4-Tier Preferred Drug List
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Molecular Mechanisms Underlying Ketamine-Mediated Inhibition Of
Anesthesiology 2005; 102:93–101 © 2004 American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins, Inc. Molecular Mechanisms Underlying Ketamine-mediated Inhibition of Sarcolemmal Adenosine Triphosphate- sensitive Potassium Channels Takashi Kawano, M.D.,* Shuzo Oshita, M.D.,† Akira Takahashi, M.D.,‡ Yasuo Tsutsumi, M.D.,* Katsuya Tanaka, M.D.,§ Yoshinobu Tomiyama, M.D., Hiroshi Kitahata, M.D.,# Yutaka Nakaya, M.D.** Background: Ketamine inhibits adenosine triphosphate-sen- sensitive channel pore.3 These channels, as metabolic sitive potassium (KATP) channels, which results in the blocking sensors, are associated with such cellular functions as of ischemic preconditioning in the heart and inhibition of va- insulin secretion, cardiac preconditioning, vasodilata- sorelaxation induced by KATP channel openers. In the current 4–7 Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/102/1/93/357819/0000542-200501000-00017.pdf by guest on 27 September 2021 study, the authors investigated the molecular mechanisms of tion, and neuroprotection. ketamine’s actions on sarcolemmal KATP channels that are re- In cardiac myocytes, intravenous general anesthetics, associated by expressed subunits, inwardly rectifying potas- such as ketamine racemate, propofol, and thiamylal, di- sium channels (Kir6.1 or Kir6.2) and sulfonylurea receptors 8–10 rectly inhibit native sarcolemmal KATP channels. Al- (SUR1, SUR2A, or SUR2B). though these observations suggest that intravenous an- Methods: The authors used inside-out patch clamp configura- tions to investigate the effects of ketamine on the activities of esthetics may impair the endogenous organ protective reassociated Kir6.0/SUR channels containing wild-type, mutant, mechanisms mediated by KATP channels, the possibility or chimeric SURs expressed in COS-7 cells. -

Iatrogenic Misadventure
BRITISH MEDICAL JOURNAL 18 MARcH 1972 733 Scientific Basis of Clinical Practice Br Med J: first published as 10.1136/bmj.1.5802.733 on 18 March 1972. Downloaded from Iatrogenic Misadventure A. G. W. WHITFIELD British Medical journal, 1972, 1, 733-734 effects. No one would pretend that our knowledge of drugs interacting with oral anticoagulants is complete. Even so, A striking feature of the history of therapeutics is the extent to sufficient is already known to indicate that anticoagulant drugs which fashion, rather than clinical science, governs the treat- have potent dangers and should be used only within the limited ment we mete out to our patients. Some ten years ago I attended sphere in which they are of proven worth. Moreover, when they a symposium on anticoagulant therapy and returned home are given, if possible, no other drug should be given at the firmly convinced that in all but a very few conditions such same time as many are known to inhibit or enhance their effect treatment was absolutely essential and indeed it was little short and many others may have similar interactions, even though of criminal negligence to withhold it. At that time the patient these are as yet unrecognized and unreported. queue for "prothrombin times" was usually the longest in our hospitals and phenindione was among the most frequently prescribed drugs, but our constant use of it stemmed from enthusiasm and ignorance of its dangers and not from scientific Hypotensive Drugs proof of its therapeutic advantages. Indeed it is only as know- Hypotensive drugs are being used increasingly and undoubtedly ledge has accumulated that we have learned of the toxic effects, their development has provided an enormous advance both in of the drug we gave so freely, on the kidney, the liver, the bone the treatment and in the prognosis of the severe forms of marrow, and the skin and that except in thromboembolic disease and in patients with hypertension-particularly in the younger age groups. -

