Micronized Progesterone, Progestins, and Menopause Hormone Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
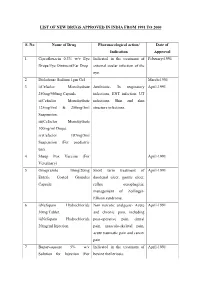
List of New Drugs Approved in India from 1991 to 2000
LIST OF NEW DRUGS APPROVED IN INDIA FROM 1991 TO 2000 S. No Name of Drug Pharmacological action/ Date of Indication Approval 1 Ciprofloxacin 0.3% w/v Eye Indicated in the treatment of February-1991 Drops/Eye Ointment/Ear Drop external ocular infection of the eye. 2 Diclofenac Sodium 1gm Gel March-1991 3 i)Cefaclor Monohydrate Antibiotic- In respiratory April-1991 250mg/500mg Capsule. infections, ENT infection, UT ii)Cefaclor Monohydrate infections, Skin and skin 125mg/5ml & 250mg/5ml structure infections. Suspension. iii)Cefaclor Monohydrate 100mg/ml Drops. iv)Cefaclor 187mg/5ml Suspension (For paediatric use). 4 Sheep Pox Vaccine (For April-1991 Veterinary) 5 Omeprazole 10mg/20mg Short term treatment of April-1991 Enteric Coated Granules duodenal ulcer, gastric ulcer, Capsule reflux oesophagitis, management of Zollinger- Ellison syndrome. 6 i)Nefopam Hydrochloride Non narcotic analgesic- Acute April-1991 30mg Tablet. and chronic pain, including ii)Nefopam Hydrochloride post-operative pain, dental 20mg/ml Injection. pain, musculo-skeletal pain, acute traumatic pain and cancer pain. 7 Buparvaquone 5% w/v Indicated in the treatment of April-1991 Solution for Injection (For bovine theileriosis. Veterinary) 8 i)Kitotifen Fumerate 1mg Anti asthmatic drug- Indicated May-1991 Tablet in prophylactic treatment of ii)Kitotifen Fumerate Syrup bronchial asthma, symptomatic iii)Ketotifen Fumerate Nasal improvement of allergic Drops conditions including rhinitis and conjunctivitis. 9 i)Pefloxacin Mesylate Antibacterial- In the treatment May-1991 Dihydrate 400mg Film Coated of severe infection in adults Tablet caused by sensitive ii)Pefloxacin Mesylate microorganism (gram -ve Dihydrate 400mg/5ml Injection pathogens and staphylococci). iii)Pefloxacin Mesylate Dihydrate 400mg I.V Bottles of 100ml/200ml 10 Ofloxacin 100mg/50ml & Indicated in RTI, UTI, May-1991 200mg/100ml vial Infusion gynaecological infection, skin/soft lesion infection. -

Progestin-Only Systemic Hormone Therapy for Menopausal Hot Flashes
EDITORIAL Progestin-only systemic hormone therapy for menopausal hot flashes Clinicians treating postmenopausal hot flashes often recommend “systemic estrogen treatment.” However, progestin-only therapy also can effectively treat hot flashes and is an option for women with a contraindication to estrogen therapy. Robert L. Barbieri, MD Editor in Chief, OBG MANAGEMENT Chair, Obstetrics and Gynecology Brigham and Women’s Hospital Boston, Massachusetts Kate Macy Ladd Professor of Obstetrics, Gynecology and Reproductive Biology Harvard Medical School he field of menopause medi- women. In one study, 133 postmeno- in postmenopausal women with cine is dominated by studies pausal women with an average age an American Heart Association risk T documenting the effective- of 55 years and approximately 3 years score greater than 10% over 10 years.3 ness of systemic estrogen or estro- from their last menstrual period were Additional contraindications to sys- gen-progestin hormone therapy for randomly assigned to 12 weeks of temic estrogen include women with the treatment of hot flashes caused treatment with placebo or micronized cardiac disease who have a throm- by hypoestrogenism. The effective- progesterone 300 mg daily taken at bophilia, such as the Factor V Leiden ness of progestin-only systemic bedtime.1 Mean serum progesterone mutation.4 hormone therapy for the treatment levels were 0.28 ng/mL (0.89 nM) and For women who are at high risk of hot flashes is much less studied 27 ng/mL (86 nM) in the women taking for estrogen-induced cardiovascu- and seldom is utilized in clinical placebo and micronized progesterone, lar events, micronized progesterone practice. -

