Foreign Body Ingestion: Dos and Don'ts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Animal Behaviour, Animal Welfare and the Scientific Study of Affect
WellBeing International WBI Studies Repository 5-2009 Animal Behaviour, Animal Welfare and the Scientific Study of Affect David Fraser University of British Columbia Follow this and additional works at: https://www.wellbeingintlstudiesrepository.org/emotio Part of the Animal Studies Commons, Comparative Psychology Commons, and the Other Animal Sciences Commons Recommended Citation Fraser, D. (2009). Animal behaviour, animal welfare and the scientific study of affect. Applied Animal Behaviour Science, 118(3), 108-117. This material is brought to you for free and open access by WellBeing International. It has been accepted for inclusion by an authorized administrator of the WBI Studies Repository. For more information, please contact [email protected]. Animal Behaviour, Animal Welfare and the Scientific Study of Affect David Fraser University of British Columbia KEYWORDS animal behaviour, animal welfare, affect, emotion, qualitative research ABSTRACT Many questions about animal welfare involve the affective states of animals (pain, fear, distress) and people look to science to clarify these issues as a basis for practices, policies and standards. However, the science of the mid twentieth century tended to be silent on matters of animal affect for both philosophical and methodological reasons. Philosophically, under the influence of Positivism many scientists considered that the affective states of animals fall outside the scope of science. Certain methodological features of the research also favoured explanations that did not involve affect. The features included the tendency to rely on abstract, quantitative measures rather than description, to use controlled experiments more than naturalistic observation, and to focus on measures of central tendency (means, medians) rather than individual differences. -

Rectal Foreign Body: a Primer for Emergency Physicians Bobby Desai
Desai International Journal of Emergency Medicine 2011, 4:73 http://www.intjem.com/content/4/1/73 CASEREPORT Open Access Visual diagnosis: Rectal foreign body: A primer for emergency physicians Bobby Desai Abstract We present a case that is occasionally seen within emergency departments, namely a rectal foreign body. After presentation of the case, a discussion concerning this entity is given, with practical information on necessity of an accurate and thorough history and removal of the object for clinicians. Case anoscope inserted. The object could not be visualized, A 39-year-old male presented to the Emergency Depart- and therefore no attempt was made to remove it. Gen- ment with vague complaints of abdominal pain and con- eral surgery was consulted to see the patient and stipation. He stated that the abdominal pain was dull decided to take him to the operating room for removal. and crampy in nature and generalized in distribution. The patient agreed to this. Furthermore, he stated that he had not had a bowel The object was noted to be the extension arm of a movement in 2 days, though he felt as if he had to have vacuum cleaner. It was removed according to notes with one. He denied constitutional complaints of fevers, some difficulty and the patient was admitted to the hos- chills, nausea, and vomiting, and denied urinary com- pital for observation and intravenous antibiotics. The plaints as well. patient was subsequently discharged 2 days later in The patient’s vital signs were: temperature 37.2°C, excellent condition. Upon social work discharge, he was pulse 87 beats per minute, respiratory rate of 20 per again asked how that apparatus managed to be placed minute, and blood pressure 130/84 mmHg. -

Functional Aspects of Emotions in Fish
Behavioural Processes 100 (2013) 153–159 Contents lists available at ScienceDirect Behavioural Processes jou rnal homepage: www.elsevier.com/locate/behavproc Functional aspects of emotions in fish ∗ Silje Kittilsen Norwegian School of Veterinary Science, Norway a r t i c l e i n f o a b s t r a c t Article history: There is an ongoing scientific discussion on whether fish have emotions, and if so how they experience Received 19 March 2013 them? The discussion has incorporated important areas such as brain anatomy and function, physiological Received in revised form and behavioural responses, and the cognitive abilities that fish possess. Little attention has however, been 10 September 2013 directed towards what functional aspects emotions ought to have in fish. If fish have emotions – why? Accepted 11 September 2013 The elucidation of this question and an assessment of the scientific evidences of emotions in fish in an evolutionary and functional framework would represent a valuable contribution in the discussion on Keywords: whether fish are emotional creatures. Here parts of the vast amount of literature from both biology and Emotions Behaviour psychology relating to the scientific field of emotions, animal emotion, and the functional aspects that Cognition emotions fulfil in the lives of humans and animals are reviewed. Subsequently, by viewing fish behaviour, Psychology physiology and cognitive abilities in the light of this functional framework it is possible to infer what Fish functions emotions may serve in fish. This approach may contribute to the vital running discussion on Evolution the subject of emotions in fish. In fact, if it can be substantiated that emotions are likely to serve a function in fish similar to that of other higher vertebrate species, the notion that fish do have emotions will be strengthened. -

