Patient Assessment and Vital Signs Measurement and Documentation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Respiratory Examination Cardiac Examination Is an Essential Part of the Respiratory Assessment and Vice Versa
Respiratory examination Cardiac examination is an essential part of the respiratory assessment and vice versa. # Subject steps Pictures Notes Preparation: Pre-exam Checklist: A Very important. WIPE Be the one. 1 Wash your hands. Wash your hands in Introduce yourself to the patient, confirm front of the examiner or bring a sanitizer with 2 patient’s ID, explain the examination & you. take consent. Positioning of the patient and his/her (Position the patient in a 3 1 2 Privacy. 90 degree sitting position) and uncover Exposure. full exposure of the trunk. his/her upper body. 4 (if you could not, tell the examiner from the beginning). 3 4 Examination: General appearance: B (ABC2DEVs) Appearance: young, middle aged, or old, Begin by observing the and looks generally ill or well. patient's general health from the end of the bed. Observe the patient's general appearance (age, Around the bed I can't state of health, nutritional status and any other see any medications, obvious signs e.g. jaundice, cyanosis, O2 mask, or chest dyspnea). 1 tube(look at the lateral sides of chest wall), metered dose inhalers, and the presence of a sputum mug. 2 Body built: normal, thin, or obese The patient looks comfortable and he doesn't appear short of breath and he doesn't obviously use accessory muscles or any heard Connections: such as nasal cannula wheezes. To determine this, check for: (mention the medications), nasogastric Dyspnea: Assess the rate, depth, and regularity of the patient's 3 tube, oxygen mask, canals or nebulizer, breathing by counting the respiratory rate, range (16–25 breaths Holter monitor, I.V. -

The Child with Altered Respiratory Status
Path: K:/LWW-BOWDEN-09-0101/Application/LWW-BOWDEN-09-0101-016.3d Date: 3rd July 2009 Time: 16:31 User ID: muralir 1BlackLining Disabled CHAPTER 16 The Child With Altered Respiratory Status Do you remember the Diaz fam- Case History leave Lela, the baby sister, ily from Chapter 9, in which with Claudia’s mother, Selma, Jose has trouble taking his asthma medication, and head to the hospital. and in Chapter 4, in which Jose’s little sister, At the hospital the emergency department Lela, expresses her personality even as a new- nurse observes Jose sitting cross-legged and born? Jose is 4 years old and was diagnosed leaning forward on his hands. His mouth is with asthma this past fall, about 6 months ago. open and he is breathing hard with an easily Since that time Claudia, his mother, has audible inspiratory wheeze. He is using his noticed several factors that trigger his asthma subclavicular accessory muscles with each including getting sick, pollen, and cold air. breath. His respiratory rate is 32 breaths per One evening following a warm early-spring minute, his pulse is 112 beats per minutes, day, Jose is outside playing as the sun sets and and he is afebrile. Claudia explains that he the air cools. When he comes inside he was fine; he was outside running and playing, begins to cough. Claudia sets up his nebulizer and then came in and began coughing and and gives him a treatment of albuterol, which wheezing, and she gave him an albuterol lessens his coughing. Within an hour, Jose is treatment. -

Breathing Sounds – Determination of Extremely Low Spl
MATEC Web of Conferences 217, 03001 (2018) https://doi.org/10.1051/matecconf/201821703001 ICVSSD 2018 BREATHING SOUNDS – DETERMINATION OF EXTREMELY LOW SPL M. Harun1*, R. Teoh Y. S1, M. ‘A. A. Ahmad, M. Mohd. Mokji1, You K. Y1, S. A. R. Syed Abu Bakar1, P. I. Khalid1, S. Z. Abd. Hamid1 and R. Arsat1 1 School of Electrical Engineering, Universiti Teknologi Malaysia, *Email: [email protected] Phone: +6075535358 ABSTRACT Breathing sound is an extremely low SPL that results from inspiration and expiration process in the lung. Breathing sound can be used to diagnose persons with complications with breathing. Also, the sound can indicate the effectiveness of treatment of lung disease such as asthma. The purpose of this study was to identify SPL of breathing sounds, over six one octave center frequencies from 63 Hz to 4000 Hz, from the recorded breathing sounds in .wav files. Breathing sounds of twenty participants with normal weight BMI had been recorded in an audiometry room. The breathing sound was acquired in two states: at rest and after a 300 meters walk. Matlab had been used to process the breathing sounds that are in .wav files to come up with SPL (in dB). It has been found out that the SPL of breathing sound of all participants are positive at frequencies 63 Hz and 125 Hz. On the other hand, the SPL are all negatives at frequency 1000 Hz, 2000 Hz and 4000 Hz. In conclusion, SPL of breathing sounds of the participants, at frequencies 250 Hz and 500 Hz that have both positive and negative values are viable to be studied further for physiological and medicinal clues. -

