Actemra® (Tocilizumab)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genmab and ADC Therapeutics Announce Amended Agreement for Camidanlumab Tesirine (Cami)
Genmab and ADC Therapeutics Announce Amended Agreement for Camidanlumab Tesirine (Cami) Media Release Copenhagen, Denmark and Lausanne, Switzerland, October 30, 2020 • ADC Therapeutics to continue the development and commercialization of Cami • Genmab to receive mid-to-high single-digit tiered royalty Genmab A/S (Nasdaq: GMAB) and ADC Therapeutics SA (NYSE: ADCT) today announced that they have executed an amended agreement for ADC Therapeutics to continue the development and commercialization of camidanlumab tesirine (Cami). The parties first entered into a collaboration and license agreement in June 2013 for the development of Cami, an antibody drug conjugate (ADC) which combines Genmab’s HuMax®-TAC antibody targeting CD25 with ADC Therapeutics’ highly potent pyrrolobenzodiazepine (PBD) warhead technology. Under the terms of the 2013 agreement, the parties were to determine the path forward for continued development and commercialization of Cami upon completion of a Phase 1a/b clinical trial. ADC Therapeutics previously announced that Cami achieved an overall response rate of 86.5%, including a complete response rate of 48.6%, in Hodgkin lymphoma patients in this trial who had received a median of five prior lines of therapy. Cami is currently being evaluated in a 100-patient pivotal Phase 2 clinical trial intended to support the submission of a Biologics License Application (BLA) to the U.S. Food and Drug Administration (FDA). The trial is more than 50 percent enrolled and ADC Therapeutics anticipates reporting interim results in the first half of 2021. “We have a long-standing relationship with the ADC Therapeutics team and believe they are an ideal partner for the ongoing development and potential commercialization of Cami,” said Jan van de Winkel, Ph.D., Chief Executive Officer of Genmab. -

ADC Therapeutics SA (Exact Name of Registrant As Specified in Its Charter)
UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 FORM 6-K REPORT OF FOREIGN PRIVATE ISSUER PURSUANT TO RULE 13a-16 OR 15d-16 UNDER THE SECURITIES EXCHANGE ACT OF 1934 For the month of February 2021. Commission File Number: 001-39071 ADC Therapeutics SA (Exact name of registrant as specified in its charter) Biopôle Route de la Corniche 3B 1066 Epalinges Switzerland (Address of principal executive office) Indicate by check mark whether the registrant files or will file annual reports under cover of Form 20-F or Form 40-F: Form 20-F ☒ Form 40-F Indicate by check mark if the registrant is submitting the Form 6-K in paper as permitted by Regulation S-T Rule 101(b)(1): ☐ Indicate by check mark if the registrant is submitting the Form 6-K in paper as permitted by Regulation S-T Rule 101(b)(7): ☐ SIGNATURE Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized. ADC Therapeutics SA Date: February 4, 2021 By: /s/ Michael Forer Name: Michael Forer Title: Executive Vice President & General Counsel EXHIBIT INDEX Exhibit No. Description 99.1 Press release dated February 4, 2021 Exhibit 99.1 ADC Therapeutics Completes Enrollment in Pivotal Phase 2 Clinical Trial of Camidanlumab Tesirine (Cami) in Relapsed or Refractory Hodgkin Lymphoma Interim results anticipated in the first half of 2021 LAUSANNE, Switzerland, February 4, 2021 – ADC Therapeutics SA (NYSE:ADCT), a late clinical-stage oncology-focused biotechnology company pioneering the development and commercialization of highly potent and targeted antibody drug conjugates (ADCs) for patients with hematological malignancies and solid tumors, today announced completion of enrollment in the pivotal Phase 2 clinical trial evaluating the efficacy and safety of camidanlumab tesirine (Cami, formerly ADCT-301) in patients with relapsed or refractory Hodgkin lymphoma. -