Label-Free Cell Phenotypic Profiling Decodes the Composition And
OPEN Label-free cell phenotypic profiling SUBJECT AREAS: decodes the composition and signaling POTASSIUM CHANNELS SENSORS AND PROBES of an endogenous ATP-sensitive Received potassium channel 28 January 2014 Haiyan Sun1*, Ying Wei1, Huayun Deng1, Qiaojie Xiong2{, Min Li2, Joydeep Lahiri1 & Ye Fang1 Accepted 24 April 2014 1Biochemical Technologies, Science and Technology Division, Corning Incorporated, Corning, NY 14831, United States of Published America, 2The Solomon H. Snyder Department of Neuroscience and High Throughput Biology Center, Johns Hopkins University 12 May 2014 School of Medicine, Baltimore, Maryland 21205, United States of America. Current technologies for studying ion channels are fundamentally limited because of their inability to Correspondence and functionally link ion channel activity to cellular pathways. Herein, we report the use of label-free cell requests for materials phenotypic profiling to decode the composition and signaling of an endogenous ATP-sensitive potassium should be addressed to ion channel (KATP) in HepG2C3A, a hepatocellular carcinoma cell line. Label-free cell phenotypic agonist Y.F. (fangy2@corning. profiling showed that pinacidil triggered characteristically similar dynamic mass redistribution (DMR) com) signals in A431, A549, HT29 and HepG2C3A, but not in HepG2 cells. Reverse transcriptase PCR, RNAi knockdown, and KATP blocker profiling showed that the pinacidil DMR is due to the activation of SUR2/ Kir6.2 KATP channels in HepG2C3A cells. Kinase inhibition and RNAi knockdown showed that the pinacidil * Current address: activated KATP channels trigger signaling through Rho kinase and Janus kinase-3, and cause actin remodeling. The results are the first demonstration of a label-free methodology to characterize the Biodesign Institute, composition and signaling of an endogenous ATP-sensitive potassium ion channel. -

(12) Patent Application Publication (10) Pub. No.: US 2015/0202317 A1 Rau Et Al
US 20150202317A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0202317 A1 Rau et al. (43) Pub. Date: Jul. 23, 2015 (54) DIPEPTDE-BASED PRODRUG LINKERS Publication Classification FOR ALPHATIC AMNE-CONTAINING DRUGS (51) Int. Cl. A647/48 (2006.01) (71) Applicant: Ascendis Pharma A/S, Hellerup (DK) A638/26 (2006.01) A6M5/9 (2006.01) (72) Inventors: Harald Rau, Heidelberg (DE); Torben A 6LX3/553 (2006.01) Le?mann, Neustadt an der Weinstrasse (52) U.S. Cl. (DE) CPC ......... A61K 47/48338 (2013.01); A61 K3I/553 (2013.01); A61 K38/26 (2013.01); A61 K (21) Appl. No.: 14/674,928 47/48215 (2013.01); A61M 5/19 (2013.01) (22) Filed: Mar. 31, 2015 (57) ABSTRACT The present invention relates to a prodrug or a pharmaceuti Related U.S. Application Data cally acceptable salt thereof, comprising a drug linker conju (63) Continuation of application No. 13/574,092, filed on gate D-L, wherein D being a biologically active moiety con Oct. 15, 2012, filed as application No. PCT/EP2011/ taining an aliphatic amine group is conjugated to one or more 050821 on Jan. 21, 2011. polymeric carriers via dipeptide-containing linkers L. Such carrier-linked prodrugs achieve drug releases with therapeu (30) Foreign Application Priority Data tically useful half-lives. The invention also relates to pharma ceutical compositions comprising said prodrugs and their use Jan. 22, 2010 (EP) ................................ 10 151564.1 as medicaments. US 2015/0202317 A1 Jul. 23, 2015 DIPEPTDE-BASED PRODRUG LINKERS 0007 Alternatively, the drugs may be conjugated to a car FOR ALPHATIC AMNE-CONTAINING rier through permanent covalent bonds. -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine -

