Medullo-Epithelioma (Diktyoma)Of The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Eye Neoplasm
Eye neoplasm Origin and location Eye cancers can be primary (starts within the eye) and metastatic cancer (spread to the eye from another organ). The two most common cancers that spread to the eye from another organ are breast cancer and lung cancer. Other less common sites of origin include the prostate, kidney, thyroid, skin, colon and blood or bone marrow. Types Tumors in the eye and orbit can be benign like dermoid cysts, or malignant like rhabdomyosarcoma and retinoblastoma. Signs and symptoms • Melanomas (choroidal, ciliary body and uveal) - In the early stages there may be no symptoms (the person does not know there is a tumor until an ophthalmologist or optometrist looks into the eye with an ophthalmoscope during a routine test). As the tumor grows, symptoms can be blurred vision, decreased vision, double vision, eventual vision loss and if they continue to grow the tumor can break past the retina causing retinal detachment. Sometimes the tumor can be visible through the pupil. • Nevus - Are benign, freckle in the eye. These should be checked out and regular checks on the eye done to ensure it hasn't turned into a melanoma. • Iris and conjuctival tumors (melanomas) - Presents as a dark spot. Any spot which continues to grow on the iris and the conjunctiva should be checked out. • Retinoblastoma - Strabismus (crossed eyes), a whitish or yellowish glow through the pupil, decreasing/loss of vision, sometimes the eye may be red and painful. Retinoblastoma can occur in one or both eyes. This tumor occurs in babies and young children. It is called RB for short. -

Commentary on the Masquerades of A
perim Ex en l & ta a l ic O p in l h t C h f Journal of Clinical & Experimental a o l m l a o n l r o Chua, J Clin Exp Ophthalmol 2016, 7:2 g u y o J Ophthalmology 10.4172/2155-9570.1000543 ISSN: 2155-9570 DOI: Commentary Open Access Commentary on the Masquerades of a Childhood Ciliary Body Medulloepithelioma: A Case of Chronic Uveitis, Cataract, and Secondary Glaucoma Jocelyn Chua* Eye Specialist Clinic, 290 Orchard Road, Singapore *Corresponding author: Dr Jocelyn Chua, Eye Specialist Clinic, 290 Orchard Road, #06-01 to 05, 238859, Singapore; Tel: +65 96897919; Email: [email protected], [email protected] Received date: February 09, 2016; Accepted date: April 20, 2016; Published date: April 25, 2016 Copyright: © 2016 Chua J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Commentary Ciliary body medulloepithelioma is the commonest ciliary body tumor in childhood. The term “medulloepithelioma”, coined by "The masquerades of a childhood ciliary body medulloepithelioma: Grinker in 1931, best describes the origin of the tumor from the A case of chronic uveitis, cataract and secondary glaucoma" by Chua et primitive medullary epithelium located along the inner layer of the al. [1] is a case report of a healthy two year old boy who presented with optic cup. This undifferentiated medullary epithelium forms the non- a unilateral cataract, anterior uveitis and glaucoma after an innocuous pigmented ciliary body epithelium in the later years of development. -

(Diktyoma) Presenting As a Perforated, Infected Eye
Br J Ophthalmol: first published as 10.1136/bjo.61.3.229 on 1 March 1977. Downloaded from British Journal of Ophthalmology, 1977, 61, 229-232 Medulloepithelioma (diktyoma) presenting as a perforated, infected eye MOHAMED A. VIRJI Central Pathology Laboratory, Ministry of Health, Dar-es-Salaam, Tanzania SUMMARY A case of embryonal medulloepithelioma (diktyoma) presenting with perforated infected eye in a 13-year-old Black African girl is described. The tumour mass occupied most of the deformed eye, and invasion of the sclera anteriorly was seen. There was no evidence of orbital or distant tumour involvement. It is suggested that with increasing age these tumours are more likely to show frankly malignant features. Medulloepithelioma (diktyoma) is a rare neoplasm anteriorly perforated left eye, with loss of cornea, of the eye which is