Poster Abstracts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Jilid 12/Bil.1 2012 Issn 2231-8321
BeritaBerita JMMJMM Newsletter of the Department of Museums Malaysia BERITA JMM JILID 12/BIL.1 2012 ISSN 2231-8321 MENARIK DI DALAM PERASMIAN PAMERAN: FORUM KURATOR: MUZIUM TEKSTIL NEGARA MISTERI SANG BUAYA TRADISI ULUNG BUAYEH 6 9 BERITA JMM JILID 12/BIL.1 112012 1 Saban tahun dunia permuziuman sentiasa ditampilkan dengan pelbagai isu-isu baru yang harus diberi perhatian khusus. Peringatan tersebut Penasihat Dato’ Ibrahim bin Ismail dilaungkan melalui pelbagai tema sambutan pada setiap tahun agar dunia permuziuman sentiasa Ketua Editor relevan dengan keadaan semasa. “Muzium dalam Wan Jamaluddin bin Wan Yusoff dunia yang berubah”; satu tema yang sangat menarik yang diutarakan sempena sambutan Hari Editor Mohd Azmi bin Mohd Yusof Muzium Antarabangsa 2012 tahun ini. Tema ini Kamarul Baharin bin A. Kasim merupakan suatu lontaran dan gesaan kepada Azmi bin Ismail penggiat-penggiat muzium supaya lebih peka Zanita binti Anuar dengan perubahan dan kehendak semasa. Tema ini juga menekankan tentang peranan dan tanggung jawab sosial yang perlu Penyelaras Bahagian Penyelidikan digalas oleh muzium. Peranan seumpama itu menjadi kunci kekuatan serta sumbangan muzium kepada masyarakat dan negara. Reka bentuk dan Reka Letak CiME Advertising Dalam mengharungi dunia teknologi yang serba canggih serta persaingan yang hebat, dunia permuziuman seharusnya perlu lebih bijak dan terbuka Fotografi Sumber Media untuk menyesuaikan diri supaya terus diterima masyarakat. Perkhidmatan permuziuman di Malaysia juga perlu bangkit untuk menilai semula peranannya Edaran selaras dengan program ‘Transformasi’ yang dilaungkan kerajaan. Penilaian ini Unit Perpustakaan penting untuk menjamin agar muzium tidak terus terpinggir dari arus perdana. Penghayatan dan kesedaran dikalangan penggiat-penggiat muzium amat Diterbitkan Oleh Jabatan Muzium Malaysia, penting dalam menetapkan hala tuju muzium. -

534.1.Full.Pdf
534 Thursday, 14 June 2018 Scientific Abstracts Ann Rheum Dis: first published as 10.1136/annrheumdis-2018-eular.6917 on 12 June 2018. Downloaded from 1.65; 95% CI 1.29–2.09); this was not observed in HFpEF (RR 0.80; 95% CI 63 (19.4%) had RA, 58 (17.8%) had pSS, 47 (14.5%) had SLE. Overall, 98 0.63–1.01). Following HF diagnosis, RA patients were more likely to be hospital- (30.2%) patients died. The survival rate of pSS-ILD(85.1%) and SLE-ILD(79.3%) ised for non-cardiovascular causes (RR 1.26; 95% CI 1.14–1.39), but not for HF were significantly higher than other CTD-ILDs [SSc-ILD(68.5%), RA-ILD(66.7%), (RR 0.96; 95% CI 0.76–1.21) or other cardiovascular causes (RR 0.99; 95% CI PM/DM-ILD(58.6%), p=0.009]. However, after categorised into three different ILD 0.81–1.20) compared to the non-RA patients. Readmission rates within 30 days imaging subtypes, it showed no statistical differences in survival rates (64.5%, of prior discharge were similar in RA and