New Hampshire
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Official List of Public Waters
Official List of Public Waters New Hampshire Department of Environmental Services Water Division Dam Bureau 29 Hazen Drive PO Box 95 Concord, NH 03302-0095 (603) 271-3406 https://www.des.nh.gov NH Official List of Public Waters Revision Date October 9, 2020 Robert R. Scott, Commissioner Thomas E. O’Donovan, Division Director OFFICIAL LIST OF PUBLIC WATERS Published Pursuant to RSA 271:20 II (effective June 26, 1990) IMPORTANT NOTE: Do not use this list for determining water bodies that are subject to the Comprehensive Shoreland Protection Act (CSPA). The CSPA list is available on the NHDES website. Public waters in New Hampshire are prescribed by common law as great ponds (natural waterbodies of 10 acres or more in size), public rivers and streams, and tidal waters. These common law public waters are held by the State in trust for the people of New Hampshire. The State holds the land underlying great ponds and tidal waters (including tidal rivers) in trust for the people of New Hampshire. Generally, but with some exceptions, private property owners hold title to the land underlying freshwater rivers and streams, and the State has an easement over this land for public purposes. Several New Hampshire statutes further define public waters as including artificial impoundments 10 acres or more in size, solely for the purpose of applying specific statutes. Most artificial impoundments were created by the construction of a dam, but some were created by actions such as dredging or as a result of urbanization (usually due to the effect of road crossings obstructing flow and increased runoff from the surrounding area). -

The World's Smallest Republic : Indian Stream Carl Gustafson
Document généré le 1 oct. 2021 04:41 Histoire Québec The World's Smallest Republic : Indian Stream Carl Gustafson Volume 16, numéro 2, 2010 URI : https://id.erudit.org/iderudit/66139ac Aller au sommaire du numéro Éditeur(s) Les Éditions Histoire Québec La Fédération des sociétés d’histoire du Québec ISSN 1201-4710 (imprimé) 1923-2101 (numérique) Découvrir la revue Citer cet article Gustafson, C. (2010). The World's Smallest Republic : Indian Stream. Histoire Québec, 16(2), 36–40. Tous droits réservés © Les Éditions Histoire Québec, 2010 Ce document est protégé par la loi sur le droit d’auteur. L’utilisation des services d’Érudit (y compris la reproduction) est assujettie à sa politique d’utilisation que vous pouvez consulter en ligne. https://apropos.erudit.org/fr/usagers/politique-dutilisation/ Cet article est diffusé et préservé par Érudit. Érudit est un consortium interuniversitaire sans but lucratif composé de l’Université de Montréal, l’Université Laval et l’Université du Québec à Montréal. Il a pour mission la promotion et la valorisation de la recherche. https://www.erudit.org/fr/ Histoire Québec Vol 16, no2:Layout 1 10-10-28 15:49 Page 36 HISTOIRE QUÉBEC VOLUME 16 NUMÉRO 2 2010 The World’s Smallest Republic : Indian Stream by Carl Gustafson Rev. Carl Gustafson (1908-97) spent almost his entire life in the Eastern Townships. He attended school in Waterville and went on to McGill University, where he graduated with degrees in Arts and Divinity. He was ordained by the United Church of Canada and served many congregations in the Townships over a span of more than half a century. -
Stream Crossings Like Habitat Connectivity, Streams Require Continuity to Support the Movement of Aquatic Organisms
MANAGING STATE LANDS FOR WILDLIFE Stream Crossings Like habitat connectivity, streams require continuity to support the movement of aquatic organisms. Many species need different habitats for feeding, breeding, and shelter. The ability to move up or down stream is required for the natural dispersal of individuals. Disruption of stream continuity can result in the loss and degradation of habitat, block wildlife movement, and disrupt the ecological processes that occur in streams over time. Intersections of streams and roads—or stream crossings—have been historically designed to pass water under a road without consideration of stream continuity. Flow variability, natural sediment transport, and aquatic organism passage are overlooked. Characteristic problems of culverts include undersized, shallow, or perched crossings resulting in low or high flow, unnatural bed materials, scouring, erosion, clogging, and ponding. Bridges generally have a lesser impact on streams but, if improperly designed, can still result in sediment deposition and/or streambed degradation. Good stream crossing for wildlife are also good for people. Proper design and placement reduce erosion and damage to roads, infrastructure, and personal property. Click here for more information on Fish and Game’s Fish Habitat Program. Click here for New Hampshire’s Stream Crossing Guidelines and related resources from New Hampshire’s Department of Environmental Services. Mascoma WMA (Canaan) This property contained a 15 foot culvert used to cross the 60-80 foot wide Mascoma River that bisects the property. The culvert was installed by the former landowner. The constriction caused by the culvert led to significant riverbank erosion both up and downstream, forced the river to change course, and deterred fish passage. -