characterised by slow growth and purulent discharge, and a fragmenting mass of local invasion and is composed of glandular, irregular brownish-grey tissue attached mainly to neural, and mesenchymal elements (Andersen, the superior and temporal portion of the eye and 1962). It presents even rarely as an infected perfor- extending into the posterior chamber. The infection ated eye with a fungating mass replacing the ocular was controlled with systemic antibiotics and the left copyright. contents. Soudakoff (1936) reported the case of a eye was enucleated. Radiological examination of 28-year-old Chinese who had a perforated eye with the skull showed no orbital involvement, and chest tumour mass completely filling it. This paper x-rays were normal. Postoperative recovery was reports the case of a young black African girl who uneventful. -

Retinoblastoma Simulators
Retinoblastoma: Atypical Presentation & Simulators Dr. Njambi Ombaba; Paediatric Ophthalmologist, University of Nairobi Objectives • To review of typical presentation of retinoblastoma • To understand the atypical presentation • To understand the Rb simulators Presentation of retinoblastoma Growth patterns Endophytic: Inner retina, vitreous mass, no overlying vessels, pseudohypopyon Exophytic: Outer retina, SR space mass, overlying vessels, RD Diffuse: No mass, signs of inflammation/ endophthalmitis Echogenic soft tissue mass Variable shadowing – calcification Persistent on reduced gain Heterogeneous – necrosis/ haemorrhage Floating debris- vitreous seeds, increased globulin MRI- • Pre-treatment staging T1- Hyper intense to vitreous T2-Hypo intense to vitreous T1:C+Gd- homo/ heterogeneous Enhancement: Choroid & AC ON involvement Hypo intense sclera- Normal Trilateral retinoblastoma CT SCAN Typically a mass of high density Usually calcified and moderately enhancing on iodinated contrast CT has a sensitivity of 81–96%, and a higher specificity for calcification detection However, delineation of intraocular soft-tissue detail is limited. Low sensitivity for ON invasion Atypical presentation Non calcified Retinoblastoma Calcification is key to diagnosis retinoblastoma US detects calcifications in 92–95% of positive cases Non-calcified retinoblastomas: 1. Tumefaction with irregular internal structure 2. Medium reflectivity 3. Typical signs of vascularity 4. Retinal detachment with part of the retinal surface destroyed. Rare, 2% of all -

Successful Treatment of Ciliary Body Medulloepithelioma with Intraocular
Stathopoulos et al. BMC Ophthalmology (2020) 20:239 https://doi.org/10.1186/s12886-020-01512-y CASE REPORT Open Access Successful treatment of ciliary body medulloepithelioma with intraocular melphalan chemotherapy: a case report Christina Stathopoulos*, Marie-Claire Gaillard, Julie Schneider and Francis L. Munier Abstract Background: Intraocular medulloepithelioma is commonly treated with primary enucleation. Conservative treatment options include brachytherapy, local resection and/or cryotherapy in selected cases. We report for the first time the use of targeted chemotherapy to treat a ciliary body medulloepithelioma with aqueous and vitreous seeding. Case presentation: A 17-month-old boy with a diagnosis of ciliary body medulloepithelioma with concomitant seeding and neovascular glaucoma in the right eye was seen for a second opinion after parental refusal of enucleation. Examination under anesthesia showed multiple free-floating cysts in the pupillary area associated with iris neovascularization and a subluxated and notched lens. Ultrasound biomicroscopy revealed a partially cystic mass adjacent to the ciliary body between the 5 and 9 o’clock meridians as well as multiple nodules in the posterior chamber invading the anterior vitreous inferiorly. Fluorescein angiography demonstrated peripheral retinal ischemia. Left eye was unremarkable. Diagnosis of intraocular medulloepithelioma with no extraocular invasion was confirmed and conservative treatment initiated with combined intracameral and intravitreal melphalan injections given according to the previously described safety-enhanced technique. Ciliary tumor and seeding totally regressed after a total of 3 combined intracameral (total dose 8.1 μg) and intravitreal (total dose 70 μg) melphalan injections given every 7–10 days. Ischemic retina was treated with cryoablation as necessary. -