non-RA (p=0.14). Smoking (current or 73.6%, 69.5% of the UIP group, NSIP group, indeterminate group, respectively, former), prior myocardial infarction (MI) and higher score on Charlson comorbidity p=0.558). Multivariable analysis revealed that compared with DM/PM-ILD, the index were associated with increased risk for hospitalisation: hazard ratio (HR) mortality rate was significantly lower in pSS-ILD(RR=0.321, p=0.001), RA-ILD 1.33, 95% CI 1.06–1.68; HR 1.37, 95% CI 1.03–1.82; and HR 1.10, 95% CI 1.06– (RR=0.466, p=0.016), SSc-ILD(RR=0.566, p=0.045), and SLE-ILD patients 1.14, respectively. -

Senarai Penerima Darjah Kebesaran Persekutuan Tahun 2012 Sempena Sambutan Ulang Tahun Hari Keputeraan Rasmi Seri Paduka Baginda Yang Di-Pertuan Agong
SENARAI PENERIMA DARJAH KEBESARAN PERSEKUTUAN TAHUN 2012 SEMPENA SAMBUTAN ULANG TAHUN HARI KEPUTERAAN RASMI SERI PADUKA BAGINDA YANG DI-PERTUAN AGONG PANGLIMA SETIA MAHKOTA MEMBAWA GELARAN “TAN SRI” PERKHIDMATAN AWAM Bil. Nama, Jawatan dan Alamat 1. YA Datuk Suriyadi bin Halim Omar Hakim Mahkamah Persekutuan Mahkamah Persekutuan Malaysia, Aras 5, Istana Kehakiman, Presint 3 62506 PUTRAJAYA 2. YBhg. Datuk Hamidon bin Ali Bekas Perutusan Tetap Malaysia ke Pertubuhan Bangsa-Bangsa Bersatu, New York, Kementerian Luar Negeri No. 8, Jalan USJ 5/1L 47610 SUBANG JAYA, SELANGOR 3. YBhg. Dato’ Sri Abd. Ghafar bin Mahmud Ketua Pengarah Pelajaran Kementerian Pelajaran Malaysia Aras 8, Blok E8, Kompleks E, Pusat Pentadbiran Kerajaan Persekutuan 62604 PUTRAJAYA 4. YB Datuk Amar Haji Mohamad Morshidi bin Abdul Ghani Setiausaha Kerajaan Negeri Sarawak Pejabat Setiausaha Kerajaan Negeri Sarawak, Pejabat Ketua Menteri Tingkat 20, Wisma Bapa Malaysia, Petra Jaya 93502 KUCHING, SARAWAK 5. YB Datuk Seri Panglima Haji Sukarti bin Wakiman Setiausaha Kerajaan Negeri Sabah Pejabat Setiausaha Kerajaan Negeri Sabah, Jabatan Ketua Menteri Tingkat 6, Wisma Innoprise, Jalan Sulaman, Teluk Likas 88817 KOTA KINABALU, SABAH PIHAK BERKUASA TEMPATAN/ BADAN BERKANUN Bil. Nama, Jawatan dan Alamat 6. YBhg. Dato’ Dr. Mohd Shukor bin Haji Mahfar Ketua Pegawai Eksekutif/Ketua Pengarah Lembaga Hasil Dalam Negeri Ibu Pejabat Lembaga Hasil Dalam Negeri, Aras 18, Menara Hasil, Persiaran Rimba Permai, Cyber 8 63000 CYBERJAYA, SELANGOR SWASTA/ PERSATUAN/ SUKARELA/ SUKAN Bil. Nama, Jawatan dan Alamat 7. YTM Dato’ Seri Utama Tunku Annuar Alhaj ibni Almarhum Sultan Badlishah Pengerusi Jemaah Pemangku Sultan Kedah/ Tunku Bendahara Kedah Temenggong Corp. Sdn. Bhd. B-13-03, Armcorp Tower, No. -

Malaysia Health System Review Health Systems in Transition Vol
