Conclusion.....................................................................................................................................28 References......................................................................................................................................32 2 Introduction Preeclampsia is a complex pregnancy-specific disorder characterized by the onset of maternal hypertension and proteinuria.1,2 This multifactorial disorder complicates 2-8% of US deliveries and is a major cause of maternal and fetal morbidity and mortality.3 Preeclamptic pregnancies are associated with long-term outcomes for both the mother and offspring. Stroke, cardiovascular disease, diabetes, and premature mortality are linked to preeclampsia in affected mothers -

The Proteins of Keratoconus: a Literature Review Exploring Their Contribution to the Pathophysiology of the Disease
Adv Ther (2019) 36:2205–2222 https://doi.org/10.1007/s12325-019-01026-0 REVIEW The Proteins of Keratoconus: a Literature Review Exploring Their Contribution to the Pathophysiology of the Disease Eleftherios Loukovitis . Nikolaos Kozeis . Zisis Gatzioufas . Athina Kozei . Eleni Tsotridou . Maria Stoila . Spyros Koronis . Konstantinos Sfakianakis . Paris Tranos . Miltiadis Balidis . Zacharias Zachariadis . Dimitrios G. Mikropoulos . George Anogeianakis . Andreas Katsanos . Anastasios G. Konstas Received: June 11, 2019 / Published online: July 30, 2019 Ó The Author(s) 2019 ABSTRACT abnormalities primarily relate to the weakening of the corneal collagen. Their understanding is Introduction: Keratoconus (KC) is a complex, crucial and could contribute to effective man- genetically heterogeneous multifactorial agement of the disease, such as with the aid of degenerative disorder characterized by corneal corneal cross-linking (CXL). The present article ectasia and thinning. Its incidence is approxi- critically reviews the proteins involved in the mately 1/2000–1/50,000 in the general popula- pathophysiology of KC, with particular tion. KC is associated with moderate to high emphasis on the characteristics of collagen that myopia and irregular astigmatism, resulting in pertain to CXL. severe visual impairment. KC structural Methods: PubMed, MEDLINE, Google Scholar and GeneCards databases were screened for rel- evant articles published in English between January 2006 and June 2018. Keyword combi- Enhanced Digital Features To view enhanced digital nations of the words ‘‘keratoconus,’’ ‘‘risk features for this article go to https://doi.org/10.6084/ m9.figshare.8427200. E. Loukovitis K. Sfakianakis Hellenic Army Medical Corps, Thessaloniki, Greece Division of Surgical Anatomy, Laboratory of Anatomy, Medical School, Democritus University of E. -

Dysregulation of the Mir-449B Target TGFBI Alters the Tgfβ Pathway to Induce Cisplatin Resistance in Nasopharyngeal Carcinoma Pierre-Antoine Bissey1, Jacqueline H
Bissey et al. Oncogenesis (2018) 7:40 DOI 10.1038/s41389-018-0050-x Oncogenesis ARTICLE Open Access Dysregulation of the MiR-449b target TGFBI alters the TGFβ pathway to induce cisplatin resistance in nasopharyngeal carcinoma Pierre-Antoine Bissey1, Jacqueline H. Law2,JeffP.Bruce1,WeiShi1, Aline Renoult3,MelvinL.K.Chua 1,4,5,6, Kenneth W. Yip1 and Fei-Fei Liu1,2,4 Abstract Despite the improvement in locoregional control of nasopharyngeal carcinoma (NPC), distant metastasis (DM), and chemoresistance persist as major causes of mortality. This study identified a novel role for miR-449b, an overexpressed gene in a validated four-miRNA signature for NPC DM, leading to chemoresistance via the direct targeting of transforming growth factor beta-induced (TGFBI). In vitro shRNA-mediated downregulation of TGFBI induced phosphorylation of PTEN and AKT, increasing cisplatin resistance. Conversely, the overexpression of TGFBI sensitized the NPC cells to cisplatin. In NPC patients treated with concurrent chemoradiotherapy (CRT), the overall survival (OS) was significantly inversely correlated with miR-449b, and directly correlated with both TGFBI mRNA and protein expression, as assessed by RNA sequencing and immunohistochemistry (IHC). Mechanistically, co- immunoprecipitation demonstrated that TGFBI competes with pro-TGFβ1 for integrin receptor binding. Decreased TGFBI led to increased pro-TGFβ1 activation and TGFβ1 canonical/noncanonical pathway-induced cisplatin resistance. Thus, overexpression of miR-449b decreases TGFBI, thereby altering the balance between TGFBI and pro-TGFβ1, 1234567890():,; 1234567890():,; revealing a novel mechanism of chemoresistance in NPC. Introduction remains a major clinical challenge7. Concurrent cisplatin Nasopharyngeal carcinoma (NPC) is an Epstein–Barr or 5-fluorouracil chemotherapy in combination with RT virus (EBV)-associated malignancy1,2 that accounts for provides only a modest improvement in OS, yet causes – 87,000 new cases and 51,000 deaths annually3,4. -