AVMA Guidelines for the Euthanasia of Animals: 2020 Edition*
AVMA Guidelines for the Euthanasia of Animals: 2020 Edition* Members of the Panel on Euthanasia Steven Leary, DVM, DACLAM (Chair); Fidelis Pharmaceuticals, High Ridge, Missouri Wendy Underwood, DVM (Vice Chair); Indianapolis, Indiana Raymond Anthony, PhD (Ethicist); University of Alaska Anchorage, Anchorage, Alaska Samuel Cartner, DVM, MPH, PhD, DACLAM (Lead, Laboratory Animals Working Group); University of Alabama at Birmingham, Birmingham, Alabama Temple Grandin, PhD (Lead, Physical Methods Working Group); Colorado State University, Fort Collins, Colorado Cheryl Greenacre, DVM, DABVP (Lead, Avian Working Group); University of Tennessee, Knoxville, Tennessee Sharon Gwaltney-Brant, DVM, PhD, DABVT, DABT (Lead, Noninhaled Agents Working Group); Veterinary Information Network, Mahomet, Illinois Mary Ann McCrackin, DVM, PhD, DACVS, DACLAM (Lead, Companion Animals Working Group); University of Georgia, Athens, Georgia Robert Meyer, DVM, DACVAA (Lead, Inhaled Agents Working Group); Mississippi State University, Mississippi State, Mississippi David Miller, DVM, PhD, DACZM, DACAW (Lead, Reptiles, Zoo and Wildlife Working Group); Loveland, Colorado Jan Shearer, DVM, MS, DACAW (Lead, Animals Farmed for Food and Fiber Working Group); Iowa State University, Ames, Iowa Tracy Turner, DVM, MS, DACVS, DACVSMR (Lead, Equine Working Group); Turner Equine Sports Medicine and Surgery, Stillwater, Minnesota Roy Yanong, VMD (Lead, Aquatics Working Group); University of Florida, Ruskin, Florida AVMA Staff Consultants Cia L. Johnson, DVM, MS, MSc; Director, -

Perforation Due to a Rectal Foreign Body and Radiological Findings
Case Report Ann Colorectal Res 2021;9(1):44-46. Perforation Due to a Rectal Foreign Body and Radiological Findings Saim Turkoglu1, MD; Adem Yokuş2, MD; Fırat Aslan3, MD 1Van Traınıng and Research Hospıtal, Van, Turkey 2Department of Radiology, Medical Faculty, Yuzuncu Yıl University, Van, Turkey 3Department of General Surgery, Medical Faculty, Yuzuncu Yıl University, Van, Turkey *Corresponding authors: Received: 01-03-2021 Saim Turkoglu, Van Traınıng and Research Hospıtal, Van,Turkey Revised: 03-04-2021 Tel: +90 5356452865; Fax: +90 432 2150471 Accepted: 05-04-2021 Email: [email protected] Abstract Introduction: Rectal foreign bodies have been increasingly seen and cause urgent surgical complications. Diagnosis and treatment of these cases in emergency departments may be difficult. The effective use of radiological imaging techniques can accelerate and facilitate this process. Case Presentation: A 65-year-old male patient, who underwent computed tomography (CT) with the suspicion of a foreign body in the rectum, was admitted to the emergency outpatient clinic. The patient was a male with a psychiatric illness who later underwent emergency surgery. Since the patient had impaired consciousness during the examination, anamnesis could not be obtained, so the initial impression upon surgical consultation was perforation due to rectal tumoral thickening. In almost all cases, plain radiography is sufficient and can eliminate diagnostic difficulties. However, this is not possible for non-opaque objects. Therefore, the CT scan played an important role in the diagnosis of this patient. A 30 cm foreign body, identified as salami, was removed from the abdomen of the patient, who was later taken for emergency surgery. -