Health Systems in Transition Vol. 2 No. 1 2012 Vol. in Transition Health Systems Health Systems in Transition Vol. 3 No.1 2013 Malaysia Health System Review The Asia Pacific Observatory on Health Review Malaysia Health System Systems and Policies is a collaborative partnership which supports and promotes evidence-based health policy making in the Asia Pacific Region. Based in WHO’s Regional Office for the Western Pacific it brings together governments, international agencies, foundations, civil society and the research community with the aim of linking systematic and scientific analysis of health systems in the Asia Pacific Region with the decision- makers who shape policy and practice. Asia Pacific Observatory on Health Systems and Policies Health Systems in Transition Vol. 3 No. 1 2013 Malaysia Health System Review Written by: Safurah Jaafar, Ministry of Health, Malaysia Kamaliah Mohd Noh, Ministry of Health, Malaysia Khairiyah Abdul Muttalib, Ministry of Health, Malaysia Nour Hanah Othman, Ministry of Health, Malaysia Judith Healy, Australian National University, Australia Other authors: Kalsom Maskon, Ministry of Health, Malaysia Abdul Rahim Abdullah, Ministry of Health, Malaysia Jameela Zainuddin, Ministry of Health, Malaysia Azman Abu Bakar, Ministry of Health, Malaysia Sameerah Shaikh Abd Rahman, Ministry of Health, Malaysia Fatanah Ismail, Ministry of Health, Malaysia Chew Yoke Yuen, Ministry of Health, Malaysia Nooraini Baba, Ministry of Health, Malaysia Zakiah Mohd Said, Ministry of Health, Malaysia Edited by: Judith Healy, Australian National University, Australia WHO Library Cataloguing in Publication Data Malaysia health system review. (Health Systems in Transition, Vol. 2 No. 1 2012) 1. Delivery of healthcare. 2. Health care economics and organization. -

(COVID-19) SITUATION in MALAYSIA 3 October 2020
PRESS STATEMENT MINISTRY OF HEALTH MALAYSIA UPDATES ON THE CORONAVIRUS DISEASE 2019 (COVID-19) SITUATION IN MALAYSIA 3 October 2020 Current Status of Confirmed COVID-19 Cases Who Have Recovered The Ministry of Health (MOH) would like to inform that 121 cases have fully recovered and discharged today. Cumulatively, 10,216 confirmed COVID-19 cases have been discharged (84.5% of total cumulative cases). Current Situation of COVID-19 in Malaysia 3 October 2020, 12 pm – a total of 317 additional confirmed COVID-19 cases were reported to the National Crisis Preparedness and Response Centre (CPRC) MOH today. Cumulatively there are now 12,088 confirmed COVID-19 cases in Malaysia. Therefore, there are currently 1,735 active and infective COVID-19 cases. They have all been isolated and given treatment. All 317 cases reported today are local transmission cases involving 303 Malaysians and 14 non-Malaysians. Of the 317 cases, 37 cases have a history of travel to Sabah. Cumulatively there are now 176 cases with a history of travel to Sabah since 20 September 2020. The details of the local transmission COVID-19 cases are as follows: • Sabah: 155 cases o 100 cases from symptomatic screening, involving 96 Malaysians and 4 non-Malaysians. o 35 cases from the Bangau-Bangau Cluster, 33 Malaysians and 2 non-Malaysians o 10 cases from the Benteng LD Cluster, all Malaysians. o 4 cases from community screening, all Malaysians. o 3 cases from the Laut Cluster, all non-Malaysians. o 2 cases from the Joo Hwa Cluster, both Malaysians. o 1 case from the Buang Sayang Cluster, a Malaysian. -