Eye Conditions-DBQ
INTERNAL AFFAIRS VETERANS USE EYE CONDITIONS DISABILITY BENEFITS QUESTIONNAIRE IMPORTANT - THE DEPARTMENT OF VETERANS AFFAIRS (VA) WILL NOT PAY OR REIMBURSE ANY EXPENSES OR COST INCURRED IN THE PROCESS OF COMPLETING AND/OR SUBMITTING THIS FORM. PLEASE READ THE PRIVACY ACT AND RESPONDENT BURDEN INFORMATION ON REVERSE BEFORE COMPLETING FORM. NAME OF PATIENT/VETERAN PATIENT/VETERAN'S SOCIAL SECURITY NUMBER NOTE: This examination must be conducted by a licensed ophthalmologist or by a licensed optometrist. The examiner must identify the disease, injury or other pathologic process responsible for any decrease in visual acuity or other visual impairment found. Examinations of visual fields or muscle function should be conducted ONLY when there is a medical indication of disease or injury that may be associated with visual field defect or impaired muscle function. If indicated to address requested claim, and not medically contraindicated, dilated fundus exam required. IS THIS DBQ BEING COMPLETED IN CONJUNCTION WITH A VA21-2507, C&P EXAMINATION REQUEST? YES NO If "No," how was the examination completed (check all that apply)? In-person examination Records reviewed Other, please specify: Comments: ACCEPTABLE CLINICAL EVIDENCE (ACE) INDICATE METHOD USED TO OBTAIN MEDICAL INFORMATION TO COMPLETE THIS DOCUMENT: Review of available records (without in-person or video telehealth examination) using the Acceptable Clinical Evidence (ACE) process because the existing medical evidence provided sufficient information on which to prepare the DBQ and such an examination will likely provide no additional relevant evidence. Review of available records in conjunction with a telephone interview with the Veteran (without in-person or telehealth examination) using the ACE process because the existing medical evidence supplemented with a telephone interview provided sufficient information on which to prepare the DBQ and such an examination would likely provide no additional relevant evidence. -

Search Strategies for Identifying Systematic Reviews in Eyes and Vision Research
Page 1 of 5 Search Strategies for Identifying Systematic Reviews in Eyes and Vision Research Page 2 of 5 PubMed Search strategies for identifying eyes and vision systematic reviews (ABNORMAL ACCOMMODATION[tiab] OR Abnormal color vision[tiab] OR ABNORMAL LACRIMATION[tiab] OR Abnormal vision[tiab] OR accommodative disorders[tiab] OR Amblyopia[tiab] OR Ametropia[tiab] OR ANISOCORIA[tiab] OR ANOPHTHALMIA[tiab] OR Anterior CHAMBER hemorrhage[tiab] OR Aphakia[tiab] OR aqueous outflow obstruction[tiab] OR Asthenopia[tiab] OR Balint's syndrome[tiab] OR Bilateral visual field constriction[tiab] OR Binocular Vision Disorder[tiab] OR BLEPHARITIS[tiab] OR BLEPHAROSPASM[tiab] OR BLINDNESS[tiab] OR blurred vision[tiab] OR CATARACT[tiab] OR Cataracts[tiab] OR Chorioretinal disorder[tiab] OR Chorioretinitis[tiab] OR Choroid Diseases[tiab] OR Choroidal[tiab] OR Choroiditis[tiab] OR CHROMATOPSIA[tiab] OR Color Blindness[tiab] OR Color Vision Defects[tiab] OR Color vision deficiency[tiab] OR Colour blindness[tiab] OR Conjunctival Diseases[tiab] OR CONJUNCTIVAL HAEMORRHAGE[tiab] OR Conjunctival Injury[tiab] OR CONJUNCTIVAL ULCERATION[tiab] OR CONJUNCTIVITIS[tiab] OR CORNEAL DEPOSITS[tiab] OR Corneal Diseases[tiab] OR Corneal Disorder[tiab] OR Corneal injuries[tiab] OR Corneal Injury[tiab] OR CORNEAL OEDEMA[tiab] OR CORNEAL OPACITY[tiab] OR CORNEAL ULCERATION[tiab] OR decreased Lacrimation[tiab] OR Decreased vision[tiab] OR defective vision[tiab] OR Delayed visual maturation[tiab] OR Difficulty seeing[tiab] OR difficulty with vision[tiab] OR Dim vision[tiab] -

Ocular Oncology and Pathology 2018 Hot Topics in Ocular Pathology and Oncology— an Update