New Hampshire Granite State Ambassadors Great North Woods
New Hampshire Granite State Ambassadors www.NHGraniteStateAmbassadors.org Regional Resource & Referral Guide: Great North Woods Region Use this document filled with local referrals from Granite State Ambassadors & State Welcome Center attendants as an informational starting point for guest referrals. For business referrals, please reference your local brochures & guides. Hidden Gems: ● Baby Flume Gorge, 1212 NH 26 West, Dixville Notch – short walk inside Dixville Notch State Park to a waterfall within a small, narrow gorge. The Cascade Brook Falls are across the road about ¼ mile. (https://www.nhstateparks.org/visit/state-parks/dixville-notch-state- park) ● Beaver Brook Falls, NH 145, Colebrook – About 2.5 miles north of Colebrook on the right- hand side of the road. (https://www.chamberofthenorthcountry.com/blog/best-bets-north- country-waterfalls) ● Pondcherry Wildlife Refuge, Airport Rd., Whitefield – Off NH 115, hiking trails, owned and managed by the U.S. Fish and Wildlife Service in partnership with NH Audubon and NH Department of Fish and Game. (http://www.nhaudubon.org/pondicherry-wildlife-refuge/) ● Lake Umbagog National Wildlife Refuge and NH 16 North along the Thirteen Mile Woods for moose watching and beautiful landscapes. (https://www.fws.gov/refuge/umbagog/) Curiosity: ● North Hill Cemetery, off NH 145, Stewartstown Hollow in Stewartstown – Grave of Metallak was the last Indian living in NH who had not gone to Canada or assimilated into early 19th century American culture. https://www.chamberofthenorthcountry.com/historical- attractions.html) ● 45th Parallel, NH 145, Clarksville – Located in triangular plot at junction of NH 145 and Clarksville Pond Road. At this point you stand at longitude 71 degrees, 24 degrees west from Greenwich, England and half-way between the equator and the north pole. -

Williams Hydroelectric Project FERC Project No
ENVIRONMENTAL ASSESSMENT FOR HYDROPOWER LICENSE Williams Hydroelectric Project FERC Project No. 2335-039 Maine Federal Energy Regulatory Commission Office of Energy Projects Division of Hydropower Licensing 888 First Street, NE Washington, DC 20426 November 2016 TABLE OF CONTENTS TABLE OF CONTENTS ..................................................................................................... i LIST OF FIGURES ............................................................................................................ iii ACRONYMS AND ABBREVIATIONS............................................................................ v EXECUTIVE SUMMARY ............................................................................................... vii 1.0 INTRODUCTION ................................................................................................ 1 1.1 APPLICATION .................................................................................................... 1 1.2 PURPOSE OF ACTION AND NEED FOR POWER ......................................... 1 1.2.1 Purpose of Action .......................................................................................... 1 1.2.2 Need for Power .............................................................................................. 3 1.3 STATUTORY AND REGULATORY REQUIREMENTS ................................. 3 1.3.1 Federal Power Act ......................................................................................... 3 1.3.2 Clean Water Act ........................................................................................... -

Surface Water Supply of the United States 1960