RESEARCH ARTICLE Colorectal Cancer Awareness and Screening
DOI:http://dx.doi.org/10.7314/APJCP.2015.16.18.8345 Colorectal Cancer Awareness and Screening Preference: a Survey during the Malaysian World Digestive Day Campaign RESEARCH ARTICLE Colorectal Cancer Awareness and Screening Preference: A Survey during the Malaysian World Digestive Day Campaign Mohd Azri Mohd Suan1*, Noor Syahireen Mohammed1, Muhammad Radzi Abu Hassan2 Abstract Background: Although the incidence of colorectal cancer in Malaysia is increasing, awareness of this cancer, including its symptoms, risk factors and screening methods, remains low among Malaysian populations. This survey was conducted with the aim of (i) ascertaining the awareness level regarding colorectal cancer symptoms, risk factors and its screening among the general populations and (ii) assessing the public preference and willingness to pay for colorectal cancer screening. Materials and Methods: The questionnaire was distributed in eight major cities in West Malaysia during the World Health Digestive Day (WDHD) campaign. Two thousand four hundred and eight respondents participated in this survey. Results: Generally, awareness of colorectal cancer was found to be relatively good. Symptoms such as change in bowel habit, blood in the stool, weight loss and abdominal pain were well recognized by 86.6%, 86.9%, 83.4% and 85.6% of the respondents, respectively. However, common risk factors such as positive family history, obesity and old age were acknowledged only by less than 70% of the respondents. Almost 80% of the respondents are willing to take the screening test even without any apparent symptoms. Colonoscopy is the preferred screening method, but only 37.5% were willing to pay from their own pocket to get early colonoscopy. -

Sultanah Bahiyah Laid to Rest (NST 28/08/2003)
28/08/2003 Sultanah Bahiyah laid to rest Abdul Razak Ahmad; Alina Simon; Sheridan Mahavera ALOR STAR, Wed. - The Sultanah of Kedah, Tuanku Bahiyah Tuanku Abdul Rahman, 73, who died yesterday, was laid to rest at the Langgar Royal Mausoleum here at 3.22pm today. More than 1,000 people, including the Kedah royal family and State Government officials, were earlier led in the sembahyang jenazah at 10.05am by Masjid Zahir imam Syeikh Roslan Abd Halim. The Sultan of Kedah, Tuanku Abdul Halim Mu'adzam Shah, paid his last respects to the Sultanah at the Balai Penghadapan at 12.05pm. He was accompanied by Menteri Besar Datuk Seri Syed Razak Syed Zain. Prime Minister Datuk Seri Dr Mahathir Mohamad and Datuk Seri Dr Siti Hasmah Mohd Ali arrived at the Balai Penghadapan at 12.37pm to pay their respects. They were followed by Sultan Hassanal Bolkiah of Brunei, and Sultan Sharafuddin Idris Shah of Selangor, both of whom arrived at 12.51pm. Yang di-Pertuan Agong Tuanku Syed Sirajuddin and Raja Permaisuri Agong Tuanku Fauziah arrived at 1pm. Present were the