Autosomal Dominant Corneal Dystrophy with TGFBI Mutations
ndrom Sy es tic & e G n e e n G e f T o Shu et al., J Genet Syndr Gene Ther 2015, 6:2 Journal of Genetic Syndromes h l e a r n a DOI: 10.4172/2157-7412.1000264 r p u y o J & Gene Therapy ISSN: 2157-7412 Research Article Open Access Autosomal Dominant Corneal Dystrophy with TGFBI Mutations: Lessons Learned from a Chinese Pedigree Anli Shu1, Zheng Wei2, Yibin Hao3, Hai Luo1, Fu Tian3, Fred G Biddle4, Wei Wu3,5, Min Liu3 and Wei Cao3* 1Hunan University of Medicine, Huaihua 418000, Hunan Province, China 2Department of Experimental Laboratory, General Hospital of Shenyang Military Area Command, Shengyang 110840, China 3Clinical Research Laboratory, Zhengzhou Central Hospital, Zhengzhou University, China 4Department of Medical Genetics and Department of Biological Sciences, University of Calgary, Canada 5Department of Pathology and Experimental Medicine, University of Calgary, Canada Abstract Corneal dystrophies are rare autosomal dominant genetic diseases with diverse anatomic classification. The complexity of this disease reflects both the heterogeneity of causative gene mutations and the diversity of clinical presentations. Here, we studied and report a four-generation Chinese pedigree with corneal dystrophy, in which the clinical symptoms resemble Meesmann corneal dystrophy without the characteristic gene mutations of either KRT3 or KRT12. Targeted exon sequencing with PCR methods identified an Arg124Cys mutation in the TGFBI gene that concordant with phenotype in all affected individuals. This TGFBI mutation has been associated with multiple subtypes of corneal dystrophy. We reviewed the global reported TGFBI mutations in different ethnic groups and geographically mapped TGFBI mutations previously reported in China. -

Extracellular Matrix Protein Ig-H3/TGFBI Promotes Metastasis of Colon Cancer by Enhancing Cell Extravasation
Downloaded from genesdev.cshlp.org on September 26, 2021 - Published by Cold Spring Harbor Laboratory Press Extracellular matrix protein ig-h3/TGFBI promotes metastasis of colon cancer by enhancing cell extravasation Chaoyu Ma,1 Yu Rong,1 Daniel R. Radiloff,1 Michael B. Datto,2 Barbara Centeno,3 Shideng Bao,4 Anthony Wai Ming Cheng,2 Fumin Lin,1 Shibo Jiang,5 Timothy J. Yeatman,3 and Xiao-Fan Wang1,6 1Department of Pharmacology and Cancer Biology, Duke University Medical Center, Durham, North Carolina 27710, USA; 2Department of Pathology, Duke University Medical Center, Durham, North Carolina 27710, USA; 3Department of Surgery, H. Lee Moffitt Cancer Center and Research Institute, Tampa, Florida 33612, USA; 4Department of Radiation Oncology and Department of Neurosurgery, University of Colorado at Denver and Health Science Center, Aurora, Colorado 80045, USA; 5Lindsley F. Kimball Research Institute, New York Blood Center, New York, New York 10021, USA Metastasis, the major cause of cancer death, is a multistep process that requires interactions between cancer cells and stromal cells and between cancer cells and extracellular matrix. Molecular alterations of the extracellular matrix in the tumor microenvironment have a considerable impact on the metastatic process during tumorigenesis. Here we report that elevated expression of ig-h3/TGFBI (transforming growth factor, -induced), an extracellular matrix protein secreted by colon cancer cells, is associated with high-grade human colon cancers. Ectopic expression of the ig-h3 protein enhanced the aggressiveness and altered the metastatic properties of colon cancer cells in vivo. Inhibition of ig-h3 expression dramatically reduced metastasis. Mechanistically, ig-h3 appears to promote extravasation, a critical step in the metastatic dissemination of cancer cells, by inducing the dissociation of VE-cadherin junctions between endothelial cells via activation of ␣   the integrin v 5–Src signaling pathway. -