USP–NF 2021, Issue 1 Commentary
Commentary USP–NF 2021 Issue 1 November 2, 2020 In accordance with USP’s Rules and Procedures of the Council of Experts (“Rules”), and except as provided in Section 9.02 Accelerated Revision Processes, USP publishes proposed revisions to the United States Pharmacopeia and the National Formulary (USP–NF) for public review and comment in the Pharmacopeial Forum (PF), USP’s free bimonthly journal for public notice and comment. After comments are considered and incorporated as the Expert Committee deems appropriate, the proposal may advance to official status or be re-published in PF for further notice and comment, in accordance with the Rules. In cases when proposals advance to official status, a summary of comments received and the appropriate Expert Committee's responses, as well as Expert Committee-initiated changes, are published in the Proposal Status/Commentary section of USPNF.com at the time the official revision is published. The Commentary is not part of the official text and is not intended to be enforceable by regulatory authorities. Rather, it explains the basis of Expert Committees’ responses to public comments on proposed revisions. If there is a difference or conflict between the contents of the Commentary and the official text, the official text prevails. For further information, contact: USP Executive Secretariat United States Pharmacopeia 12601 Twinbrook Parkway Rockville, MD 20852-1790 USA Commentary for USP–NF 2021, Issue 1 Comments were received for the following when they were proposed in Pharmacopeial Forum: General -
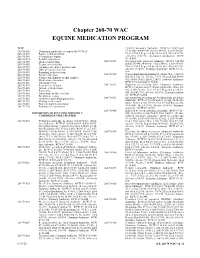
Chapter 260-70 WAC EQUINE MEDICATION PROGRAM
Chapter 260-70 Chapter 260-70 WAC EQUINE MEDICATION PROGRAM WAC 12/6/93. Statutory Authority: RCW 67.16.020 and 260-70-500 Definitions applicable to chapter 260-70 WAC. 67.16.040. 84-06-061 (Order 84-01), § 260-70-028, 260-70-510 Equine health and safety. filed 3/7/84.] Repealed by 96-10-001, filed 4/17/96, 260-70-540 Veterinarians' reports. effective 5/18/96. Statutory Authority: RCW 260-70-545 Prohibited practices. 67.16.040. 260-70-550 Medication labeling. 260-70-029 Receiving barn. [Statutory Authority: RCW 67.16.020 260-70-560 Treatment restrictions. and 67.16.040. 84-06-061 (Order 84-01), § 260-70-029, 260-70-570 All horses are subject to inspection. filed 3/7/84.] Repealed by 96-10-001, filed 4/17/96, 260-70-580 Official veterinarian's list. effective 5/18/96. Statutory Authority: RCW 67.16.- 260-70-590 Reporting to the test barn. 040. 260-70-600 Sample collection. 260-70-030 When administration prohibited. [Order 74.1, § 260-70- 260-70-610 Storage and shipment of split samples. 030, filed 5/22/74, effective 7/1/74.] Repealed by 80-01- 260-70-620 Medication restrictions. 072 (Order 79-02), filed 12/24/79. Statutory Authority: 260-70-630 Threshold levels. RCW 67.16.020 and 67.16.040. 260-70-640 Permitted medication. 260-70-031 Reporting to receiving barn. [Statutory Authority: 260-70-645 Anti-ulcer medications. RCW 67.16.020 and 67.16.040. 84-06-061 (Order 84- 260-70-650 Furosemide. -

Pharmacy Program Updates: Quarterly Pharmacy Changes Effective Jan
Pharmacy Program Updates: Quarterly Pharmacy Changes Effective Jan. 1, 2020 – Part 2 This article is a continuation of the previously published Quarterly Pharmacy Changes Part 1 article. While that part 1 article included the drug list revisions/exclusions, dispensing limits, utilization management changes and general information on pharmacy benefit program updates, this part 2 version contains the more recent coverage additions, utilization management updates and any other updates to the pharmacy program. DRUG LIST CHANGES Based on the availability of new prescription medications and Prime’s National Pharmacy and Therapeutics Committee’s review of changes in the pharmaceuticals market, some additions (new to coverage) and/or some coverage tier changes (drugs moved to a lower out-of-pocket payment level) will be made to the Blue Cross and Blue Shield of New Mexico (BCBSNM) drug lists. Please note: Revisions (drugs still covered but moved to a higher out-of-pocket payment level) and/or exclusions (drugs no longer covered) were included in the Quarterly Pharmacy Changes Part 1 article. Your patient(s) may ask you about therapeutic or lower cost alternatives if their medication is affected by one of these changes. Changes effective Jan. 1, 2020 are outlined below. Drug List Coverage Additions – As of Jan. 1, 2020 Preferred Drug1 Drug Class/Condition Used For Basic, Multi-Tier Basic, Multi-Tier Basic Annual, Enhanced, Enhanced Annual, Multi-Tier Enhanced and Multi-Tier Enhanced Annual Drug Lists BELBUCA (buprenorphine hcl buccal film 75 mcg, -