Surface Water Supply of the United States 1960 Part 1 -A. North Atlantic Slope Basins, Maine to Connecticut Prepared under the direction of E. L. HENDRICKS, Chief, Surface Water Branch GEOLOGICAL SURVEY WATER-SUPPLY PAPER 1701 Prepared in cooperation with the States of Connecticut, Maine, Massachusetts, New Hampshire, New York, Rhode Island, and Vermont, and with other agencies UNITED STATES GOVERNMENT PRINTING OFFICE, WASHINGTON : 1961 UNITED STATES DEPARTMENT OF THE INTERIOR STEWART L. UDALL, Secretary GEOLOGICAL SURVEY Thomas B. Nolan, Director For sale by the Superintendent of Documents, U.S. Government Printing Office Washington 25, D.C. PREFACE This report was prepared by the Geological Survey in coopera tion with the States of Connecticut, Maine, Massachusetts, New Hampshire, New York, Rhode Island, and Vermont, and with other agencies, by personnel of the Water Resources Division, L. B. Leopold, chief, under the general direction of E. L. Hendricks, chief, Surface Water Branch, and F. J. Flynn, chief, Basic Records Section. The data were collected and computed under supervision of dis trict engineers, Surface Water Branch, as follows: D. F. Dougherty............................................................. Albany, N. Y. G. S. Hayes................................................................. Augusta, Maine John Horton................................................................. Hartford, Conn. C. E. Knox................................................................... Boston, Mass, HI CALENDAR FOR WATER YEAR 1960 -

The Development of the Upper Connecticut River Valley of New Hampshire, 1750-1820
University of New Hampshire University of New Hampshire Scholars' Repository Honors Theses and Capstones Student Scholarship Spring 2012 From Forest to Freshet: The Development of the Upper Connecticut River Valley of New Hampshire, 1750-1820 Madeleine Beihl University of New Hampshire - Main Campus Follow this and additional works at: https://scholars.unh.edu/honors Part of the United States History Commons Recommended Citation Beihl, Madeleine, "From Forest to Freshet: The Development of the Upper Connecticut River Valley of New Hampshire, 1750-1820" (2012). Honors Theses and Capstones. 32. https://scholars.unh.edu/honors/32 This Senior Honors Thesis is brought to you for free and open access by the Student Scholarship at University of New Hampshire Scholars' Repository. It has been accepted for inclusion in Honors Theses and Capstones by an authorized administrator of University of New Hampshire Scholars' Repository. For more information, please contact [email protected]. From Forest to Freshet: The Development of the Upper Connecticut River Valley of New Hampshire 1750-1820 Madeleine Beihl Senior Honors Thesis University of New Hampshire Spring 2012 Table of Contents Acknowledgements ......................................................................................................................... 2 Introduction ..................................................................................................................................... 3 The Early Years, Pre-1750 ............................................................................................................. -

In the Maine Woods: 1902 Edition (Title: in Pine Tree Jungles) Bangor and Aroostook Railroad
Bangor Public Library Bangor Community: Digital Commons@bpl Maine Railroad Publications Railroads in Bangor and Vicinity 1902 In the Maine Woods: 1902 Edition (Title: In Pine Tree Jungles) Bangor and Aroostook Railroad Follow this and additional works at: http://digicom.bpl.lib.me.us/railroad_pubs Recommended Citation Bangor and Aroostook Railroad, "In the Maine Woods: 1902 Edition (Title: In Pine Tree Jungles)" (1902). Maine Railroad Publications. 28. http://digicom.bpl.lib.me.us/railroad_pubs/28 This Book is brought to you for free and open access by the Railroads in Bangor and Vicinity at Bangor Community: Digital Commons@bpl. It has been accepted for inclusion in Maine Railroad Publications by an authorized administrator of Bangor Community: Digital Commons@bpl. For more information, please contact [email protected]. Copyright ;902 By the Bangor & Aroostook Railroad Co. A copy of this book will be sent to any address on receipt of ten cents by GEo. M. IloUGHToN, Traffic '.tanager, Bangor & Aroostook Railroad Co., Bangor, Maine. WRITTEN A!'ill ARRANGt:I> nv FREI> II. CLIFFORD, BA!'iGUR, MF. ' CONTENTS. Page ON THE \\'AY IN •....... 7 \VHERE BIG FIS!! ARE PLENTY 9 FISH LAWS IN BRIEF . ..... 39 TABLE OF B. & A. FISHING WATERS How HUDNUTT lIELl'ED, A STORY BY HOLMAN F. DAY 49 WHERE THE BIG GAME HIDE SS SHIPMENT OF GAME, 1901 ... GAME LAWS IN BRIEF ......... THE llIGl!-SHOULDERED Hu:>:T, A STORY RY \\'INFH:l.D M. THOMPSON..... 79 JUNGLE VOYAGES HY CA:-OOE ••••... .. .. Ss CA~IPING AND CANOEING . .......... II3 EQl'IPMENT ...•.......•.....•••••..•...................•.....•........ 117 \Vo~IES IN THE \\'oons, BY .MARY AI.DES IIOPKISS .........•........... -

New Hampshire!