Targeted Expression of Tgfbip Peptides in Mouse and Human Tissue by MALDI-Mass Spectrometry Imaging
separations Article Targeted Expression of TGFBIp Peptides in Mouse and Human Tissue by MALDI-Mass Spectrometry Imaging Venkatraman Anandalakshmi 1,†, Guillaume Hochart 2,†, David Bonnel 2, Jonathan Stauber 2, Shigeto Shimmura 3 , Rajamani Lakshminarayanan 1,4 , Konstantin Pervushin 5 and Jodhbir S. Mehta 1,4,6,* 1 Singapore Eye Research Institute, The Academia, 20 College Road, Level 6 Discovery Tower, Singapore 169856, Singapore; [email protected] (V.A.); [email protected] (R.L.) 2 ImaBiotech, Parc Eurasanté, 152 Rue Du Docteur Yersin, 59120 Loos, France; [email protected] (G.H.); [email protected] (D.B.); [email protected] (J.S.) 3 Department of Ophthalmology, Keio University, 35 Shinanomachi, Tokyo 160-8582, Japan; [email protected] 4 Ophthalmology and Visual Sciences Academic Clinical Program, Duke-NUS Graduate Medical School, Singapore 169857, Singapore 5 School of Biological Sciences, Nanyang Technological University, Singapore 637551, Singapore; [email protected] 6 Singapore National Eye Centre, 11 Third Hospital Avenue, Singapore 168751, Singapore * Correspondence: [email protected]; Fax: +65-6225-2568 † Both authors (VA and GH) contributed equally towards the publication. Abstract: Stromal corneal dystrophies are a group of hereditary disorders caused by mutations in the TGFBI gene. The mutant TGFBIp is prone to protein aggregation and the mutant protein gets deposited in the cornea, leading to severe visual impairment. The mutations lead to a corneal Citation: Anandalakshmi, V.; specific protein aggregation suggesting the involvement of tissue-specific factors. The exact molecular Hochart, G.; Bonnel, D.; Stauber, J.; mechanism of the process of tissue-specific protein aggregation remains to be elucidated. -

Inhibitory Effect of Tranilast on Transforming Growth Factor-Beta-Induced Protein in Granular Corneal Dystrophy Type 2 Corneal Fibroblasts
BASIC INVESTIGATION Inhibitory Effect of Tranilast on Transforming Growth Factor-Beta-Induced Protein in Granular Corneal Dystrophy Type 2 Corneal Fibroblasts Tae-im Kim, MD, PhD,* Hun Lee, MD,* Hye Kyoung Hong, PhD,* Kyu Seo Kim, BS,† Seung-Il Choi, PhD,* Yong-Sun Maeng, PhD,* and Eung Kweon Kim, MD, PhD*‡ recurrence of corneal opacity in TGFBI-linked corneal dystrophies if Purpose: To investigate the effects of tranilast, an inhibitor of clinical studies confirm these findings. chemical mediators and fibroblast proliferation, on the expression of transforming growth factor-beta (TGF-b)-induced protein (TGFBIp) Key Words: tranilast, TGFBIp, TGF-b, pSmad, a-SMA, corneal in wild-type (WT) and homozygous (HO) granular corneal dystro- dystrophy fi phy type 2 corneal broblasts. (Cornea 2015;34:950–958) Methods: Cell proliferation and cytotoxicity were measured by Cell Counting Kit-8 and lactate dehydrogenase assay. Western blotting and real-time polymerase chain reaction were used to bnormal accumulation of extracellular matrix (ECM) determine changes in the expression of TGFBIp and TGFBI mRNA. Aproteins produced by activated or transformed corneal We determined the effects of tranilast on phosphorylated Smad2 fibroblasts is associated with loss of corneal transparency in (pSmad2) and pSmad3, wound-healing, and expression of alpha- corneal dystrophies. The extracellular transforming growth smooth muscle actin (a-SMA), type I collagen, and integrins. factor beta (TGF-b)-induced gene (TGFBI, formerly known as BIGH3), located on chromosome 5q31, is mutated in corneal Results: High concentrations of tranilast decreased proliferation of dystrophies.1–3 The TGFBI protein (TGFBIp) contains 4 tandem corneal fibroblasts but did not cause elevation of lactate dehydroge- repeats of the fasciclin I domain and an N-terminal cysteine-rich nase, except at 1.0 mM tranilast.