ADC Therapeutics SA (Exact Name of Registrant As Specified in Its Charter)
UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 FORM 6-K REPORT OF FOREIGN PRIVATE ISSUER PURSUANT TO RULE 13a-16 OR 15d-16 UNDER THE SECURITIES EXCHANGE ACT OF 1934 For the month of July, 2020. Commission File Number: 001-39071 ADC Therapeutics SA (Exact name of registrant as specified in its charter) Biopôle Route de la Corniche 3B 1066 Epalinges Switzerland (Address of principal executive office) Indicate by check mark whether the registrant files or will file annual reports under cover of Form 20-F or Form 40-F: Form 20-F ☒ Form 40-F Indicate by check mark if the registrant is submitting the Form 6-K in paper as permitted by Regulation S-T Rule 101(b)(1): ☐ Indicate by check mark if the registrant is submitting the Form 6-K in paper as permitted by Regulation S-T Rule 101(b)(7): ☐ SIGNATURE Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized. ADC Therapeutics SA Date: July 6, 2020 By: /s/ Dominique Graz Name: Dominique Graz Title: General Counsel EXHIBIT INDEX Exhibit No. Description 99.1 Press release dated July 6, 2020 Exhibit 99.1 ADC Therapeutics Announces U.S. Food and Drug Administration Has Lifted Partial Clinical Hold on Pivotal Phase 2 Clinical Trial of Camidanlumab Tesirine Lausanne, Switzerland — July 6, 2020 — ADC Therapeutics SA (NYSE:ADCT), a clinical-stage oncology-focused biotechnology company leading the development and commercialization of next-generation antibody drug conjugates (ADCs) with highly potent and targeted pyrrolobenzodiazepine (PBD) dimer technology, today announced that the U.S. -

Comparative Effectiveness of Pembrolizumab Vs. Nivolumab In
www.nature.com/scientificreports OPEN Comparative efectiveness of pembrolizumab vs. nivolumab in patients with recurrent or advanced NSCLC Pengfei Cui1,2,4, Ruixin Li2,4, Ziwei Huang3,2,4, Zhaozhen Wu3,2, Haitao Tao2, Sujie Zhang2 & Yi Hu1,2,3* The efcacies of pembrolizumab and nivolumab have never been directly compared in a real-world study. Therefore, we sought to retrospectively evaluate the objective response rate (ORR) and the progression-free survival (PFS) of patients with recurrent or advanced non-small cell lung cancer (NSCLC) in a real-world setting. This study included patients with recurrent or advanced NSCLC diagnosed between September 1, 2015 and August 31, 2019, who were treated with programmed cell death 1 (PD-1) inhibitors at the Cancer Center of the Chinese People’s Liberation Army. PFS was estimated for each treatment group using Kaplan–Meier curves and log-rank tests. The multivariate analysis of PFS was performed with Cox proportional hazards regression models. A total of 255 patients with advanced or recurrent NSCLC treated with PD-1 inhibitors were identifed. The ORR was signifcantly higher in the pembrolizumab group than in the nivolumab group, while PFS was not signifcantly diferent between the two groups. Subgroup analysis showed that the ORR was signifcantly higher for pembrolizumab than for nivolumab in patients in the frst-line therapy subgroup and in those in the combination therapy as frst-line therapy subgroup. Survival analysis of patients receiving combination therapy as second- or further-line therapy showed that nivolumab had better efcacy than pembrolizumab. However, the multivariate analysis revealed no signifcant diference in PFS between patients treated with pembrolizumab and those treated with nivolumab regardless of the subgroup. -

Cutaneous Adverse Effects of Biologic Medications
REVIEW CME MOC Selena R. Pasadyn, BA Daniel Knabel, MD Anthony P. Fernandez, MD, PhD Christine B. Warren, MD, MS Cleveland Clinic Lerner College Department of Pathology Co-Medical Director of Continuing Medical Education; Department of Dermatology, Cleveland Clinic; of Medicine of Case Western and Department of Dermatology, W.D. Steck Chair of Clinical Dermatology; Director of Clinical Assistant Professor, Cleveland Clinic Reserve University, Cleveland, OH Cleveland Clinic Medical and Inpatient Dermatology; Departments of Lerner College of Medicine of Case Western Dermatology and Pathology, Cleveland Clinic; Assistant Reserve University, Cleveland, OH Clinical Professor, Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, OH Cutaneous adverse effects of biologic medications ABSTRACT iologic therapy encompasses an expo- B nentially expanding arena of medicine. Biologic therapies have become widely used but often As the name implies, biologic therapies are de- cause cutaneous adverse effects. The authors discuss the rived from living organisms and consist largely cutaneous adverse effects of tumor necrosis factor (TNF) of proteins, sugars, and nucleic acids. A clas- alpha inhibitors, epidermal growth factor receptor (EGFR) sic example of an early biologic medication is inhibitors, small-molecule tyrosine kinase inhibitors insulin. These therapies have revolutionized (TKIs), and cell surface-targeted monoclonal antibodies, medicine and offer targeted therapy for an including how to manage these reactions -