Ocular Oncology and Pathology 2018 Hot Topics in Ocular Pathology and Oncology— An Update Program Directors Patricia Chévez-Barrios MD and Dan S Gombos MD In conjunction with the American Association of Ophthalmic Oncologists and Pathologists McCormick Place Chicago, Illinois Saturday, Oct. 27, 2018 Presented by: The American Academy of Ophthalmology 2018 Ocular Oncology and Pathology Subspecialty Day Advisory Committee Staff Planning Group Daniel S Durrie MD Melanie R Rafaty CMP DES, Director, Patricia Chévez-Barrios MD Associate Secretary Scientific Meetings Program Director Julia A Haller MD Ann L’Estrange, Subspecialty Day Manager Dan S Gombos MD Michael S Lee MD Carolyn Little, Presenter Coordinator Program Director Francis S Mah MD Debra Rosencrance CMP CAE, Vice R Michael Siatkowski MD President, Meetings & Exhibits Former Program Directors Kuldev Singh MD MPH Patricia Heinicke Jr, Copy Editor 2016 Carol L Shields MD Mark Ong, Designer Maria M Aaron MD Gina Comaduran, Cover Designer Patricia Chévez-Barrios MD Secretary for Annual Meeting 2014 Hans E Grossniklaus MD Arun D Singh MD ©2018 American Academy of Ophthalmology. All rights reserved. No portion may be reproduced without express written consent of the American Academy of Ophthalmology. ii Planning Group 2018 Subspecialty Day | Ocular Oncology & Pathology 2018 Ocular Oncology and Pathology Planning Group On behalf of the American Academy of Ophthalmology and the American Association of Ophthalmic Oncologists and Pathologists, it is our pleasure to welcome you to Chicago and -

Rblonyin.Pdf 262.0 KB
Retinoblastoma: the Dangerous White Eye Lon Yin Chan SBSQ11HG – Pd May 31, 2013 Fig 1 Physiology ➢ Incidence Rate: 1 in 18,000 and 30,000; No Racial Bias ➢Incomplete penetrance – may inherit but not express mutation ➢ Can be bilateral (affecting both eyes) or unilateral (affecting only one eye): Unilateral are frequently due to spontaneous mutations, while bilateral are due to germline mutation SYMPTOMS ● Leukocoria: a “white eye” shows rather than typical red eye when light is shone into the eye; this is due to the eye neoplasm – a tumor ●Strbismus: squinting ● Lazy Eye: A rare sign – as lazy eye can occur in other cases ● Conjunctivitus ●Visual Disorientation ●Dymorphic features – occurs if there's a deletion of 13q; includes bulbous tip nose, large mouth, thin upper lip, protruding upper incisors, if serious: may have finger and/or toes abnormalities, and mental retardation ● Many patients have little or no visibility of abnormality ● Early Onset: ● Bilateral cases are shown in the first year ● Unilateral cases are shown between 24 to 30 months Molecular Cause Fig 3 ➔ Mutation in tumor suppressor gene that codes for Rb protein, located at 13q14.1 and 14.2 ➔ Over 900 reported cases of mutation (~ 930) ➔Autosomal Dominant ➔Can be spontaneous or germline mutation; most germline mutations are from paternal allele, and equal frequency from either allele in somatic ➔Caused by mutations or deletion. ➔ Mutations within coding regions destabalizes Rb or compromises its association with enzymes ➔ Mutation within the promoter region causes reduced -

Original Article
J Cancer Allied Spec 2020;6(1):1 Original Article Outcomes of Advanced Retinoblastoma Treated with Local Salvage Treatment; a Retrospective Case Series Palwasha Rehman, Saadiya Javed Khan Department of Pediatric Oncology, Shaukat Khanum Cancer Hospital and Research Centre, Lahore, Pakistan Received: 27 September 2019/Accepted: 16 December 2019 Abstract OPEN ACCESS Correspondence: Palwasha Rehman, Department of Pediatric Introduction: Retinoblastoma (RB) is the most common intraocular Oncology, Shaukat Khanum malignancy arising from the developing retina and occurs in approximately Cancer Hospital and Research one of every 15,000–20,000 births. With the introduction of the intra- Centre, Lahore, Pakistan. arterial chemotherapy (IAC), the 5-year overall survival of children with Email: Palwasharehman@skm. org.pk RB is 99%, though in low- and middle-income countries, it rarely exceeds Citation: Rehman P, Khan SJ. 35% due to limited resources and lack of expertise. The aim of this Outcomes of advanced study was