Sultanah's brother, the Yang di-Pertuan Besar of Negri Sembilan Tuanku Ja'afar and the Tengku Ampuan of Negri Sembilan Tuanku Najihah. The day began with Sultanah Bahiyah's coffin being carried from Istana Cegar located in the Anak Bukit palace complex to the nearby Balai Penghadapan. Thousands thronged the hall between 9am and noon to pay their respects. The stairways were clogged with people from all walks of life and the traffic of people to the hall stalled many times as the huge crowd squeezed into the narrow passages of Istana Anak Bukit. -

Program Objective and Target Faculty Members
OBJECTIVE AND TARGET PROGRAM FACULTY MEMBERS Pelvic surgery and the management of pelvic fractures has DATO’ DR. ABDUL RAUF BIN AHMAD Dato’ Dr Suresh Chopra Course Patron Course Advisor advanced greatly among the Malaysia Orthopaedics Head Of Service Advance Trauma Arthoplasty Fellow(Exeter) community. Unstable pelvic fractures can be fatal, Senior Consultant In Orthopaedic Senior Consultant In Orthopaedic therefore requiring urgent management. Departmant Orthopaedic & Departmant Orthopaedic & Traumatology Traumatology Hospital Tuanku Jaafar Hospital Sultanah Bahiyah With the emergence of better knowledge of pelvic Seremban, Negeri Sembilan Alor Setar, Kedah anatomy and implant systems, most pelvic fractures nowadays managed surgically with improved outcome. Miss. Khoh Phaik Shan Mr. Muhammad Azhar Bin Abdullah Course Chairman Course Secretary Orthopaedic Surgeon Orthopaedic Surgeon However surgical exposures and fixation techniques differ TIME MONDAY (04/9) - DAY 1 TUESDAY (05/9) - DAY 2 Departmant Orthopaedic & Departmant Orthopaedic & according to the type of fracture. Therefore the learning Traumatology Traumatology 8:00 am Registration Registration curve is long and arduous. Hospital Sultanah Bahiyah Hospital Sultanah Bahiyah Recitation Of Doa Alor Setar, Kedah Alor Setar, Kedah 8:30 CME Hospital Open Ceremony We hope that this kind of workshop will give surgeons BASIC PELVIC PRACTICAL SESSION sufficient amount of exposure training especially with Anatomy & Biomechanics of Application of Pelvic Ext. SPEAKERS regard to basic surgical -

Senarai Kelulusan Pertukaran Jururawat Gred U29 Berkuatkuasa 20 Januari 2014
SENARAI KELULUSAN PERTUKARAN JURURAWAT GRED U29 BERKUATKUASA 20 JANUARI 2014 LULUS BIL NAMA / NO. KAD PENGENALAN TEMPAT BERTUGAS NEGERI KE NEGERI 1 NURUL -OMME BINTI MOHD SAYUTI HOSPITAL AMPANG SELANGOR KELANTAN 840801-03-5978 2 SITI NORAZIZAH BINTI ABDULLAH HOSPITAL KUALA LUMPUR HKL KELANTAN 850415-03-5004 3 NOOR AYU BINTI HOSPITAL KUALA LUMPUR HKL KELANTAN AB. RAZAK 850310-08-5734 4 NOOR AZLINAWATI HOSPITAL SELAYANG SELANGOR KELANTAN BINTI MOHAMAD 810215-03-5142 5 HALIZA BINTI BISU HOSPITAL SULTAN HAJI AHMAD PAHANG KELANTAN 820702-03-5974 SHAH 6 NORHAYATI BINTI HOSPITAL KUALA LUMPUR HKL KELANTAN MAMAT 850415-03-5020 7 NOOR REHA BINTI MUHAMAD NAWI HOSPITAL RAJA PERMAISURI PERAK KELANTAN 780315-03-5794 BAINUN 8 ROSARIFAH BINTI