5.01.591 Immune Checkpoint Inhibitors
MEDICAL POLICY – 5.01.591 Immune Checkpoint Inhibitors Effective Date: Sept. 1, 2021 RELATED POLICIES/GUIDELINES: Last Revised: Aug. 10, 2021 5.01.543 General Medical Necessity Criteria for Companion Diagnostics Related Replaces: N/A to Drug Approval 5.01.589 BRAF and MEK Inhibitors Select a hyperlink below to be directed to that section. POLICY CRITERIA | DOCUMENTATION REQUIREMENTS | CODING RELATED INFORMATION | EVIDENCE REVIEW | REFERENCES | HISTORY ∞ Clicking this icon returns you to the hyperlinks menu above. Introduction Chemotherapy, often called chemo, is cancer treatment that uses drugs. Radiation and surgery treat one area of cancer. But chemo usually travels through the bloodstream to treat the whole body. Treating the whole body is called a systemic treatment. Immunotherapy is a new type of cancer treatment that helps the body’s immune cells fight the cancer more effectively. Cancer cells sometimes “hide” from the body’s cells that are designed to search for cells that don’t belong, like cancer cells or bacteria. Immune checkpoint inhibitors are drugs that block the way that cancer cells do this and so help the immune cells find them so they can be stopped. It is one of the ways we can make the environment less friendly to the cancer and slow its growth. Current immunotherapy drugs are complex molecules that must be given through a vein (intravenous). In the future, some may be given by a shot (injection) the patient could inject without help. This policy gives information about immunotherapy drugs and the criteria for when they may be medically necessary. Note: The Introduction section is for your general knowledge and is not to be taken as policy coverage criteria. -

Actemra (Tocilizumab) NON-ONCOLOGY POLICY (Intravenous) Department: PHA
Policy Title: Actemra (tocilizumab) NON-ONCOLOGY POLICY (Intravenous) Department: PHA Effective Date: 01/01/2020 Review Date: 09/25/2019, 12/18/2019, 1/22/2020, 8/3/2020 Revision Date: 09/25/2019, 12/18/2019, 1/22/2020, 8/3/2020 Purpose: To support safe, effective and appropriate use of Actemra (tocilizumab). Scope: Medicaid, Commerical, Medicare-Medicaid Plan (MMP) Policy Statement: Actemra (tocilizumab) is covered under the Medical Benefit when used within the following guidelines for non-oncology indications. Use outside of these guidelines may result in non-payment unless approved under an exception process. For oncology indications, please refer to NHPRI Oncology Policy Procedure: Coverage of Actemra (tocilizumab) will be reviewed prospectively via the prior authorization process based on criteria below. Initial Criteria: Patient has been evaluated and screened for the presence of latent TB infection prior to initiating treatment; AND Patient does not have an active infection, including clinically important localized infections; AND Must not be administered concurrently with live vaccines; AND Patient is not on concurrent treatment with another TNF-inhibitor, biologic response modifier or other non-biologic agent (i.e., apremilast, tofacitinib, baricitinib); MMP members who have previously received this medication within the past 365 days are not subject to Step Therapy Requirements Rheumatoid Arthritis Patient is 18 years or older; AND Physician has assessed baseline disease severity utilizing an objective measure/tool; AND -