CUSTOMS TARIFF - SCHEDULE 99 - I
CUSTOMS TARIFF - SCHEDULE 99 - i Chapter 99 SPECIAL CLASSIFICATION PROVISIONS - COMMERCIAL Notes. 1. The provisions of this Chapter are not subject to the rule of specificity in General Interpretative Rule 3 (a). 2. Goods which may be classified under the provisions of Chapter 99, if also eligible for classification under the provisions of Chapter 98, shall be classified in Chapter 98. 3. Goods may be classified under a tariff item in this Chapter and be entitled to the Most-Favoured-Nation Tariff or a preferential tariff rate of customs duty under this Chapter that applies to those goods according to the tariff treatment applicable to their country of origin only after classification under a tariff item in Chapters 1 to 97 has been determined and the conditions of any Chapter 99 provision and any applicable regulations or orders in relation thereto have been met. 4. The words and expressions used in this Chapter have the same meaning as in Chapters 1 to 97. Issued January 1, 2016 99 - 1 CUSTOMS TARIFF - SCHEDULE Tariff Unit of MFN Applicable SS Description of Goods Item Meas. Tariff Preferential Tariffs 9901.00.00 Articles and materials for use in the manufacture or repair of the Free CCCT, LDCT, GPT, UST, following to be employed in commercial fishing or the commercial MT, MUST, CIAT, CT, harvesting of marine plants: CRT, IT, NT, SLT, PT, COLT, JT, PAT, HNT, Artificial bait; KRT: Free Carapace measures; Cordage, fishing lines (including marlines), rope and twine, of a circumference not exceeding 38 mm; Devices for keeping nets open; Fish hooks; Fishing nets and netting; Jiggers; Line floats; Lobster traps; Lures; Marker buoys of any material excluding wood; Net floats; Scallop drag nets; Spat collectors and collector holders; Swivels. -

Chloride Channels Regulate HIT Cell Volume but Cannot Fully Account for Swelling-Induced Insulin Secretion Tracie A
Chloride Channels Regulate HIT Cell Volume but Cannot Fully Account for Swelling-Induced Insulin Secretion Tracie A. Kinard,1 Paulette B. Goforth,1 Qing Tao,1 Mary E. Abood,1,4 Jeanette Teague,5 and Leslie S. Satin1,2,3 ؊ Insulin-secreting pancreatic islet -cells possess anion- ing Cl channels. This suggests that the proximal effects ؊ of swelling to regulate cell volume may be mediated by permeable Cl channels (ICl,islet) that are swelling-acti- ؊ vated, but the role of these channels in the cells is CLC-3 or a closely related Cl channel. Diabetes 50: unclear. The Cl؊ channel blockers 4,4-diisothiocyano- 992–1003, 2001 stilbene-2,2-disulfonic acid (DIDS) and niflumic acid were evaluated for their ability to inhibit ICl,islet in clonal -cells (HIT cells). Both drugs blocked the chan- nel, but the blockade due to niflumic acid was less hereas much is known about the respective voltage-dependent than the blockade due to DIDS. HIT roles of cations and membrane cation chan- cell volume initially increased in hypotonic solution and nels in islet function (1), by comparison, there was followed by a regulatory volume decrease (RVD). The addition of niflumic acid and, to a lesser extent, W is little detailed information available concern- DIDS to the hypotonic solution potentiated swelling ing the physiological role of anions or anion-handling mech- and blocked the RVD. In isotonic solution, niflumic acid anisms in islets. This is true even though it has been known produced swelling, suggesting that islet Cl؊ channels for some time that islets have glucose-sensitive anion fluxes are activated under basal conditions. -

