Cognitive and Functional Decline in Patients with Mild Alzheimer Dementia with Or Without Comorbid Diabetes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treatment of Diabetes Mellitus
TREATMENT OF DIABETES MELLITUS DIABETES is a condition that affects how the body makes energy from food. Food is broken down into sugar (glucose) in the body and released into the blood. When the blood sugar level rises after a meal, insulin responds to let the sugar into the cells to be used as energy. In diabetes, the body either does not make enough insulin or it stops responding to insulin as well as it should. This results in sugar staying in the blood and leads to serious health problems over time. DIAGNOSIS OF DIABETES1 • A1C Test: Lab test measuring average blood sugar over past two to three months • Fasting Blood Sugar Test: Lab test measuring blood sugar after eight hours of no food or drink • Oral Glucose Tolerance Test (OGTT): Measures blood sugar before and two hours after drinking a specific sugary liquid • Random Blood Sugar Test: Measures blood sugar at a moment in time, without any kind of preparation (like fasting) FASTING BLOOD ORAL GLUCOSE TOLERANCE RANDOM BLOOD RESULT A1C TEST SUGAR TEST TEST SUGAR TEST Diabetes ≥ 6.5% ≥126 mg/dL ≥ 200 mg/dL ≥ 200 mg/dL Prediabetes 5.7 – 6.4% 100 – 125 mg/dL 140 – 199 mg/dL N/A Normal < 5.7% ≤99 mg/dL < 140 mg/dL N/A NON-DRUG TREATMENTS2 THERAPY COST WHAT TO EXPECT Diet (Mediterranean diet) and exercise (30 minutes a day, five days a week of moderate- Weight loss $-$$ intensity exercise); 7% weight loss decreases risk of diabetes3 Psychological intervention $$-$$$ Psychotherapy may reduce diabetic distress and improve glycemic control4,5 nationalcooperativerx.com PRESCRIPTION TREATMENTS -

IP Vol.2 No.2 Jul-Dec 2014.Pmd
International Physiology63 Short Communication Vol. 2 No. 2, July - December 2014 Role of Polyol Pathway in Pathophysiology of Diabetic Peripheral Neuropathy: An Updated Overview Kumar Senthil P.*, Adhikari Prabha**, Jeganathan*** Abstract The aim of this short communication article was to enlighten the role of polyol pathway in pathophysiology of diabetic peripheral neuropathy (DPN) through an evidence-informed overview of current literature. Findings from experimental models of DPN suggest that altered glutathione redox state, with exaggerated NA(+)-K(+)-ATPase activity, increased malondialdehyde content, decreased red blood cell 2,3-diphosphoglycerate concentration, reduced cyclic adenosine monophosphate, reduced myo- inositol and excessive sorbitol in peripheral nerves were indicative of polyol metabolic pathwayin producing pathophysiological changes of DPN, and treatments using aldose reductase inhibitors were found to reverse those changes. Keywords: Polyol pathway; Myo-inositol; Sorbitol; Neurophysiology; Endocrinology. The aim of this short communication oxidized (GSSG) glutathione levels in crude article was to enlighten the role of polyol homogenates of rat sciatic nerve. The study pathway in pathophysiology of diabetic concluded that altered glutathione redox peripheral neuropathy (DPN) through an state played no detectable role in the evidence-informed overview of current pathogenesis of this defect in diabetic literature. peripheral nerve. Calcutt et al[1] measured motor nerve Finegold et al[3] studied the effect of conduction velocity (MNCV), Na(+)-K(+)- polyol pathway blockade with sorbinil, a ATPase activity, polyol-pathway specific inhibitor of aldose reductase, on metabolites, and myo-inositol in sciatic nerve myo-inositol content in acutely nerves from control mice, galactose-fed streptozotocin-diabetic ratswhich (20% wt/wt diet) mice, and galactose-fed completely prevented the fall in nerve myo- mice given the aldose reductase inhibitor inositol. -