On the Horizon: Immuno-Oncology (I-O) Combinations
Immuno-Oncology (I-O) Combinations • Jeffrey A. Sosman, MD • Robert H. Lurie Comprehensive Cancer Center of Northwestern University The Cancer–Immunity Cycle Daniel Chen and Ira Mellman Immunity, Volume 39, Issue 1, 2013, 1 - 10 The Cancer–Immunity Cycle Daniel Chen and Ira Mellman Immunity, Volume 39, Issue 1, 2013, 1 - 10 Stimulatory and Inhibitory Factors in the Cancer-Immunity Cycle Each step of the Cancer-Immunity Cycle requires the coordination of numerous factors, both stimulatory and inhibitory in nature. Stimulatory factors shown in green promote immunity, ... Where will Improvements come from? • Combinations: – Based on Template: anti-PD-1/PD-L1 or with anti-PD- 1/anti-CTLA-4 • Block other co-inhibitory: LAG3, TIM3, KIR, VISTA • Activate co-stimulatory: 4-1BB, OX-40, GITR, CD27, ICOS • Block inhibitory molecules- IDOi, TGFbi, CSF1Ri, anti-IL-6 or anti- IL-10 • Effect trafficking- anti-VEGF, CCL5, CXCR4i • Vaccines- TVEC- oncolytic virus, Neoantigen, other cellular • Adoptive Cellular therapy- TIL, CAR-T cells, TCR T-cells Where will Improvements come from? • Combinations: – Based on Template: anti-PD-1/PD-L1 or with anti-PD- 1/anti-CTLA-4 • Signal Inhibition, BRAF directed (BRAFi+MEKi), MEKi, PI3K inhibition (PTEN effects) • Cytokines- IL-2, IFN a,b,g,, Directed cytokines (FAP-IL-2v or CEA-IL-2v) • Epigenetic modulation- gene expression and EVR expression • Microbiome modification- fecal transplants • Chemotherapy other cytotoxics • Localized Irradiation SBRT, SRS T cells in Tumors Express Multiple Immunoinhibitory Receptors -
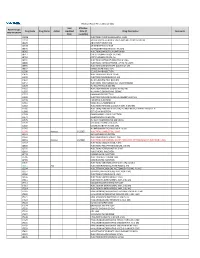
2021 Prior Authorization List Part B Appendix a (PDF)
Medicare Part B PA List Effective 2021 Last Effective Part B Drugs: Drug Code Drug Name Action Updated Date (if Drug Description Comments STEP THERAPY Date available) C9050 INJECTION, EMAPALUMAB-LZSG, 1 MG C9122 MOMETASONE FUROATE SINUS IMPLANT 10 MCG SINUVA J0129 ABATACEPT INJECTION J0178 AFLIBERCEPT INJECTION J0570 BUPRENORPHINE IMPLANT 74.2MG J0585 INJECTION,ONABOTULINUMTOXINA J0717 CERTOLIZUMAB PEGOL INJ 1MG J0718 CERTOLIZUMAB PEGOL INJ J0791 INJECTION CRIZANLIZUMAB-TMCA 5 MG J0800 INJECTION, CORTICOTROPIN, UP TO 40 UNITS J0896 INJECTION LUSPATERCEPT-AAMT 0.25 MG J0897 DENOSUMAB INJECTION J1300 ECULIZUMAB INJECTION J1428 INJECTION ETEPLIRSEN 10 MG J1429 INJECTION GOLODIRSEN 10 MG J1442 INJ FILGRASTIM EXCL BIOSIMIL J1447 INJECTION, TBO-FILGRASTIM, 1 MICROGRAM J1459 INJ IVIG PRIVIGEN 500 MG J1555 INJECTION IMMUNE GLOBULIN 100 MG J1556 INJ, IMM GLOB BIVIGAM, 500MG J1557 GAMMAPLEX INJECTION J1558 INJECTION IMMUNE GLOBULIN XEMBIFY 100 MG J1559 HIZENTRA INJECTION J1561 GAMUNEX-C/GAMMAKED J1562 INJECTION; IMMUNE GLOBULIN 10%, 5 GRAMS J1566 INJECTION, IMMUNE GLOBULIN, INTRAVENOUS, LYOPHILIZED (E.G. P J1568 OCTAGAM INJECTION J1569 GAMMAGARD LIQUID INJECTION J1572 FLEBOGAMMA INJECTION J1575 INJ IG/HYALURONIDASE 100 MG IG J1599 IVIG NON-LYOPHILIZED, NOS J1602 GOLIMUMAB FOR IV USE 1MG J1745 INJ INFLIXIMAB EXCL BIOSIMILR 10 MG J1930 Remove 1/1/2021 INJECTION, LANREOTIDE, 1 MG J2323 NATALIZUMAB INJECTION J2350 INJECTION OCRELIZUMAB 1 MG J2353 Remove 1/1/2021 INJECTION, OCTREOTIDE, DEPOT FORM FOR INTRAMUSCULAR INJECTION, 1 MG J2357 INJECTION, OMALIZUMAB, -