Informed Consent for Feminizing Hormone Therapy
Informed Consent for Feminizing Hormone Therapy For _________________________ Date of Birth: _____________ Name Used: ____________________ Patient Name as listed in chart Name if different from chart This form will assist you (and your guardian) to think through the expected effects of hormone therapy including possible unwanted side effects. You are encouraged to talk about this treatment with your medical provider and decide if hormone therapy is right for you (your child). By signing this form, you are stating that you have discussed the effects and risks of this medication with your medical provider or a member of the medical team and that you understand and accept these effects and possible risks. You (and your guardian) may ask questions and talk about any concerns you have related to this treatment at any time in this process. Estrogen (usually estradiol) is used to feminize the body (make it look more traditionally female). This medical treatment will reduce some male features and increase some female features of the body. Androgen (testosterone) blockers further decrease the amount of and/or block the effect of testosterone and masculinization of the body. Your medical provider will help decide which form and the amount of estrogen (shots, pills, gels, patches) and androgen blockers (pills, gels, shots, implanted) that are best for you based on your personal needs and any medical or mental health conditions you might have. Each person’s body responds to estrogen differently and it is hard to promise or predict with certainty how each person may respond to treatment. Your medical provider will talk with you throughout the treatment and will help you achieve the best results safely. -

A Guide to Feminizing Hormones – Estrogen
1 | Feminizing Hormones A Guide to Feminizing Hormones Hormone therapy is an option that can help transgender and gender-diverse people feel more comfortable in their bodies. Like other medical treatments, there are benefits and risks. Knowing what to expect will help us work together to maximize the benefits and minimize the risks. What are hormones? Hormones are chemical messengers that tell the body’s cells how to function, when to grow, when to divide, and when to die. They regulate many functions, including growth, sex drive, hunger, thirst, digestion, metabolism, fat burning & storage, blood sugar, cholesterol levels, and reproduction. What are sex hormones? Sex hormones regulate the development of sex characteristics, including the sex organs such as genitals and ovaries/testicles. Sex hormones also affect the secondary sex characteristics that typically develop at puberty, like facial and body hair, bone growth, breast growth, and voice changes. There are three categories of sex hormones in the body: • Androgens: testosterone, dehydroepiandrosterone (DHEA), dihydrotestosterone (DHT) • Estrogens: estradiol, estriol, estrone • Progestin: progesterone Generally, “males” tend to have higher androgen levels, and “females” tend to have higher levels of estrogens and progestogens. What is hormone therapy? Hormone therapy is taking medicine to change the levels of sex hormones in your body. Changing these levels will affect your hair growth, voice pitch, fat distribution, muscle mass, and other features associated with sex and gender. Feminizing hormone therapy can help make the body look and feel less “masculine” and more “feminine" — making your body more closely match your identity. What medicines are involved? There are different kinds of medicines used to change the levels of sex hormones in your body. -