RAMLI HOSPITAL KUALA LUMPUR HKL KELANTAN 840727-03-6074 9 HASNI BINTI OMAR HOSPITAL TENGKU AMPUAN PAHANG KELANTAN 750118-03-6096 AFZAN 10 ROZIYATUM HADAWIAH BINTI HASAN HOSPITAL KUALA LUMPUR HKL KELANTAN 840108-03-5064 11 UMI KALSOM BINTI DERAMAN HOSPITAL SULTANAH NORA JOHOR KELANTAN 760618-03-5558 ISMAIL 12 ROSMI BINTI HASSAN HOSPITAL SULTANAH AMINAH JOHOR KELANTAN 820709-03-5328 13 SUZEAWANI BINTI CHE MAHMOOD HOSPITAL SUNGAI BULOH SELANGOR KELANTAN 841229-03-5604 14 TUAN HASNIZA BINTI TUAN ISMAIL HOSPITAL SELAYANG SELANGOR KELANTAN @TUAN SOH 750730-03-5946 15 SAMEIAH BINTI SAFIYE HOSPITAL TUANKU JAFFAR NEGERI SEMBILAN KELANTAN 800122-03-5064 16 NOOR HASLINDA BINTI MD. NOR HOSPITAL RAJA PERMAISURI PERAK KELANTAN 760530-13-5748 BAINUN 17 SALINA BINTI MOHAMED HOSPITAL SIK KEDAH KELANTAN 811013-03-5130 18 NORLYDA -

Annex 3 Senarai Pusat Saringan Covid-19 (Hospital)
ANNEX 3 SENARAI PUSAT SARINGAN COVID-19 (HOSPITAL) DAN HOSPITAL YANG MENGENDALIKAN KES COVID-19 A. SENARAI PUSAT SARINGAN COVID-19 (HOSPITAL) HOSPITAL KKM (136) BIL NEGERI BILANGAN SCREENING HOSPITAL MENGIKUT NEGERI 1 PERLIS 1 Hospital Tuanku Fauziah Kangar 2 KEDAH 9 Hospital Sultanah Bahiyah Alor Setar 3 Hospital Sultanah Maliha Langkawi 4 Hospital Jitra 5 Hospital Kuala Nerang 6 Hospital Sultan Abdul Halim Sg Petani 7 Hospital Kulim 8 Hospital Yan 9 Hospital Sik 10 Hospital Baling 11 PULAU PINANG 4 Hospital Pulau Pinang 12 Hospital Sebarang Jaya 13 Hospital Bukit Mertajam 14 Hospital Kepala Batas 15 PERAK 15 Hospital Raja Permaisuri Bainun Ipoh 16 Hospital Taiping 17 Hospital Sri Manjung 18 Hospital Teluk Intan 19 Hospital Slim River 20 Hospital Parit Buntar 21 Hospital Selama 22 Hospital Kuala Kangsar 23 Hospital Gerik 24 Hospital Batu Gajah 25 Hospital Kampar 26 Hospital Sungai Siput 27 Hospital Changkat Melintang 28 Hospital Tapah 29 Hospital Bahagia Ulu Kinta 30 SELANGOR 12 Hospital Tengku Ampuan Rahimah, Klang 31 Hospital Selayang 32 Hospital Serdang 33 Hospital Ampang 34 Hospital Sungai Buloh 35 Hospital Kajang Ministry of Health Malaysia Updated on 11 Jun 2021 ANNEX 3 36 Hospital Shah Alam 37 Hospital Banting 38 Hospital Kuala Kubu Bharu 39 Hospital Tanjung Karang 40 Hospital Tengku Ampuan Jemaah 41 Hospital Orang Asli Gombak 42 WP KUALA 1 Hospital Kuala Lumpur LUMPUR 43 WP PUTRAJAYA 1 Hospital Putrajaya 44 NEGERI 7 Hospital Tuanku Ja'afar Seremban 45 SEMBILAN Hospital Tuanku Ampuan Najihah Kuala Pilah 46 Hospital Tampin 47 Hospital -

ASEAN Senior Travelling Fellowship
ASEAN ORTHOPAEDIC ASSOCIATION Senior Travelling Fellowship 2013 The following Senior Fellows started their Fellowship in Singapore: 1. Dr. Sarwan Singh, Malaysia: sarwan,[email protected] 2. Dr. Andre Chandra Parluhut, Indonesia : [email protected] 3. Dr. Robinson T. Uy, Philippines : [email protected] 4. Dr. Khong Kok Sun, Singapore (first half) ; [email protected] 5. Dr. Kanwaljit Soin, Singapore (second half); [email protected] 6. Dr. Lai Pham Hoang, Vietnam: [email protected] 7. Dr. Kiat