295-304 Research Article Pulsatile Drug Delivery of Chitosan Co
Available online www.jocpr.com Journal of Chemical and Pharmaceutical Research, 2015, 7(12):295-304 ISSN : 0975-7384 Research Article CODEN(USA) : JCPRC5 Pulsatile drug delivery of chitosan coated beads of miglitol with fast dissolving glimepiride tablet Bhise S. H.*, Surve B. S., Aloorkar N. H., Majumdar S. H. and Kulkarni A. S. Department of Pharmaceutics, Satara College of Pharmacy, Satara, Shivaji University, Maharashtra, India _____________________________________________________________________________________________ ABSTRACT : Pulsatile drug delivery system was developed which have three parts fast dissolving tablet of glimepiride, sustained release chitosan coated microbeads of miglitol and plug of HPMC E5 and spray dried lactose. After pre- formulation studies fast dissolving tablets were prepared by direct compression method; which shows instant drug release and % CDR of glimepiride fast dissolving tablet was found to be 70.81%. polymer plug have lag time 2.30 hr, chitosan coated miglitol beads shows sustained release upto 81.66% .this system is evaluated using different physicochemical parameters and in-vitro studies. Result suggests that the system can be applicable for diabetes treatment. Key words: Pulsatile, microbeads, sustained release, miglitol, glimepiride. _____________________________________________________________________________________________ INTRODUCTION Oral controlled drug delivery systems represent the most popular form of controlled drug delivery system which release the drug with constant or variable release rates.[1] Dose of drug, reduced dosage frequency, avoidance of side effects, and improved patient compliance. However, there are certain conditions for which such a release pattern is not suitable. These conditions demand release of drug after a lag time. In other words, it is required that the drug should not be released at all during the initial phase of dosage form administration. -

Effect of the Α-Glucosidase Inhibitor Miglitol on the Glucose Profile in Japanese Type 2 Diabetic Patients Receiving Multiple Daily Insulin Injections
Endocrine Journal 2012, 59 (4), 345-352 ORIGINAL Effect of the α-glucosidase inhibitor miglitol on the glucose profile in Japanese type 2 diabetic patients receiving multiple daily insulin injections Hiroyuki Kato, Akio Ohta, Suzuko Kobayashi, Satoshi Ishii, Yukiyoshi Sada, Hidetoshi Kobayashi, Shintaro Ohmori, Akihiko Kondo, Takuyuki Katabami, Junro Fuse, Hisashi Fukuda, Yoshio Nagai and Yasushi Tanaka Department of Internal Medicine, Division of Metabolism and Endocrinology, St. Marianna University School of Medicine, Kawasaki 216-8511, Japan Abstract. Strict postprandial glycemic control may have a preventive effect on atherogenesis in patients with type 2 diabetes. The α-glucosidase inhibitor (α-GI) miglitol is useful for controlling the early postprandial increase of glucose, but the combined effect of miglitol and multiple daily insulin injections (MDI) on glucose excursion has not been evaluated. First, we retrospectively compared the daily glucose profile, evaluated by self-monitoring of blood glucose (SMBG) at nine times on the day before discharge from hospital, between type 2 diabetic patients receiving MDI (n=81) or MDI plus miglitol at 150 mg daily (n=24). Second, we prospectively examined the effect of adding miglitol to MDI on the daily glucose profile (SMBG) in 19 other type 2 diabetic patients. Although the daily insulin dosage and the glucose level before meals did not differ between the two groups, the 1-h postprandial glucose level after each meal, 2-h glucose level after lunch and dinner, mean and standard deviation of glucose, and amplitude of glucose excursion were significantly lower or smaller in the MDI plus miglitol group than in the MDI group. -

Hypoglycemia in Diabetes: Common, Often Unrecognized
REVIEW ILAN GABRIELY, MD HARRY SHAMOON, MD CME Diabetes Research Center, Albert Einstein Professor of Medicine, Diabetes Research CREDIT College of Medicine, New York Center, Albert Einstein College of Medicine, New York Hypoglycemia in diabetes: Common, often unrecognized ■ ABSTRACT YPOGLYCEMIA poses a major barrier to H diabetes treatment. On one hand, we Hypoglycemic episodes in patients with diabetes often go want to maintain tight glycemic control to unrecognized, and over time, patients may lose the ability prevent the vascular complications of diabetes, to sense hypoglycemia, increasing their risk. Intensive but we also have to ensure the safety and com- diabetes control is beneficial for patients with diabetes, fort of the patient by avoiding hypoglycemia— but it increases their risk of hypoglycemia, underscoring and by recognizing and treating it if it occurs. the complexity of diabetes management. Hypoglycemic events are probably com- mon, especially in patients with type 1 diabetes. ■ KEY POINTS And when patients with type 2 diabetes receive insulin, they may become more prone to hypo- Epinephrine release during hypoglycemia becomes glycemic episodes. Unfortunately, the more progressively defective in type 1 diabetes. This decrease in episodes of hypoglycemia a patient has, the epinephrine response is accompanied by an attenuated more the body’s response is blunted, decreasing autonomic neural response, which results in the clinical the patient’s awareness of an episode. syndrome of impaired awareness of hypoglycemia (ie, Thus, we need to be vigilant in monitor- lack of the warning symptoms of prevailing ing patients for increasing episodes of hypo- glycemia, and for events that a patient may not hypoglycemia). -

