THE ACUTE ABDOMEN Definition Abdominal Pain of Short Duration
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Perforated Ulcers Shaleen Sathe, MS4 Christina Lebedis, MD CASE HISTORY
Perforated Ulcers Shaleen Sathe, MS4 Christina LeBedis, MD CASE HISTORY 54-year-old male with known history of hypertension presents with 2 days of acute onset abdominal pain, nausea, vomiting, and diarrhea, with periumbilical tenderness and abdominal distention on exam, without guarding or rebound tenderness. Labs, including CBC, CMP, and lipase, were unremarkable in the emergency department. Radiograph Perforated Duodenal Ulcer Radiograph of the chest in the AP projection shows large amount of free air under diaphragm (blue arrows), suggestive of intraperitoneal hollow viscus perforation. CT Perforated Duodenal Ulcer CT of the abdomen in the axial projection (I+, O-), at the level of the inferior liver edge, shows large amount of intraperitoneal free air (blue arrows) in lung window (b), and submucosal edema in the gastric antrum and duodenal bulb (red arrows), suggestive of a diagnosis of perforated bowel, most likely in the region of the duodenum. US Perforated Gastric Ulcer US of the abdomen shows perihepatic fluid (blue arrow) and free fluid in the right paracolic gutter (not shown), concerning for intraperitoneal pathology. Radiograph Perforated Gastric Ulcer Supine radiograph of the abdomen shows multiple air- filled dilated loops of large bowel, with air lucencies on both sides of the sigmoid colon wall (green arrows), consistent with Rigler sign and perforation. CT Perforated Gastric Ulcer CT of the abdomen in the axial (a) and sagittal (b) projections (I+, O-) shows diffuse wall thickening of the gastric body and antrum (green arrows) with an ulcerating lesion along the posterior wall of the stomach (red arrows), and free air tracking adjacent to the stomach (blue arrow), concerning for gastric ulcer perforation. -

Emergent Repair of a Perforated Giant Duodenal Ulcer in a Patient with an Unmanaged Ulcer History
Open Access Case Report DOI: 10.7759/cureus.12198 Emergent Repair of a Perforated Giant Duodenal Ulcer in a Patient With an Unmanaged Ulcer History Eli B. Eisman 1, 2 , Nicole C. Jamieson 2 , Rashona A. Moss 3 , Melina M. Henderson 4 , Richard C. Spinale 2 1. College of Osteopathic Medicine, Michigan State University, East Lansing, USA 2. General Surgery, Garden City Hospital, Garden City, USA 3. Internal Medicine, Garden City Hospital, Garden City, USA 4. Obstetrics and Gynecology, Garden City Hospital, Garden City, USA Corresponding author: Eli B. Eisman, [email protected] Abstract Giant duodenal ulcers (GDUs) are full-thickness disruptions of the gastrointestinal epithelium greater than 3cm in diameter. The significant size and disease chronicity lead to deleterious outcomes and high mortality risk if ulcer progression is not halted. While still prevalent in developing countries, GDUs are increasingly rare in industrialized nations. Here, we present the case of an 82-year-old woman with perforated GDU requiring emergent surgical intervention complicated by prior duodenal surgery requiring a previously unreported triple-layered omental patch. Discussion of this technique and novel approaches to GDU repair ensue. Categories: Internal Medicine, Gastroenterology, General Surgery Keywords: complicated peptic ulcer disease, duodenal ulcers, duodenal ulceration, perforated duodenal ulcer, gastrointestinal perforation, chronic ulcer, graham patch repair Introduction Giant duodenal ulcers (GDUs) were first characterized in 1931, though initially difficult to diagnose on barium study due to the mistaken identification of ulcers as deformed duodenal caps [1]. Nussbaum and Schusterman codified GDUs as full-thickness ulcers greater than 2cm, usually involving but not limited to the duodenal bulb [2]. -