Classification and Pharmacology of Progestins
Maturitas 46S1 (2003) S7–S16 Classification and pharmacology of progestins Adolf E. Schindler a,∗, Carlo Campagnoli b, René Druckmann c, Johannes Huber d, Jorge R. Pasqualini e, Karl W. Schweppe f, Jos H. H. Thijssen g a Institut für Medizinische Forschung und Fortbildung, Universitätsklinikum, Hufelandstr. 55, Essen 45147, Germany b Ospedale Ginecologico St. Anna, Corso Spezia 60, 10126 Torino, Italy c Ameno-Menopause-Center, 12, Rue de France, 06000 Nice, France d Abt. für Gynäkologische Endokrinologie, AKH Wien, Währingergürtel 18-20, 1090 Wien, Austria e Institute de Puériculture26, Boulevard Brune, 75014 Paris, France f Abt. für Gynäkologie und Geburtshilfe, Ammerland Klinik, Langestr.38, 26622 Westerstede, Germany g Department of Endocrinology, Universitair Medisch Centrum Utrecht, P.O. Box 85090, 3508 AB Utrecht, The Netherlands Abstract Besides the natural progestin, progesterone, there are different classes of progestins, such as retroprogesterone (i.e. dydroges- terone), progesterone derivatives (i.e. medrogestone) 17␣-hydroxyprogesterone derivatives (i.e. chlormadinone acetate, cypro- terone acetate, medroxyprogesterone acetate, megestrol acetate), 19-norprogesterone derivatives (i.e. nomegestrol, promege- stone, trimegestone, nesterone), 19-nortestosterone derivatives norethisterone (NET), lynestrenol, levonorgestrel, desogestrel, gestodene, norgestimate, dienogest) and spironolactone derivatives (i.e. drospirenone). Some of the synthetic progestins are prodrugs, which need to be metabolized to become active compounds. Besides -

Is Alcohol Use Related to High Cholesterol in Premenopausal
Research iMedPub Journals Journal of Preventive Medicine 2018 http://www.imedpub.com/ Vol.3 No.1:3 ISSN 2572-5483 DOI: 10.21767/2572-5483.100024 Is Alcohol Use Related To High Cholesterol in Premenopausal Women Aged 40-51 Years Old? Sydnee Homeyer, Jessica L Hartos*, Holli Lueg, Jessica Moore and Patricia Stafford Department of Physician Assistant Studies, University of North Texas Health Science Center, USA *Corresponding author: Jessica L. Hartos, Department of Physician Assistant Studies, University of North Texas Health Science Center, USA, Tel: 817-735-2454; Fax: 817-735-2529; E-mail: [email protected] Received date: November 13, 2017; Accepted date: January 8, 2018; Publication date: January 15, 2018 Citation: Homeyer S, Hartos JL, Lueg H, Moore J, Stafford P, et al. (2018) Is Alcohol Use Related To High Cholesterol In Premenopausal Women Aged 40-51 Years Old? J Prev Med Vol.3 No.3: 3. Copyright: © 2018 Homeyer S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited. Introduction Abstract Increased serum cholesterol levels is a major risk factor for coronary heart disease (CHD) [1], and over seventy-one million Purpose: Alcohol use and cholesterol are related in men and American adults have high cholesterol (27%) [2,3]. In American postmenopausal women but relations between alcohol use women, cholesterol levels have been shown to increase with and cholesterol are unclear for premenopausal women. The age, and nearly 1 in 2 American women has high or borderline purpose of this study was to determine whether alcohol use was related to cholesterol in women aged 40-51 years old. -

E the Effect of Topiramate on Weight Loss in Patients with Type 2 Diabetes
E The effect of topiramate on weight loss in patients with type 2 diabetes RTICL Sedighe Moradi, Scott Reza Jafarian Kerman, Mina Mollabashi A Institute of Endocrinology and Metabolism (Hemmat Campus), Firoozgar Hospital, Tehran University of Medical Sciences, Tehran, Iran Background: Obesity has been associated with several co‑morbidities such as diabetes and increased mortality. In general, the use of medication promotes only a modest weight loss in the range of 2 to 10 kg, usually most effective during the first 6 months of therapy; however, studies have shown positive effects on other risk factors such as blood pressure and serum glucose levels, but there are fewer studies in patients with diabetes. The aim of this study was to assess the effect of topiramate on weight reduction patients with type 2 diabetes. Materials and Methods: This was a 32‑week randomized clinical trial study of 69 subjects during 2008‑2010. RIGINAL Patients, in two treatment groups were given topiramate (39 patients) and Placebo (30 patients) and were subjected to participation in a non‑pharmacologic lifestyle intervention program; which were randomly allocated in our two groups. The percentage change in body O weight and Body Mass Index (BMI) at the end of the study was the primary efficacy endpoint and secondary indicators were changes in blood pressure (BP), proportion of subjects who achieved 5% or 10% weight loss, changes in lipid profile (total cholesterol, low‑density lipoprotein cholesterol, high‑density lipoprotein cholesterol, triglycerides); and changes in glycosylated hemoglobin (HgA1c). Paired samples and independent samples t‑test was used for statistical analysis. -