Practical Cardiac Auscultation
LWW/CCNQ LWWJ306-08 March 7, 2007 23:32 Char Count= Crit Care Nurs Q Vol. 30, No. 2, pp. 166–180 Copyright c 2007 Wolters Kluwer Health | Lippincott Williams & Wilkins Practical Cardiac Auscultation Daniel M. Shindler, MD, FACC This article focuses on the practical use of the stethoscope. The art of the cardiac physical exam- ination includes skillful auscultation. The article provides the author’s personal approach to the patient for the purpose of best hearing, recognizing, and interpreting heart sounds and murmurs. It should be used as a brief introduction to the art of auscultation. This article also attempts to illustrate heart sounds and murmurs by using words and letters to phonate the sounds, and by presenting practical clinical examples where auscultation clearly influences cardiac diagnosis and treatment. The clinical sections attempt to go beyond what is available in standard textbooks by providing information and stethoscope techniques that are valuable and useful at the bedside. Key words: auscultation, murmur, stethoscope HIS article focuses on the practical use mastered at the bedside. This article also at- T of the stethoscope. The art of the cardiac tempts to illustrate heart sounds and mur- physical examination includes skillful auscul- murs by using words and letters to phonate tation. Even in an era of advanced easily avail- the sounds, and by presenting practical clin- able technological bedside diagnostic tech- ical examples where auscultation clearly in- niques such as echocardiography, there is still fluences cardiac diagnosis and treatment. We an important role for the hands-on approach begin by discussing proper stethoscope selec- to the patient for the purpose of evaluat- tion and use. -

Mosby: Mosby's Nursing Video Skills
Mosby: Mosby's Nursing Video Skills Procedural Guideline for Assessing Apical Pulse Procedure Steps 1. Verify the health care provider’s orders. 2. Gather the necessary equipment and supplies. 3. Perform hand hygiene. 4. Provide for the patient’s privacy. 5. Introduce yourself to the patient and family if present. 6. Identify the patient using two identifiers. 7. Assess for factors that can affect the apical pulse rate and rhythm, such as medical history, disease processes, age, exercise, position changes, medications, temperature, or sympathetic stimulation. 8. Gloves are only worn if nurse will be in contact with bodily fluids or the patient is in protective precautions. 9. Help the patient into a supine or sitting position, and expose the sternum and the left side of the chest. 10. Locate the point of maximal impulse (PMI, or apical impulse). To do this, find the angle of Louis, which feels like a bony prominence just below the suprasternal notch. 11. Slide your fingers down each side of the angle to find the second intercostal space (ICS). Carefully move your fingers down the left side of the sternum to the fifth intercostal space and over to the left midclavicular line. 12. Feel the PMI as a light tap about 1 to 2 centimeters in diameter, reflecting the apex of the heart. 13. If the PMI is not where you would expect, as in a patient whose left ventricle is enlarged, inch your fingers along the fifth intercostal space until you feel the PMI. 14. Remember where you felt the PMI: over the apex of the heart in the fifth intercostal space at the left midclavicular line. -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -

Bradycardia; Pulse Present
Bradycardia; Pulse Present History Signs and Symptoms Differential • Past medical history • HR < 60/min with hypotension, acute • Acute myocardial infarction • Medications altered mental status, chest pain, • Hypoxia / Hypothermia • Beta-Blockers acute CHF, seizures, syncope, or • Pacemaker failure • Calcium channel blockers shock secondary to bradycardia • Sinus bradycardia • Clonidine • Chest pain • Head injury (elevated ICP) or Stroke • Digoxin • Respiratory distress • Spinal cord lesion • Pacemaker • Hypotension or Shock • Sick sinus syndrome • Altered mental status • AV blocks (1°, 2°, or 3°) • Syncope • Overdose Heart Rate < 60 / min and Symptomatic: Exit to Hypotension, Acute AMS, Ischemic Chest Pain, Appropriate NO Acute CHF, Seizures, Syncope, or Shock Protocol(s) secondary to bradycardia Typically HR < 50 / min YES Airway Protocol(s) AR 1, 2, 3 if indicated Respiratory Distress Reversible Causes Protocol AR 4 if indicated Hypovolemia Hypoxia Chest Pain: Cardiac and STEMI Section Cardiac Protocol Adult Protocol AC 4 Hydrogen ion (acidosis) if indicated Hypothermia Hypo / Hyperkalemia Search for Reversible Causes B Tension pneumothorax 12 Lead ECG Procedure Tamponade; cardiac Toxins Suspected Beta- IV / IO Protocol UP 6 Thrombosis; pulmonary Blocker or Calcium P Cardiac Monitor (PE) Channel Blocker Thrombosis; coronary (MI) A Follow Overdose/ Toxic Ingestion Protocol TE 7 P If No Improvement Transcutaneous Pacing Procedure P (Consider earlier in 2nd or 3rd AVB) Notify Destination or Contact Medical Control Revised AC 2 01/01/2021 Any local EMS System changes to this document must follow the NC OEMS Protocol Change Policy and be approved by OEMS 1 Bradycardia; Pulse Present Adult Cardiac Adult Section Protocol Pearls • Recommended Exam: Mental Status, HEENT, Skin, Heart, Lungs, Abdomen, Back, Extremities, Neuro • Identifying signs and symptoms of poor perfusion caused by bradycardia are paramount. -