Perforated Peptic Ulcer: Different Ethnic, Climatic and Fasting Risk Factors for Morbidity in Al-Ain Medical District, United Arab Emirates
Original Article Perforated Peptic Ulcer: Different Ethnic, Climatic and Fasting Risk Factors for Morbidity in Al-Ain Medical District, United Arab Emirates Fawaz Chikh Torab, Mohamed Amer, Fikri M. Abu-Zidan and Frank James Branicki, Department of Surgery, Faculty of Medicine & Health Sciences, UAE University, UAE. AIM: To evaluate risk factors, morbidity and mortality rates of perforated peptic ulcer (PPU) and to inves- tigate factors affecting postoperative complications of PPU. BACKGROUND: The incidence of PPU has remained constant, simple closure with omental patch repair being the mainstay of treatment. PATIENTS AND METHODS: One hundred and nineteen patients admitted to Al-Ain Hospital with PPU between January 2000 and March 2004 was studied retrospectively; two with deficient data were excluded from the analysis. Logistic regression was used to define factors affecting postoperative complications. RESULTS: The mean age of patients was 35.3 years (range, 20–65). 45.7% of patients were Bangladeshi, and 85.3% originated from the Indian subcontinent. One patient, subsequently found to have a perfo- rated gastric cancer, died. In 116 patients, 26 complications were recorded in 20 patients (17.2%). Common risk factors for perforation were smoking, history of peptic ulcer disease (PUD) and use of non-steroidal anti-inflammatory drugs (NSAIDs). A significantly increased risk of perforation was evident during the daytime fasting month of Ramadan. An increase in the acute physiology and chronic health evaluation (APACHE) II score (p = 0.047) and a reduced white blood cell count (0.04) were highly significant for the prediction of postoperative complications. CONCLUSION: Patients with dyspeptic symptoms and a history of previous PUD should be considered for prophylactic treatment to prevent ulcer recurrence during prolonged daytime fasting in Ramadan, especially during the winter time. -
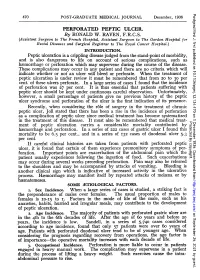
PERFORATED PEPTIC ULCER. Patient Usually Experiences
Postgrad Med J: first published as 10.1136/pgmj.12.134.470 on 1 December 1936. Downloaded from 470 POST-GRADUATE MEDICAL JOURNAL December, 1936 PERFORATED PEPTIC ULCER. By RONALD W. RAVEN, F.R.C.S. (Assistant Surgeon to T'he French Hospital, Assistant Surgeon to The Gordon Hospital for Rectal Diseases and Swrgical Registrar to The Royal Cancer Hospital.) INTRODUCTION. Peptic ulceration is a crippling disease judged from the stand-point of morbidity, and is also dangerous to life on account of serious complications, such as haemorrhage or perforation which may supervene during the course of the disease. These complications may occur in any patient and there are no criteria which will indicate whether or not an ulcer will bleed or perforate. When the treatment of peptic ulceration is under review it must be remembered that from 20 to 30 per cent. of these ulcers perforate. In a large series of cases I found that the incidence of perforation was 27 per cent. It is thus essential that patients suffering with peptic ulcer should be kept under continuous careful observation. Unfortunately, however, a small percentage of patients give no previous history of the peptic ulcer syndrome and perforation of the ulcer is the first indication of its presence. Recently, when considering the role of surgery in the treatment of chronic peptic ulcer, Joll stated that there has been a rise in the incidence of perforation as a complication of peptic ulcer since medical treatment has become systematized in the treatment of this disease. It must also be remembered that medical treat- Protected by copyright. -
Managing Envenomations
ResidentOfficial Publication of the Emergency Medicine Residents’ Association June/July 2021 VOL 48 / ISSUE 3 Managing Envenomations How to Sustain a Career: Peer Support Guide to ABEM Certi ication We Help Healers SCP Reach New Heights Health Meet Your Medical Career Dream Team SCP Health Step Right Up, Residents! As you’re transitioning from residency to begin your career, our team is here to create a tailored environment for you that fosters growth and delivers rewarding daily work experiences. Explore clinical careers at scp-health.com/explore TOGETHER, WE HEAL Welcome to a New Academic Year! uly marks a turning point each year, as new interns arrive in programs throughout Jthe country, newly graduated residents launch the next phase of their careers, and medical students take the next steps in their journey to residency. DO YOU KNOW HOW EMRA CAN HELP? Resources for Interns Resources for PGY2+ Resources for Students All EM programs will receive EMRA residents members receive the EMRA shows up for medical students Intern Kits this summer with nearly 10-pound EMRA Resident Kit upon interested in this specialty. From resources that offer immediate first joining EMRA. It is packed with clinical new advising content every month to backup for those first nerve-wracking resources for every rotation — some you’ll opportunities for leadership and growth, shifts. The high-yield EMRA Intern need only rarely (but prove to be clutch), and EMRA student membership is high-yield. Kit is sent for free to all EM interns some you’ll use every single shift (EMRA Plus, our online resources are unparalleled: (membership not required) and Antibiotic Guide, anyone?). -