New Hampshire Fish and Game Department NEW HAMPSHIRE FRESHWATER FISHING 2021 DIGEST Jan. 1–Dec. 31, 2021 Go Fish New Hampshire! Nearly 1,000 fishable lakes and 12,000 miles of rivers and streams… The Official New Hampshire fishnh.com Digest of Regulations Why Smoker Craft? It takes a true fisherman to know what makes a better fishing experience. That’s why we’re constantly taking things to the next level with design, engineering and construction that deliver best-in-class aluminum fishing boats for every budget. \\Pro Angler: \\Voyager: Grab Your Friends and Head for the Water Years of Worry-Free Reliability More boat for your bucks. The Smoker Craft Pro Angler The Voyager is perfect for the no-nonsense angler. aluminum fishing boat series leads the way with This spacious and deep boat is perfect for the first feature-packed value. time boat buyer or a seasoned veteran who is looking for a solid utility boat. Laconia Alton Bay Hudson 958 Union Ave., PO Box 6145, 396 Main Street 261 Derry Road Route 102 Laconia, NH 03246 Alton Bay, NH 03810 Hudson, NH 03051 603-524-6661 603-875-8848 603-595-7995 www.irwinmarine.com Jan. 1–Dec. 31, 2021 NEW HAMPSHIRE Fish and Game Department FRESHWATER FISHING 2021 DIGEST Lakes and Rivers Galore I am new to Fish and Game, but I was born and raised in New Hampshire and have spent a lifetime working in the outdoors of our Granite State. I grew up with my friends ice fishing for lake trout and cusk on the hard waters of Lake Winnipesaukee and Lake Winnisquam with my father and his friends. -
Public Access and Recreation & Road Management Plans
Connecticut Lakes Headwaters Working Forest Recreation Program Public Access and Recreation & Road Management Plans -Volume 1- For the property owned by the Connecticut Lakes Timber Company and State of New Hampshire Department of Resources and Economic Development Initial Plan Issued: July 3, 2007 Table of Contents 1.0 Introduction .............................................................................................................................2 1.1. What are the purpose and scope of the plan? .....................................................................2 1.2. What is the Connecticut Lakes Headwaters Working Forest Recreation Program and how was it created? ............................................................................................................3 1.3. How is the Initial Plan different from the Interim Plan? ....................................................6 1.4. What substantive requirements must the Plans meet?........................................................6 1.5. What was the planning process?.........................................................................................7 1.5.1. Organizational Meetings ................................................................................................7 1.5.2. Visioning Sessions .........................................................................................................8 1.5.3. Issues and Management Alternatives.............................................................................9 1.6. How did the public influence -
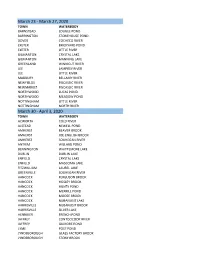