Arrhythmia What Is It?
Arrhythmia What is it? Most of us have felt our heart race or skip a beat. It’s fairly normal every once and a while. But for some people, it’s a sign of arrhythmia – a disorder of your heart rate or rhythm – that needs to be checked out by a specialist. If you have an arrhythmia (there are multiple types), your heart either beats: • too fast • too slow or • with an irregular pattern Did You Know? This change in your heart rhythm is usually caused by a “glitch” Our heart beats an average of in your heart’s electrical activity, which tells the heart when to 70 to 80 times a minute and contract and pump blood to the body. Your heart doesn’t beat over 100,000 times a day! It’s with the regularity of a Swiss watch, and many factors can cause no wonder millions of people an irregularity. notice palpitations such as skipping a beat, fluttering or a Some of these factors include: racing heart. • having had a heart attack • having heart failure • blood chemistry imbalances • abnormal hormone levels • alcohol, caffeine and other substances or medicines • a variety of inherited abnormalities 8 Tips for Staying Heart Healthy with Arrhythmias Living with an arrhythmia varies tremendously from one person to the next. It will depend on the type of arrhythmia you have, how serious it is and the recommended treatment. Some people can take a single medication to correct their heart’s rhythm; others undergo electrophysiology studies or require a pacemaker or implantable defibrillator. No matter what kind of arrhythmia you have, there are things you can do to keep your heart healthy and ticking as it should. -

5 Precordial Pulsations
Chapter 5 / Precordial Pulsations 113 5 Precordial Pulsations CONTENTS MECHANICS AND PHYSIOLOGY OF THE NORMAL APICAL IMPULSE PHYSICAL PRINCIPLES GOVERNING THE FORMATION OF THE APICAL IMPULSE NORMAL APICAL IMPULSE AND ITS DETERMINANTS ASSESSMENT OF THE APICAL IMPULSE LEFT PARASTERNAL AND STERNAL MOVEMENTS RIGHT PARASTERNAL MOVEMENT PULSATIONS OVER THE CLAVICULAR HEADS PULSATIONS OVER THE SECOND AND/OR THIRD LEFT INTERCOSTAL SPACES SUBXIPHOID IMPULSE PRACTICAL POINTS IN THE CLINICAL ASSESSMENT OF PRECORDIAL PULSATIONS REFERENCES In this chapter the pulsations of the precordium will be discussed in relation to their identification, the mechanisms of their origin, and their pathophysiological and clinical significance. Precordial pulsations include the “apical impulse,” left parasternal movement, right parasternal movement, pulsations of the clavicular heads, pulsations over the second left intercostal space, and subxiphoid impulses. MECHANICS AND PHYSIOLOGY OF THE NORMAL APICAL IMPULSE Since during systole the heart contracts, becoming smaller and therefore moving away from the chest wall, why should one feel a systolic outward movement (the apical impulse) at all? Logically speaking there should not be an apical impulse. Several different methods of recording the precordial motion have been used to study the apical impulse going back to the late 19th century (1,2). Among the more modern methods, the notable ones are the recordings of the apexcardiogram (3–17), the impulse cardiogram (18), and the kinetocardiogram (19–21). While apexcardiography records the relative displacement of the chest wall under the transducer pickup device, which is often held by the examiner’s hands, the proponents of the impulse cardiography and kinetocardiography point out that these methods allow the recording of the absolute movement of the chest wall because the pickup device is anchored to a fixed point held 113 114 Cardiac Physical Examination in space away from the chest. -
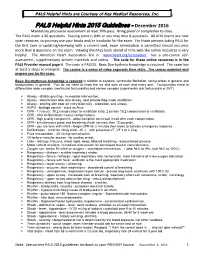
PALS Helpful Hints 2015 Guidelines - December 2016 Mandatory Precourse Assessment at Least 70% Pass
PALSPALS Helpful Helpful Hints Courtesy Hints are of CourtesyKey Medical of Resources, Key Medical Inc. Resources, www.cprclassroom.com Inc. PALS Helpful Hints 2015 Guidelines - December 2016 Mandatory precourse assessment at least 70% pass. Bring proof of completion to class. The PALS exam is 50 questions. Passing score is 84% or you may miss 8 questions. All AHA exams are now open resource, so you may use your books and/or handouts for the exam. For those persons taking PALS for the first time or updating/renewing with a current card, exam remediation is permitted should you miss more than 8 questions on the exam. Viewing the PALS book ahead of time with the online resources is very helpful. The American Heart Association link is www.heart.org/eccstudent has a pre-course self- assessment, supplementary written materials and videos. The code for these online resources is in the PALS Provider manual page ii. The code is PALS15. Basic Dysrhythmia knowledge is required. The exam has at least 5 strips to interpret. The course is a series of video segments then skills. The course materials well prepare you for the exam. Basic Dysrhythmias knowledge is required in relation to asystole, ventricular fibrillation, tachycardias in general and bradycardias in general. You do not need to know the ins and outs of each and every one. Tachycardias need to differentiate wide complex (ventricular tachycardia) and narrow complex (supraventricular tachycardia or SVT). Airway - child is grunting - immediate intervention. Airway - deteriorates after oral airway, next provide bag-mask ventilation. Airway - snoring with poor air entry bilaterally - reposition, oral airway. -