Historical Note
East African Orthopaedic Journal HISTORICAL NOTE AMBROISE PARE 1510-1590 Pare was born in 1510 in Bourge-Hersent in North- were failing to emerge from the gums due to lack of West France. He initially worked with his brother who a pathway, and this failure was a cause of death. This was a surgeon cum barber. He practiced at Hotel Dieu, belief and practice persisted for centuries, with some Frances oldest Hospital. He was an anatomist and exceptions, until towards the end of the nineteenth invented several surgical instruments. He became a century lancing became increasingly controversial and war injury doctor at Piedmont where he used boiled oil was then abandoned (2). for treating gunshot wounds. One day he improvised In 1567, Ambroise Pare described an experiment using oil of roses, egg white and turpentine with very to test the properties of bezor stones. At the time, the good results. Henceforth he stopped the cauterization stones were commonly believed to be able to cure and hot oil method. the effects of any poison, but Pare believed this to be Pare was a keen observer and did not allow the impossible. It happened that a cook at Pare court was beliefs of the day to supersede the evidence at hand. In caught stealing fine silver cutlery, and was condemned his autobiographical book, Journeys in Diverse Places, to be hanged. The cook agreed to be poisoned, on the Pare inadvatienty practiced the scientific method when conditions that he would be given a bezoar straight he returned the following morning to a battlefield. -

Dentistry – Surgery IV Year
Dentistry – Surgery IV year Which sign is not associated with peptic ulcer perforation: A 42-year-old male, with previous Sudden onset ulcer history and typical clinical picture of peptic ulcer perforation, on Cloiberg caps examination, in 4 hours after the Positive Blumberg sign beginning of the disease, discomfort in Free air below diaphragm on plain right upper quadrant, heart rate - abdominal film 74/min., mild abdominal wall muscles rigidity, negative Blumberg sign. Free Intolerable abdominal pain air below diaphragm on X-ray abdominal film. What is you diagnosis? Which ethiological factors causes Peptic ulcer recurrence peptic ulcer disease most oftenly? Acute cholecystitis Abdominal trauma, alimentary factor Chronic cholecystitis H. pylori, NSAID's Covered peptic ulcer perforation H. pylori, hyperlipidemia Acute appendicitis (subhepatic Drugs, toxins location) NSAID's, gastrinoma Most oftenly perforated peptic ulcers are located at: A 30-year-old male is operated on for peptic ulcer perforation, in 2,5 hours Posterior wall of antrum after the beginning of the disease. Fundus of stomach Which operation will be most efficient (radical operation for peptic ulcer)? Cardiac part of stomach Simple closure and highly selective Posterior wall of duodenal bulb vagotomy Anterior wall of duodenal bulb Simple closure Simple closure with a Graham patch Penetrated ulcer can cause such using omentum complications: 1). Abdominal abscess; Stomach resection 2). Portal pyelophlebitis; 3). Stomach- organ fistula; 4). Acute pancreatitis; 5). Antrumectomy Bleeding. 1, 2, 3; It has been abandoned as a method to treat ulcer disease 2, 3, 5; 1, 3, 5; A 42-year-old executive has refractory 3, 4, 5; chronic duodenal ulcer disease. -