Women with Higher BMI at Lower Risk for Glaucoma
44 WOMEN'S HEALTH SEPTEMBER 1, 2010 • FAMILY PRACTICE NEWS DRUGS, PREGNANCY, AND LACTATION Use of Antidiabetic Agents During Pregnancy n a previous column, I looked at the abinese), tolazamide (Tolinase), and tolbu- thetic analogue of human amylin given was discovered. No developmental toxi- ways uncontrolled hyperglycemia tamide (Orinase). They can cause marked by subcutaneous injection, but the ani- city was observed in the newborns. Iduring pregnancy causes significant and persistent neonatal hypoglycemia if mal data suggest moderate risk (struc- Pioglitazone (Actos) and rosiglitazone toxicity for the mother, embryo, fetus, taken close to birth. To prevent this toxi- tural anomalies in rats). The drug— (Avandia), thiazolidinediones used as ad- newborn, and adolescent (“Toxicity of city, therapy should be changed to insulin which slows the rate of gastric emptying, juncts to diet and exercise, lower insulin Diabetes in Pregnancy,” December in the third trimester or, at least, several prevents a postprandial rise in plasma resistance but do not promote insulin re- 2009, p. 52). days before birth. glucagon, and promotes satiety—is best lease. Animal reproduction data suggest This column examines the The second-generation sul- avoided in pregnancy. risk, but the human experience is too use of antidiabetic agents, fonylureas glipizide (Glu- Saxagliptin (Onglyza) and sitagliptin limited to assess the risk, so they should other than insulin, that are cotrol), glimepiride (Amaryl), (Januvia), inhibitors of the enzyme be avoided in pregnancy. used for non–insulin-depen- and glyburide (DiaBeta, Gly- dipeptidyl peptidase–4, are indicated as In summary, only metformin and gly- dent diabetes during preg- nase, and Micronase) are pre- monotherapy or in combination with buride have sufficient human pregnancy nancy and lactation. -

Review of Nisha Amalaki –An Ayurvedic Formulation of Turmeric and Indian Goose Berry in Diabetes
wjpmr, 2017,3(9), 101-105 SJIF Impact Factor: 4.103 Review Article Bedarkar. WORLD JOURNAL OF PHARMACEUTICAL World Journal of Pharmaceutical and Medical Research AND MEDICAL RESEARCH ISSN 2455-3301 www.wjpmr.com WJPMR REVIEW OF NISHA AMALAKI –AN AYURVEDIC FORMULATION OF TURMERIC AND INDIAN GOOSE BERRY IN DIABETES Dr. Prashant Bedarkar* Assistant Prof. Dept. of Rasashastra and B.K., IPGT & R. A., Jamnagar, Gujarat, India. *Corresponding Author: Dr. Prashant Bedarkar Assistant Prof. Dept. of Rasashastra and B.K., IPGT & R. A., Jamnagar, Gujarat, India. Article Received on 01/08/2017 Article Revised on 22/08/2017 Article Accepted on 12/09/2017 ABSTRACT Introduction- Nishamalaki or Nisha Amalaki representing various combination formulations of Turmeric (Nisha, Haridra, Curcuma longa L.) and Indian gooseberry (Amalaki, Emblica officinalis Gaertn.) is recommended in Ayurvedic classics, proven efficacious and widely practiced in the management i.e. treatment of Diabetes along with management and prevention of complications of Madhumeha (Diabetes). Aims and objectives-Inspite of many pharmacological, clinical researches of Nishamalaki on Glucose metabolism and Glycemic control, their review is not available, hence present study was conducted. Material and methods- Evidence based online published researches of Nishamalaki on Glucose metabolism and Glycemic control and its efficacy in the management of complications of Diabetes from available databases and search engines were referred for review through. Summary of published researches was systematically arranged, analyzed and presented. Observations and results-Review of online Published original research studies reveals total were found to be 13 in number, comprising of 3 in vitro studies and animal experimental pharmacological researches each and 7 clinical researches. -