Mitigating the Inhibition of Human Bile Salt Export Pump by Drugs
DMD Fast Forward. Published on September 7, 2012 as DOI: 10.1124/dmd.112.047068 DMD FastThis Forward. article has not Published been copyedited on andSeptember formatted. The 7, final 2012 version as doi:10.1124/dmd.112.047068may differ from this version. DMD #47968 Mitigating the inhibition of human Bile Salt Export Pump by drugs: opportunities provided by physicochemical property modulation, in-silico modeling and structural modification Daniel J. Warner, Hongming Chen, Louis-David Cantin, J. Gerry Kenna, Simone Stahl, Clare L. Walker, Tobias Noeske. Department of Medicinal Chemistry, AstraZeneca R&D Montreal, Montreal, Quebec, H4S Downloaded from 1Z9, Canada (DJW, LDC) Computational Sciences, Discovery Sciences, AstraZeneca R&D Mölndal, Pepparedsleden dmd.aspetjournals.org 1, Mölndal 43183, Sweden (HC) Molecular Toxicology, Global Safety Assessment, AstraZeneca, Alderley Park, Macclesfield, Cheshire, SK10 4TG, UK (JGK, SS, CLW) Global Safety Assessment, AstraZeneca R&D Mölndal, Pepparedsleden 1, Mölndal 43183, at ASPET Journals on October 10, 2021 Sweden (TN) 1 Copyright 2012 by the American Society for Pharmacology and Experimental Therapeutics. DMD Fast Forward. Published on September 7, 2012 as DOI: 10.1124/dmd.112.047068 This article has not been copyedited and formatted. The final version may differ from this version. DMD #47968 Inhibition of the human Bile Salt Export Pump by drugs. Corresponding author: Tobias Noeske Global Safety Assessment AstraZeneca R&D Mölndal S-431 83 Mölndal, Sweden Phone: +46-31-7064002 Mobile: +46-727-158344 -

THE ACTION of DIAZOXIDE on ISOLATED VASCULAR SMOOTH MUSCLE By
THE ACTION OF DIAZOXIDE ON ISOLATED VASCULAR SMOOTH MUSCLE by HAROLD JAMES RHODES B.A., University of British Columbia, 1965 A THESIS SUBMITTED IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE DEGREE OF Master of Science in the Department or Pharmacology We accept this thesis as conforming to the required standard THE UNIVERSITY OF BRITISH COLUMBIA October, 1969 In presenting this thesis in partial fulfilment of the requirements for an advanced degree at the University of British Columbia, I agree that the Library shall make it freely available for reference and Study. I further agree that permission for extensive copying of this thesis for scholarly purposes may be granted by the Head of my Department or by his representatives. It is understood that copying or publication of this thes,is for financial gain shall not be allowed without my written permission. Department of Pharmacology The University of British Columbia Vancouver 8, Canada Date ''i/h&fa^&r For Brenda il A preliminary report of this work was presented at The Canadian Fed• eration of Biological Sciences Meet• ing held in Edmonton, Alberta in June, 1969. iii ABSTRACT Diazoxide, a non-diuretic benzothiadiazlne antihypertensive agent, is thought to act directly upon the vascular smooth muscle of the resistance vessels to exert its therapeutic effects in hypertension. Diazoxide may exert its antihypertensive action by antagonizing calcium in vascular smooth muscle. Wohl e_t al. (196? and 1968) have suggested such an interaction based on experiments conducted with isolated rabbit aortae. The present experiments were designed to investigate the possible cellular locus of the postulated interaction of diazoxide with calcium using the iso• lated anterior mesenteric vein of the rabbit as a model of vas• cular smooth muscle.