to determine the outcome of local salvage in advanced RB. retinoblastoma treated with Materials and Methods: A retrospective analysis was conducted on local salvage treatment; a retrospective case series. children diagnosed with advanced RB that had local salvage therapy along J Cancer Allied Spec [Internet]. with systemic chemotherapy from January 2015 to January 2018 at Shaukat 2020 Jan.6; 6(1):e1002957. Khanum Memorial Cancer Hospital and Research Centre, Lahore, Pakistan. https://doi.org/10.37029/jcas. Fifteen patients were included in the study, among these 10 were v6i1.281 Results: male. The median age of presentation was 20 months (range 2–40 months). Copyright: © 2020 Rehman and Khan. -
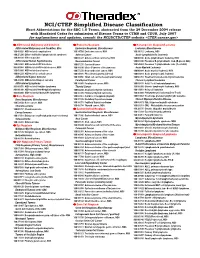
NCI/CTEP Simplified Disease Classification
NCI/CTEP Simplified Disease Classification Short Abbreviations for the SDC 1.0 Terms, abstracted from the 29 December 2004 release with Mandated Codes for submission of Disease Terms to CTMS and CDUS, July 2007 for explanations and updates, consult the NCI/DCTD/CTEP website <CTEP.cancer.gov> ²²² AIDS-related Malignancy and Condition ²²² Endocrine Neoplasm ²²² Hematopoietic Neoplasm/Leukemia AIDS-related Malignancy and Condition, Misc Endocrine Neoplasm, Miscellaneous Leukemia, Miscellaneous 100 49 026 AIDS-related complications 100 14 709 Endocrine cancer, NOS 100 24 312 Leukemia, NOS 100 25 280 Diffuse infiltrative lymphocytosis syndrome Adrenal Cancer Acute Lymphoblastic Leukemia 100 20 188 HIV test positive 100 01 327 Adrenocortical carcinoma, NOS 100 00 846 Acute lymphoblastic leukemia, NOS AIDS-related Human Papillomavirus Neuroendocrine Cancer 100 03 890 Precursor B-lymphoblastic leuk. (B-precur ALL) 100 63 001 AIDS-related HPV infections 100 07 276 Carcinoid tumor 100 54 569 Precursor T-lymphoblastic leuk. (T-cell ALL) 906 00 068 AIDS-related HPV-related cancer, NOS 100 33 630 Islet cell tumors of the pancreas Acute Myeloid Leukemia 100 65 860 AIDS-related anal cancer 100 57 270 Neuroendocrine cancer, NOS 100 00 884 Acute myeloid leukemia, NOS 100 08 229 AIDS-related cervical cancer 100 34 876 Pheochromocytoma (adrenal) 100 01 019 Acute promyelocytic leukemia AIDS-related Kaposi Sarcoma 100 41 056 Small cell carcinoma (extrapulmonary) 100 66 353 Treatment-related acute myloid leukemia 100 23 290 AIDS-related Kaposi sarcoma Parathyroid -
Study Guide for Understanding Pathophysiology This Page Intentionally Left Blank Study Guide for Understanding Pathophysiology
Study Guide for Understanding Pathophysiology This page intentionally left blank Study Guide for Understanding Pathophysiology Sue E. Huether, MSN, PhD Professor Emeritus College of Nursing University of Utah Salt Lake City, Utah Kathryn L. McCance, MSN, PhD Professor College of Nursing University of Utah Salt Lake City, Utah Section Editors Valentina L. Brashers, MD Professor Nursing and Attending Physician in Internal Medicine University of Virginia Health System Charlottesville, Virginia Neal S. Rote, PhD Academic Vice-Chair and Director of Research Department of Obstetrics and Gynecology University Hospitals of Cleveland; Professor of Reproductive Biology and Pathology Case School of Medicine Case Western Reserve University Cleveland, Ohio Prepared by Clayton F. Parkinson, PhD Professor Emeritus College of Health Sciences Weber State University Ogden, Utah 3251 Riverport Lane St. Louis, Missouri 63043 STUDY GUIDE FOR UNDERSTANDING PATHOPHYSIOLOGY, ISBN: 978-0-323-08489-5 5TH EDITION Copyright © 2012, 2008, 2004, 2000, 1996 by Mosby, an imprint of Elsevier Inc. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Details on how to seek permission, further information about the Publisher’s permissions policies and our arrangements with organizations such as the Copyright Clearance Center and the Copyright Licensing Agency, can be found at our website: www.elsevier.com/permissions. This book and the individual contributions contained in it are protected under copyright by the Publisher (other than as may be noted herein). Notices Knowledge and best practice in this field are constantly changing.