Exposure to Female Hormone Drugs During Pregnancy
British Journal of Cancer (1999) 80(7), 1092–1097 © 1999 Cancer Research Campaign Article no. bjoc.1998.0469 Exposure to female hormone drugs during pregnancy: effect on malformations and cancer E Hemminki, M Gissler and H Toukomaa National Research and Development Centre for Welfare and Health, Health Services Research Unit, PO Box 220, 00531 Helsinki, Finland Summary This study aimed to investigate whether the use of female sex hormone drugs during pregnancy is a risk factor for subsequent breast and other oestrogen-dependent cancers among mothers and their children and for genital malformations in the children. A retrospective cohort of 2052 hormone-drug exposed mothers, 2038 control mothers and their 4130 infants was collected from maternity centres in Helsinki from 1954 to 1963. Cancer cases were searched for in national registers through record linkage. Exposures were examined by the type of the drug (oestrogen, progestin only) and by timing (early in pregnancy, only late in pregnancy). There were no statistically significant differences between the groups with regard to mothers’ cancer, either in total or in specified hormone-dependent cancers. The total number of malformations recorded, as well as malformations of the genitals in male infants, were higher among exposed children. The number of cancers among the offspring was small and none of the differences between groups were statistically significant. The study supports the hypothesis that oestrogen or progestin drug therapy during pregnancy causes malformations among children who were exposed in utero but does not support the hypothesis that it causes cancer later in life in the mother; the power to study cancers in offspring, however, was very low. -

2011/097571 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau „ (10) International Publication Number (43) International Publication Date \i\ 11 August 2011 (11.08.2011) 2011/097571 A2 (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 38/22 (2006.01) A61P 11/06 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 31/573 (2006.01) A61P 11/00 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, A61P 29/00 (2006.01) A61P 37/00 (2006.01) CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, PCT/US201 1/023917 KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (22) International Filing Date: ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, 7 February 201 1 (07.02.201 1) NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, (25) Filing Language: English TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (26) Publication Language: English (84) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of regional protection available): ARIPO (BW, GH, 61/302,325 8 February 2010 (08.02.2010) US GM, KE, LR, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, 13/021,950 7 February 201 1 (07.02.201 1) US ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, (71) Applicant (for all designated States except US): EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, PRAIRIE PHARMACEUTICALS, LLC [US/US]; LV, MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, 1041 1 Motor City Drive, Suite 750, Bethesda, MD 20817 SM, TR), OAPI (BF, BJ, CF, CG, CI, CM, GA, GN, GQ, (US). -

Menopausal Hormone Therapy
GYNAECOLOGY ENDOCRINOLOGY Menopausal hormone therapy: where are we now? Menopausal hormone therapy (MHT) is an effective treatment for symptoms associated with menopause, such as hot flushes, night sweats, mood changes, sleep disturbances and changes in sexual function. While the evidence around MHT has changed over the years, there is now international consensus that the benefits of MHT are likely to outweigh the risks for most women aged < 60 years or within ten years of menopause, for whom menopausal symptoms are affecting their quality of life. KEY PRACTICE POINTS: Every woman’s experience of menopause is different, and Among the oestrogen and progestogen formulations perceptions of menopause vary across cultures. Most available, transdermal oestrogen (funded) and micronised women will experience some menopause symptoms, progesterone (not funded) are associated with the lowest however, only some will seek treatment. risk of adverse effects Menopausal hormone therapy (MHT) is likely to offer overall There is no specific recommended duration for MHT. The benefit to women with menopausal symptoms affecting decision to continue treatment should be reviewed on their quality of life if they are aged < 60 years or within ten an annual basis, taking into account any changes in the years of menopause patient’s risk factors, adverse effects and extent of benefit. Adverse outcomes associated with MHT include breast If women primarily seek assistance for urogenital symptoms cancer, stroke and venous thromboembolism (VTE). of menopause, vaginal products are recommended instead However, the risk of these outcomes depends on factors of MHT. This includes moisturisers, lubricants or a vaginal such as the age or time since menopause when MHT oestrogen cream or pessary. -