Witoonchart, Thailand: [email protected] Singapore: 13.07.2013 to 16.07.2013 13th July 2013 The above fellows flew in from their home countries and assembled at the Ritz Carlton Hotel to observe the rehearsal of the Singapore Independence Day from Dr. Khong Kok Sun’s room, filled with snacks from our various countries and wine. The rehearsal ended with a majestic fireworks display. This was followed by a wonderful dinner at the Ritz Carlton Hotel with AOA Outreach Chairman, Dr Peter Lee and his wife. This enabled the fellows to interact with each other resulting in a closer understanding of each other. 14th July 2013 The following day was a sightseeing day. Being a Sunday, the main hospital units were on emergency standby. So the STFs took the opportunity to see the sights of Singapore. It was a short morning walk across to Marina Bay Sands Hotel’s Sky57 for high-level breakfast. In a light drizzle, we visited the Arts Science Museum with it’s the Mummy secret of the tomb exhibition. After that we walked across to the Gardens by the Bay with its two climate-controlled Flower Domes. -
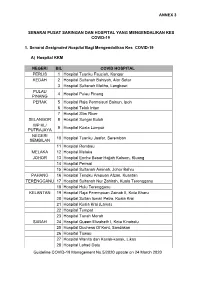
ANNEX 3 Guideline COVID-19 Management No.5/2020 Update On
ANNEX 3 SENARAI PUSAT SARINGAN DAN HOSPITAL YANG MENGENDALIKAN KES COVID-19 1. Senarai Designated Hospital Bagi Mengendalikan Kes COVID-19 A) Hospital KKM NEGERI BIL COVID HOSPITAL PERLIS 1 Hospital Tuanku Fauziah, Kangar KEDAH 2 Hospital Sultanah Bahiyah, Alor Setar 3 Hospital Sultanah Maliha, Langkawi PULAU 4 Hospital Pulau Pinang PINANG PERAK 5 Hospital Raja Permaisuri Bainun, Ipoh 6 Hospital Teluk Intan 7 Hospital Slim River SELANGOR 8 Hospital Sungai Buloh WP KL/ 9 Hospital Kuala Lumpur PUTRAJAYA NEGERI 10 Hospital Tuanku Jaafar, Seremban SEMBILAN 11 Hospital Rembau MELAKA 12 Hospital Melaka JOHOR 13 Hospital Enche Besar Hajjah Kalsom, Kluang 14 Hospital Permai 15 Hospital Sultanah Aminah, Johor Bahru PAHANG 16 Hospital Tengku Ampuan Afzan, Kuantan TERENGGANU 17 Hospital Sultanah Nur Zahirah, Kuala Terengganu 18 Hospital Hulu Terengganu KELANTAN 19 Hospital Raja Perempuan Zainab II, Kota Bharu 20 Hospital Sultan Ismail Petra, Kuala Krai 21 Hospital Kuala Krai (Lama) 22 Hospital Tumpat 23 Hospital Tanah Merah SABAH 24 Hospital Queen Elizabeth I, Kota Kinabalu 25 Hospital Duchess Of Kent, Sandakan 26 Hospital Tawau 27 Hospital Wanita dan Kanak-kanak, Likas 28 Hospital Lahad Datu Guideline COVID-19 Management No.5/2020 update on 24 March 2020 ANNEX 3 NEGERI BIL COVID HOSPITAL 29 Hospital Keningau SARAWAK 30 Hospital Umum Sarawak, Kuching 31 Hospital Miri 32 Hospital Bintulu 33 Hospital Sibu WP LABUAN 34 Hospital Labuan B) Hospital Bukan KKM ADMITTING HOSPITALS* NEGERI BIL SCREENING HOSPITALS BIL FOR ‘PUI & ‘CONFIRMED COVID-19’ WP KL/ Pusat Perubatan Universiti Pusat Perubatan Universiti 1 1 PUTRAJAYA Malaya Malaya 2. Screening Centre For COVID-19 SCREENING KLINIK KESIHATAN KLINIK KESIHATAN HOSPITALS (WAKTU BEKERJA) (SEMASA HUJUNG MINGGU) 1.