Jugular Venous Pressure
NURSING Jugular Venous Pressure: Measuring PRACTICE & SKILL What is Measuring Jugular Venous Pressure? Measuring jugular venous pressure (JVP) is a noninvasive physical examination technique used to indirectly measure central venous pressure(i.e., the pressure of the blood in the superior and inferior vena cava close to the right atrium). It is a part of a complete cardiovascular assessment. (For more information on cardiovascular assessment in adults, see Nursing Practice & Skill ... Physical Assessment: Performing a Cardiovascular Assessment in Adults ) › What: Measuring JVP is a screening mechanism to identify abnormalities in venous return, blood volume, and right heart hemodynamics › How: JVP is determined by measuring the vertical distance between the sternal angle and the highest point of the visible venous pulsation in the internal jugular vein orthe height of the column of blood in the external jugular vein › Where: JVP can be measured in inpatient, outpatient, and residential settings › Who: Nurses, nurse practitioners, physician assistants, and treating clinicians can measure JVP as part of a complete cardiovascular assessment What is the Desired Outcome of Measuring Jugular Venous Pressure? › The desired outcome of measuring JVP is to establish the patient’s JVP within the normal range or for abnormal JVP to be identified so that appropriate treatment may be initiated. Patients’ level of activity should not be affected by having had the JVP measured ICD-9 Why is Measuring Jugular Venous Pressure Important? 89.62 › The JVP is -

Advanced Life Support (ALS): Tachycardia with a Pulse
MEDICAL DIRECTIVE – Advanced Life Support (ALS): Tachycardia with a Pulse Approved by/Date: Medical Advisory Committee – June 23, 2015 Authorizing physician(s) LHO - Code Blue, Emergency Department & Critical Care Physicians LHB - Emergency Department and Critical Care Physicians LHPP - Emergency Department Physicians Authorized to who Registered Nurses (RN)/Registered Respiratory Therapists (RRT) that have the knowledge, skill and judgment and hold competency in the Lakeridge Health Advanced Life Support competency validation program. Competency validation on theory and practical simulation testing must be completed every two years. Must maintain current Advanced Cardiac Life Support (ACLS) provider status (new or renewal course every 2 years). Patient Description / Population Patients with symptomatic Ventricular Tachycardia (VT) or Supraventricular tachycardia (SVT), defined as a heart rate greater than 150 beats per minute (bpm) and a systolic blood pressure [SBP] less than 90 mmHg plus one or more of the following additional signs and symptoms: acute altered mental status, ongoing chest pain, congestive heart failure, or other signs of shock (dizzy, diaphoretic etc.) Adult patients or patients that appear to be 16 years of age or older. Medical Directive Description/Physician’s Order 1. Notify physician STAT 2. Obtain ECG and 12 lead to confirm rhythm interpretation 3. Administer Amiodarone (IV) 150 mg mixed in 100 mL D5W minibag and infuse over ten minutes. Continuously monitor the patient utilizing cardiac monitor. May repeat Amiodarone (IV) once as necessary prior to physician arrival. 4. Where the patient appears unstable, apply pads in case of need for cardioversion by the physician. Note: Cardioversion is not within RN/RRT scope of practice See Appendix A Document Sponsor/Owner Group: Emergency/Critical Care This material has been prepared solely for the use at Lakeridge Health.