Evaluation of Effect of Nishamalaki on STZ and HFHF Diet Induced Diabetic
DOI: 10.7860/JCDR/2016/21011.8752 Experimental Research Evaluation of Effect of Nishamalaki on STZ and HFHF Diet Induced Diabetic Pharmacology Section Neuropathy in Wistar Rats JAYSHREE SHRIRAM DAWANE1, VIJAYA ANIL PANDIT2, MADHURA SHIRISH KUMAR BHOSALE3, PALLAWI SHASHANK KHATAVKAR4 ABSTRACT Pioglitazone and Epalrestat. Animals received drug treatment Introduction: Diabetic neuropathy is one of the most common for next 12 weeks. Monitoring of Blood Sugar Level (BSL) done complications affecting 50% of diabetic patients. Neuropathic every 15 days and lipid profile at the end. Eddy’s hot plate and pain is the most difficult types of pain to treat. There is no specific tail immersion test performed to assess thermal hyperalgesia treatment for neuropathy. Nishamalaki (NA), combination of and cold allodynia. Walking function test performed to assess Curcuma longa and Emblica officinalis used to treat Diabetes motor function. Mellitus (DM). So, efforts were made to test whether NA is useful Results: Diabetic rats exhibited significant (p<0.001) hyperal- in prevention of diabetic neuropathy. gesia and increased BSL compared to control rats. Dose- Aim: To evaluate the effect of NA on diabetic neuropathy in type dependent improvement was observed in thermal hyperalgesia 2 diabetic wistar rats. & cold allodynia in NA groups. Activity of NA was more than Glibenclamide, Epalrestat and Pioglitazone in high dose and Materials and Methods: Group I (Control) vehicle treated comparable in low dose. Nishamalaki improved lipid profile. consists of 6 rats. Diabetes induced in 36 wistar rats with Streptozotocin (STZ) (35mg/kg) intra-peritoneally followed by Conclusion: Apart from controlling hyperglycaemia and High Fat High Fructose diet. -

Comparative Review of Oral Hypoglycemic Agents in Adults
SECTION 18.5 Comparative Review of Oral Hypoglycemic Agents in Adults Harinder Chahal For WHO Secretariat Table of Contents Acronyms: ............................................................................................................................................................................... 3 I. Background and Rationale for the review: ....................................................................................................................... 4 II. Medications under comparative review: ......................................................................................................................... 4 Table 1 - New oral hypoglycemic agents for comparison with current EML agents .......................................................... 5 III. Literature searches and methodology: ............................................................................................................................ 5 1. Title Search Results: .................................................................................................................................................... 6 2. Statement about quality of evidence: ........................................................................................................................ 6 IV. Clinical efficacy and safety evaluation: ............................................................................................................................ 6 1. DPP-4 Inhibitors (Sitagliptin, Saxagliptin) and Metformin: ........................................................................................ -