NICE UPDATE for COMMISSIONERS April 2019
South, Central and West NICE UPDATE FOR COMMISSIONERS April 2019 This NICE Update for Commissioners includes: At-a-glance summary Headline update: what’s been published? Guidance and quality standards published by NICE in March 2019 What’s new for CCGs? Horizon scanning What’s coming out from NICE in the next six months? For your reference, a summary of the types of NICE guidance Reference – a guide to NICE products The next (May 2019) NICE Update for Commissioners will be issued at the beginning of June 2019. For further information about NICE guidance and its implementation contact: Tiina Korhonen, Clinical Effectiveness Lead Kathryn Markey, Clinical Effectiveness Manager Kate Forbes, Clinical Effectiveness Manager Rebecca Hodge, Clinical Effectiveness Manager Gill Barlow, Clinical Effectiveness Manager Katie Newens, Clinical Effectiveness Researcher Rachel Finch, Clinical Effectiveness Administrator [email protected] 1 | p a g e At-a-glance summary The table below shows ALL NICE guidance published in April2019. Those likely to have significant impact for CCG commissioners are discussed further in the ‘What’s new for Clinical Commissioning Groups’ section (link to relevant section provided within guidance reference). Guidance type and Title Commissioner(s) Main providers(s) Impact for CCG commissioners (financial /public reference interest/quality of care) Technology Appraisal – Daratumumab with NHS England Secondary care - TA573 bortezomib and acute and dexamethasone for Tertiary care previously treated multiple myeloma Technology Appraisal – Certolizumab pegol for CCGs Primary care, NICE does not expect this guidance to have a TA574 treating moderate to severe secondary care - significant impact on resources; that is, it will be plaque psoriasis acute and tertiary less than £5 million per year in England (or care £9,100 per 100,000 population) because the technology is an option alongside current standard treatment options and is available at a similar price. -

Clinical Practice Guidelines Slideset Toxicities Immunotherapy
Management of toxicities from immunotherapy ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up J. Haanen, F. Carbonnel, C. Robert, K. Kerr, S. Peters, J. Larkin and K. Jordan, on behalf of the ESMO Guidelines Committee *For details of author affiliations, correspondence and versions, please see the full version at esmo.org/Guidelines/Supportive-and-Palliative-Care Incidence and epidemiology Time to onset and resolution of occurrence of immuno-related adverse events following Ipilimumab treatment Weber JS et al. J Clin Oncol 2012;30:2691–2697. Reprinted with permission. ©2012 American Society of Clinical Oncology. All rights reserved. © 2018 ESMO. All rights reserved. esmo.org/Guidelines/Supportive-and-Palliative-Care/Management-of-Toxicities-from-Immunotherapy Incidence and epidemiology Time to onset of grade 3-4 treatment-related select adverse events Larkin J et al. Presented at ECC 2015;Abs330. Reprinted with permission. © 2018 ESMO. All rights reserved. esmo.org/Guidelines/Supportive-and-Palliative-Care/Management-of-Toxicities-from-Immunotherapy Summary of recommendations General aspects Generally occur within 3 months after initiation of ICPi treatment of immune- related adverse Tissue biopsy may be useful for higher grade (3-4) toxicities, when there is diagnostic events (irAEs) doubt and management would be altered by the outcome Before starting treatment: patients’ susceptibility to irAEs should be assessed and Incidence and patients informed of the potential AEs, reporting directly to the treating physician -

KEYTRUDA® (Pembrolizumab)
MEDICATION GUIDE KEYTRUDA® (key-true-duh) KEYTRUDA® (key-true-duh) (pembrolizumab) (pembrolizumab) for injection injection What is the most important information I should know about KEYTRUDA? KEYTRUDA is a medicine that may treat your melanoma or lung cancer by working with your immune system. KEYTRUDA can cause your immune system to attack normal organs and tissues in many areas of your body and can affect the way they work. These problems can sometimes become serious or life-threatening and can lead to death. Call or see your doctor right away if you develop any symptoms of the following problems or these symptoms get worse: Lung problems (pneumonitis). Symptoms of pneumonitis may include: shortness of breath chest pain new or worse cough Intestinal problems (colitis) that can lead to tears or holes in your intestine. Signs and symptoms of colitis may include: diarrhea or more bowel movements than usual stools that are black, tarry, sticky, or have blood or mucus severe stomach-area (abdomen) pain or tenderness Liver problems (hepatitis). Signs and symptoms of hepatitis may include: yellowing of your skin or the whites of your eyes nausea or vomiting pain on the right side of your stomach area (abdomen) dark urine feeling less hungry than usual bleeding or bruising more easily than normal Hormone gland problems (especially the thyroid, pituitary, adrenal glands, and pancreas). Signs and symptoms that your hormone glands are not working properly may include: rapid heart beat weight loss or weight gain increased sweating feeling more hungry or thirsty urinating more often than usual hair loss feeling cold constipation your voice gets deeper muscle aches dizziness or fainting headaches that will not go away or unusual headache Kidney problems, including nephritis and kidney failure.