Giving Another Chance to Mifepristone in Pharmacotherapy for Aggressive Meningiomas—A Likely Synergism with Hydroxyurea?
Curr Probl Cancer 40 (2016) 229–243 Contents lists available at ScienceDirect Curr Probl Cancer journal homepage: www.elsevier.com/locate/cpcancer Giving another chance to mifepristone in pharmacotherapy for aggressive meningiomas—A likely synergism with hydroxyurea? İlhan Elmaci, MDa, Meric A. Altinoz, MDb,*, Aydin Sav, MDc, Zeliha Yazici, PhDd, Aysel Ozpinar, PhDe Introduction Meningiomas: An underestimated health problem Meningiomas are the most frequently reported intracranial tumors, accounting for approx- imately one-fourth of all reported primary brain neoplasms.1 They are benign in approximately 90% of the cases and the remaining cases are either borderline or atypical (World Health Organization [WHO] grade II) or malignant (WHO grade III).1 In the United States, the incidence rates with similar age standardization estimated from figures provided by the Central Brain Tumor Registrywere1.8formenand4.2per100,000forwomenin2006.1 Increasing incidence rates of meningiomas have been reported from several industrialized countries since the early 1980s. But recent studies revealed that real meningioma incidence is even higher.1 As meningiomas are mostly benign, they are not covered by most cancer registries.1 Nevertheless, in Finland, as in other Nordic countries, all surgeons and pathologists are obliged to report all tumors of the central nervous system, both malignant and benign, to the cancer registry.1 To reveal the real incidence of Grant/Financial Support: none. This is original work and is not under consideration for publication elsewhere. This submission is for the special issue being compiled by Beata Holkova on the topic Amylodosis. a Department of Neurosurgery, Memorial Hospital, Istanbul, Turkey b Department of Immunology, Experimental Medical Research Institute/DETAE, Istanbul University, Istanbul, Turkey c Nisantasi Neuropathology Group, Istanbul, Turkey d Department of Pharmacology, Cerrahpasa Faculty of Medicine, Istanbul University, Turkey e Department of Biochemistry, Acibadem University, Istanbul, Turkey * Corresponding author: Meric A. -

Progestogens and Venous Thromboembolism Among Postmenopausal Women Using Hormone Therapy. Marianne Canonico, Geneviève Plu-Bureau, Pierre-Yves Scarabin
Progestogens and venous thromboembolism among postmenopausal women using hormone therapy. Marianne Canonico, Geneviève Plu-Bureau, Pierre-Yves Scarabin To cite this version: Marianne Canonico, Geneviève Plu-Bureau, Pierre-Yves Scarabin. Progestogens and venous throm- boembolism among postmenopausal women using hormone therapy.. Maturitas, Elsevier, 2011, 70 (4), pp.354-60. 10.1016/j.maturitas.2011.10.002. inserm-01148705 HAL Id: inserm-01148705 https://www.hal.inserm.fr/inserm-01148705 Submitted on 5 May 2015 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Progestogens and VTE Finale version Progestogens and venous thromboembolism among postmenopausal women using hormone therapy Marianne Canonico1,2, Geneviève Plu-Bureau1,3 and Pierre-Yves Scarabin1,2 1 Centre for Research in Epidemiology and Population Health, U1018, Hormones and Cardiovascular Disease 2 University Paris-Sud, UMR-S 1018, Villejuif, France 3 University Paris Descartes and Hôtel-Dieu Hospital, Paris, France Adresse: 16 av. Paul Vaillant Couturier 94807 Villejuif Cedex Tel: +33 1 45 59 51 66 Fax: +33 1 45 59 51 70 Corresponding author: Marianne Canonico ([email protected]) 1/21 Progestogens and VTE Finale version Abstract Hormone therapy (HT) is the most effective treatment for correcting menopausal symptoms after menopause.