Phytobezoar: Not an Uncommon Cause of Intestinal Obstruction
ISRA MEDICAL JOURNAL Volume 3 Issue 3 Dec 2011 CASE REPORT PHYTOBEZOAR: NOT AN UNCOMMON CAUSE OF INTESTINAL OBSTRUCTION Ishtiaq Ahmed, Samia Shaheen, Sundas Ishtiaq ABSTRACT We are presenting a case report of an 18 year old boy brought in emergency with acute intestinal obstruction. An exploratory Laparotomy revealed Guava pulp and seeds making a large phytobezoars as a cause of the acute small intestinal obstruction at mid ileum. Enterotomy was done to remove the bezoars and patient had smooth recovery. KEY WORDS: Phytobezoar, Intestinal obstruction, Diagnosis, Management INTRODUCTION have been reported5, 7 . Due to change in dietary habits and improvement in medical facilities, bezoars are Bezoars were sought because they were believed to now diagnosed more commonly as a cause on have the power of a universal antidote against any intestinal obstruction in our set up. poison. It was believed that a drinking glass which contained a bezoar would neutralize any poison CASE REPORT poured into it. The word "bezoar" comes from the Persian pâdzahr (ÑÜÜå ÒÏÇ ), which literally means An 18 year old boy was admitted with five days history "antidote"1 . It has been the subject of fascination in of abdominal distension, generalized abdominal pain medical history because of the belief that it and vomiting. Past medical history was inconclusive. possesses magical power. In 1575, the surgeon Clinical examination revealed marked central Ambroise Paré believed that the bezoar didn't have abdominal distension, tenderness with localized antidote properties. It happened that a cook at Paré's guarding and absent bowel sounds. Plain abdominal court was caught stealing fine silver cutlery. -

Foreign Body Imaging-Experience with 6 Cases of Retained Foreign Bodies in the Emergency
Arch Clin Med Case Rep 2020; 4 (5): 952-968 DOI: 10.26502/acmcr.96550285 Case Series Foreign Body Imaging-Experience with 6 Cases of Retained Foreign Bodies in the Emergency Radiology Unit Muniraju Maralakunte MD1, Uma Debi MD1*, Lokesh Singh MD1, Himanshu Pruthi MD1, Vikas Bhatia MD, DNB DM1, Gita Devi MD1, Sandhu MS MD1 2Department of Radio diagnosis, PGIMER, Chandigarh, India *Corresponding Author: Dr. Uma Debi, Radiodiagnosis and Imaging, PGIMER, Chandigarh, India, Tel: 0091- 172-2756381; Fax: 0091-172-2745768; E-mail: [email protected] Received: 22 June 2020; Accepted: 14 August 2020; Published: 21 September 2020 Abstract Introduction: Retained foreign bodies are the external objects lying within the body, which are placed with voluntary or involuntary intentions. The involuntarily or accidentally, and complicated cases with the retained foreign body may come to the emergency services, which may require rapid and adequate imaging assessment. Materials and methods: We share our experience with six different cases with retained foreign bodies, who visited emergency radiological services with acute presentation of symptoms. The choice of radiological investigation considered based on the clinical presentation of the subjects with a retained foreign body. Conclusion: Patients with the retained foreign body may present acute symptoms to the emergency medical or surgical services, radiologists play a central role in rapid imaging evaluation. Radiological investigation plays a crucial role in identification, localization, characterization, and reporting the complication of the retained foreign bodies, and in many scenarios, radiological investigations may expose the unsuspected or concealed foreign bodies in the human body. Ultimately radiological services are useful rapid assessment tools that aid in triage and guide in the medical or surgical management of patients with a retained foreign body. -

Perforated Duodenal Ulcer an Alternative Therapeutic Plan
SPECIAL ARTICLE Perforated Duodenal Ulcer An Alternative Therapeutic Plan Arthur J. Donovan, MD; Thomas V. Berne, MD; John A. Donovan, MD n alternative plan for the treatment of a perforated duodenal ulcer is proposed. We will focus on the now-recognized role of Helicobacter pylori in the genesis of the ma- jority of duodenal ulcers and on the high rate of success of therapy with a combina- tion of antibiotics and a proton-pump inhibitor or histamine2 blocker in treatment of suchA ulcers. Knowledge that half the cases of perforated duodenal ulcer may have securely sealed spontaneously at the time of presentation is incorporated in the therapeutic plan. Patients with a perforated duodenal ulcer who have already been evaluated for H pylori and are not infected or, if infected, have received appropriate therapy should undergo an ulcer-definitive operation if they are suitable surgical candidates. Most authorities recommend surgical closure of the perforation and a parietal cell vagotomy. The remaining patients should have a gastroduodenogram with water- soluble contrast medium. If the perforation is sealed, the patient can be treated nonsurgically. If the perforation is leaking, secure surgical closure of the perforation is necessary. Following recov- ery from the immediate consequences of the perforation, evaluation for H pylori should be con- ducted. If the patient is infected, combined medical therapy is recommended. If the patient is not infected, Zollinger-Ellison syndrome should be ruled out and medical therapy is recommended if the ulcer has not been treated previously. Elective ulcer-definitive surgery should be considered for the occasional uninfected patient who has already received appropriate medical therapy for the ulcer. -