Stocking Report Through June 12, 2020
March 23 ‐ March 27, 2020 TOWN WATERBODY BARNSTEAD LOUGEE POND BARRINGTON STONEHOUSE POND DOVER COCHECO RIVER EXETER BRICKYARD POND EXETER LITTLE RIVER GILMANTON CRYSTAL LAKE GILMANTON MANNING LAKE GREENLAND WINNICUT RIVER LEE LAMPREY RIVER LEE LITTLE RIVER MADBURY BELLAMY RIVER NEWFIELDS PISCASSIC RIVER NEWMARKET PISCASSIC RIVER NORTHWOOD LUCAS POND NORTHWOOD MEADOW POND NOTTINGHAM LITTLE RIVER NOTTINGHAM NORTH RIVER March 30 ‐ April 3, 2020 TOWN WATERBODY ACWORTH COLD RIVER ALSTEAD NEWELL POND AMHERST BEAVER BROOK AMHERST JOE ENGLISH BROOK AMHERST SOUHEGAN RIVER ANTRIM WILLARD POND BENNINGTON WHITTEMORE LAKE DUBLIN DUBLIN LAKE ENFIELD CRYSTAL LAKE ENFIELD MASCOMA LAKE FITZWILLIAM LAUREL LAKE GREENVILLE SOUHEGAN RIVER HANCOCK FERGUSON BROOK HANCOCK HOSLEY BROOK HANCOCK HUNTS POND HANCOCK MERRILL POND HANCOCK MOOSE BROOK HANCOCK NUBANUSIT LAKE HARRISVILLE NUBANUSIT BROOK HARRISVILLE SILVER LAKE HENNIKER FRENCH POND JAFFREY CONTOOCOOK RIVER JAFFREY GILMORE POND LYME POST POND LYNDEBOROUGH GLASS FACTORY BROOK LYNDEBOROUGH STONY BROOK MARLBOROUGH STONE POND MARLOW GUSTIN POND MASON MASON BROOK MERRIMACK SOUHEGAN RIVER MILFORD OSGOOD BROOK MILFORD PURGATORY BROOK MILFORD SOUHEGAN RIVER NELSON CENTER POND NEW LONDON SUNAPEE LAKE, LITTLE PETERBOROUGH CONTOOCOOK RIVER PETERBOROUGH NUBANUSIT BROOK STODDARD COLD SPRING POND STODDARD GRANITE LAKE SULLIVAN CHAPMAN POND SULLIVAN OTTER BROOK SUTTON KEZAR LAKE SWANZEY SWANZEY LAKE WALPOLE CONNECTICUT RIVER WARNER STEVENS BROOK WARNER WARNER RIVER WEARE MT WILLIAM POND WEARE PERKINS POND WEBSTER WINNEPOCKET -

Biological Values of the Connecticut River Watershed's Special Focus
www.fws.gov Special Focus Areas from the Silvio O. Conte NFWR Final EIS (1995) Number State Special Focus Area Name Special Values Priority 1a CT Great Island Marshes/Black Hall River/Lieutenant River 1, 2, 3, 4, 5, 7 High 1b CT North and South Coves 3, 4, 5 Medium 1c CT Ragged Rock Creek 2, 3, 4, 5 High 1d CT Ferry Point 3, 4, 5 Medium 1e CT Turtle Creek 1, 3, 4 High 1f CT Lord Cove 1, 2, 3, 4, 5 High 1g CT Essex Great Meadow 2, 3, 4, 5 High 1h CT Pratt and Post Coves 2, 3, 4, 5, 7 High 1i CT Joshua Creek 3, 4, 5, 7 Medium 1j CT Deep River 3, 4, 5, 7 Medium 1k CT Chester Creek 3, 4, 5, 7 Medium 1l CT Whalebone Creek 1, 2, 3, 4, 5, 7 High 2 CT Hamburg Cove/Eightmile River & East Branch 1, 2, 3, 4, 5, 7 High 3 CT Burnham Brook 3, 6, 8 Medium 4 CT Selden Creek 1, 2, 3, 4, 5, 7 High 5 CT Chapman Pond 1, 2, 3, 4, 5, 7 High 6 CT Salmon Cove 1, 2, 3, 4, 5, 7 High 7 CT Salmon River including tributaries below dams 3 High 8 CT Pecausett Meadows 2, 4, 5, 7 High 9 CT Round & Boggy Meadows/Mattabesset, Coginshaug 2, 3, 4, 5, 7 High River/Wilcox Island 10a CT Dead Mans Swamp 2, 3, 4, 5, 8 High 10b CT Guildersleeve Island 1 High 10c CT Wangunk Meadows 2, 4, 5, 8 High 11a CT Meshomasic Highlands 2, 4, 5, 6, 8 High 11b CT Roaring Brook in Glastonbury 3 Medium 12 CT Great Meadows 1, 2, 4, 5 Medium 13 CT Windsor Meadows/Farmington River Mouth 1, 2, 3, 4, 5 High 14 CT Farmington River & West Branch 2, 3, 7 High 15 CT Scantic River 3, 5 Low 16 CT Enfield Rapids/King Island 1, 2, 3, 5, 7 High 17 MA Honeypot Road Wetlands 2, 4 High 18 MA Mt.