Oral Health Fact Sheet for Dental Professionals Adults with Type 2 Diabetes
Oral Health Fact Sheet for Dental Professionals Adults with Type 2 Diabetes Type 2 Diabetes ranges from predominantly insulin resistant with relative insulin deficiency to predominantly an insulin secretory defect with insulin resistance, American Diabetes Association, 2010. (ICD 9 code 250.0) Prevalence • 23.6 million Americans have diabetes – 7.8% of U.S. population. Of these, 5.7 million do not know they have the disease. • 1.6 million people ≥20 years of age are diagnosed with diabetes annually. • 90–95% of diabetic patients have Type 2 Diabetes. Manifestations Clinical of untreated diabetes • High blood glucose level • Excessive thirst • Frequent urination • Weight loss • Fatigue Oral • Increased risk of dental caries due to salivary hypofunction • Accelerated tooth eruption with increasing age • Gingivitis with high risk of periodontal disease (poor control increases risk) • Salivary gland dysfunction leading to xerostomia • Impaired or delayed wound healing • Taste dysfunction • Oral candidiasis • Higher incidence of lichen planus Other Potential Disorders/Concerns • Ketoacidosis, kidney failure, gastroparesis, diabetic neuropathy and retinopathy • Poor circulation, increased occurrence of infections, and coronary heart disease Management Medication The list of medications below are intended to serve only as a guide to facilitate the dental professional’s understanding of medications that can be used for Type 2 Diabetes. Medical protocols can vary for individuals with Type 2 Diabetes from few to multiple medications. ACTION TYPE BRAND NAME/GENERIC SIDE EFFECTS Enhance insulin Sulfonylureas Glipizide (Glucotrol) Angioedema secretion Glyburide (DiaBeta, Fluconazoles may increase the Glynase, Micronase) hypoglycemic effect of glipizide Glimepiride (Amaryl) and glyburide. Tolazamide (Tolinase, Corticosteroids may produce Diabinese, Orinase) hyperglycemia. Floxin and other fluoroquinolones may increase the hypoglycemic effect of sulfonylureas. -
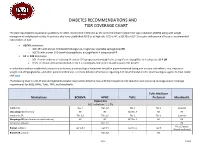
Diabetes Recommendations and Tier Coverage Chart
DIABETES RECOMMENDATIONS AND TIER COVERAGE CHART The American Diabetes Association guidelines for 2020, recommend metformin as the preferred initial treatment for type 2 diabetes (T2DM) along with weight management and physical activity. In patients who have established ASVD or at high risk, CKD, or HF, a SGLT2i or GLP-1 receptor with proven efficacy is recommended independent of A1C. • ASCVD dominates: o GLP-1RA with proven CVD benefit (dulaglutide, liraglutide, injectable semaglutide) OR o SGLT2i with proven CVD benefit (canagliflozin, empagliflozin) if adequate eGFR • HF or CKD dominates: o SGLT2i with evidence of reducing HF and/or CKD progression (empagliflozin, canagliflozin, dapagliflozin) if adequate eGFR OR o If SGLT2i intolerant/contraindicated or eGFR is inadequate, then GLP-1RA with proven CVD benefit In individuals without established cardiovascular disease, pharmacological treatment should be patient-centered taking into account side-effects, cost, impact on weight, risk of hypoglycemia, and other patient preferences. For more detailed information regarding ADA recommendations for pharmacological agents to treat T2DM click here. The following chart is a list of oral and injectable diabetes medications listed by class with their respective A1C reduction and insurance coverage and/or coverage requirements for BCBS, HPHC, Tufts, TMP, and MassHealth. Tufts Medicare Medications BCBSMA HPHC Tufts Preferred MassHealth Biguanides A1C reduction: 1-1.5% metformin Tier 1 Tier 1;2 Tier 1 Tier 1 Covered Glucoghage (metformin) NC NC NC;Tier -

The Synergistic Effect of Miglitol Plus Metformin Combination Therapy in the Treatment of Type 2 Diabetes
Clinical Care/Education/Nutrition ORIGINAL ARTICLE The Synergistic Effect of Miglitol Plus Metformin Combination Therapy in the Treatment of Type 2 Diabetes 1 JEAN-LOUIS CHIASSON, MD The recently developed class of 2 LISA NADITCH, MD ␣-glucosidase inhibitors has a unique FOR THE MIGLITOL CANADIAN UNIVERSITY mode of action; it blocks oligosaccharide INVESTIGATOR GROUP catabolism, delays carbohydrate diges- tion and absorption, and smooths and lowers postprandial plasma blood glu- cose peaks (6–9). Substantial evidence supports their use as monotherapy or ad- OBJECTIVE — To investigate the efficacy and safety of miglitol in combination with met- junct therapy for poorly controlled type 2 formin in improving glycemic control in outpatients in whom type 2 diabetes is insufficiently diabetes (5,10–14). Miglitol is the first controlled by diet alone. pseudomonosaccharide ␣-glucosidase in- RESEARCH DESIGN AND METHODS — In this multicenter, double-blind, placebo- hibitor derived from 1-deoxynojirimycin controlled study, 324 patients with type 2 diabetes were randomized, after an 8-week placebo and is structurally a glucose analog run-in period, to treatment with either placebo, miglitol alone, metformin alone, or miglitol plus (15,16). Its efficacy in monotherapy metformin for 36 weeks. The miglitol was titrated to 100 mg three times a day and metformin was (13,17) and in combination with sulfo- administered at 500 mg three times a day. The primary efficacy criterion was change in HbA1c nylureas (11) as a glucose-lowering agent from baseline to the end of treatment. Secondary parameters included changes in fasting and in type 2 diabetes has been shown in a postprandial plasma glucose and insulin levels, serum triglyceride levels, and responder rate.