MANAGEMENT of ACUTE ABDOMINAL PAIN Patrick Mcgonagill, MD, FACS 4/7/21 DISCLOSURES
MANAGEMENT OF ACUTE ABDOMINAL PAIN Patrick McGonagill, MD, FACS 4/7/21 DISCLOSURES • I have no pertinent conflicts of interest to disclose OBJECTIVES • Define the pathophysiology of abdominal pain • Identify specific patterns of abdominal pain on history and physical examination that suggest common surgical problems • Explore indications for imaging and escalation of care ACKNOWLEDGEMENTS (1) HISTORICAL VIGNETTE (2) • “The general rule can be laid down that the majority of severe abdominal pains that ensue in patients who have been previously fairly well, and that last as long as six hours, are caused by conditions of surgical import.” ~Cope’s Early Diagnosis of the Acute Abdomen, 21st ed. BASIC PRINCIPLES OF THE DIAGNOSIS AND SURGICAL MANAGEMENT OF ABDOMINAL PAIN • Listen to your (and the patient’s) gut. A well honed “Spidey Sense” will get you far. • Management of intraabdominal surgical problems are time sensitive • Narcotics will not mask peritonitis • Urgent need for surgery often will depend on vitals and hemodynamics • If in doubt, reach out to your friendly neighborhood surgeon. Septic Pain Sepsis Death Shock PATHOPHYSIOLOGY OF ABDOMINAL PAIN VISCERAL PAIN • Severe distension or strong contraction of intraabdominal structure • Poorly localized • Typically occurs in the midline of the abdomen • Seems to follow an embryological pattern • Foregut – epigastrium • Midgut – periumbilical • Hindgut – suprapubic/pelvic/lower back PARIETAL/SOMATIC PAIN • Caused by direct stimulation/irritation of parietal peritoneum • Leads to localized -

Abdominal X-Rays Made Easy
Abdominal X-Rays Made Easy James D. Begg '" BS FROR ConsuIUnlR.Jdiologist, � V"1Ctl.lrY HospiLlL """"" ;u.t Honor.ryin StniorLmUIll'l" """"'"' "'1oIogy. UnilwsilY 01 Duodl't', �nd,UK CHURCHill LIVINGSTONE WNIllIRCH IOOOON NEWYORK PHlLADEU'HIAl.ot.ffi ST SYDf\.'EY TOROI'lTO1999 Contents 1. How 10 lookat an abdominal X-ray 2. Solid organs 35 3. Hollow organs 55 4. Abnonnal gas 86 5. Ascitl'S 116 6. Abnormal intra-abdominal calcification 118 7. The female abdomen 154 !. Abdominal trauma 157 9. iatrogl'nk objects 164 10. Rlreign bodies, artefacts. misleading images 170 11. TheiK'Ute abdOml'fl In 12. Hints 179 Index 183 Cater 1 How to look at an abdominal X-ray Approachto the film • The initial inspection of any X-ray begins with a technical ilSSC'Ssmenl. Establishment of the n.lme,date, dale of birth, age and sex of the patient althe outsetis cruciJl. There are no prizes for making a brilliant diagnosis in Inc wrong patil'flll Further information relating to the ward number or hospital of originmay give an idea as tothe potential nature of the patient's problem, {"g. gastrointestinal or urinary, all of which infonnation may be visible on Ihe name badge, so never f.,illo look at it critically. This can be very helpful in exams.You will notice, however, that the data on the patients'name badges in this book have had to be removed to preserve their anonymity. • EslJblish Ihe projection of the film, Virtually every abdominal X-ray is an AP film, i.e.lhe beam P.1Sst.'S from front to back with the film behind the p,ltient, whois lying down with the X-ray machine overhead, but these are fn.'quently acrompanied by erect or even dl'Cubitus views (also APs).