THE ACUTE ABDOMEN Definition Abdominal Pain of Short Duration
THE ACUTE ABDOMEN Definition Abdominal pain of short duration that is usually associated with muscular rigidity, distension and vomiting, and which requires a decision whether an emergent operation is required. Problems and management options History and physical examination are central in the evaluation of the acute abdomen. However, in an ICU patient, these are often limited by sedation, paralysis and mechanical ventilation, and obscured by a protracted, complicated inhospital course. Often an acute abdomen is inferred from unexplained sepsis, hypovolaemia and abdominal distension. The need for prompt diagnosis and early treatment by no means equates with operative management. While it is a truism that correct diagnosis is the essential preliminary to correct treatment, this is probably more so in nonoperative management. On occasions, the need for operation is more obvious than the diagnosis and no delay should be incurred in an attempt to confirm the diagnosis before surgery. Frequently fluid resuscitation and antibiotics are required concurrently with the evaluation process. The approach is to evaluate the ICU patient in the context of the underlying disorder and decide on one of the following options: ∙ Immediate operation (surgery now)– the ‘bleeder’ e.g. ruptured ectopic pregnancy, ruptured abdominal aortic aneurysm (AAA) in the salvageable patient ∙ Emergent operation (surgery tonight)– the ‘septic’ e.g. generalized peritonitis from perforated viscus ∙ Early operation (surgery tomorrow)– the ‘obstructed’, e.g. obstructed colonic cancer ∙ Radiologically guided drainage – e.g. localized abscesses, acalculous cholecystitis, pyonephrosis ∙ Active observation and frequent reevaluation – e.g localized peritoneal signs other than in the RLQ, selected cases of endoscopic perforation . -
Managing Envenomations
ResidentOfficial Publication of the Emergency Medicine Residents’ Association June/July 2021 VOL 48 / ISSUE 3 Managing Envenomations How to Sustain a Career: Peer Support Guide to ABEM Certi ication We Help Healers SCP Reach New Heights Health Meet Your Medical Career Dream Team SCP Health Step Right Up, Residents! As you’re transitioning from residency to begin your career, our team is here to create a tailored environment for you that fosters growth and delivers rewarding daily work experiences. Explore clinical careers at scp-health.com/explore TOGETHER, WE HEAL Welcome to a New Academic Year! uly marks a turning point each year, as new interns arrive in programs throughout Jthe country, newly graduated residents launch the next phase of their careers, and medical students take the next steps in their journey to residency. DO YOU KNOW HOW EMRA CAN HELP? Resources for Interns Resources for PGY2+ Resources for Students All EM programs will receive EMRA residents members receive the EMRA shows up for medical students Intern Kits this summer with nearly 10-pound EMRA Resident Kit upon interested in this specialty. From resources that offer immediate first joining EMRA. It is packed with clinical new advising content every month to backup for those first nerve-wracking resources for every rotation — some you’ll opportunities for leadership and growth, shifts. The high-yield EMRA Intern need only rarely (but prove to be clutch), and EMRA student membership is high-yield. Kit is sent for free to all EM interns some you’ll use every single shift (EMRA Plus, our online resources are unparalleled: (membership not required) and Antibiotic Guide, anyone?). -

Surgical Management of Anorectal Foreign Bodies H Cinar, M Berkesoglu1, M Derebey2, E Karadeniz3, C Yildirim4, K Karabulut2, T Kesicioglu5, K Erzurumlu2
[Downloaded free from http://www.njcponline.com on Monday, June 11, 2018, IP: 102.251.47.77] Original Article Surgical Management of Anorectal Foreign Bodies H Cinar, M Berkesoglu1, M Derebey2, E Karadeniz3, C Yildirim4, K Karabulut2, T Kesicioglu5, K Erzurumlu2 Department of General Purpose: Anorectal foreign bodies (AFBs) inserted into anus constitute one of Surgery, Faculty of Medicine, the most important problems needing surgical emergency due to its complications. Ordu University, Ordu, 1Department of General We describe our experience in the diagnosis and treatment of AFBs retained Surgery, Mersin University, in the rectosigmoid colon. Materials and Methods: Between the years 2006 Abstract Mersin, 2Department of and 2015, a total of 11 patients diagnosed with AFBs were admitted to an General Surgery, Ondokuz emergency room and general surgery clinics. They were diagnosed and treated Mayıs University, Samsun, in four different hospitals in four different cities in Turkey. Information on the 3Department of General AFBs, clinical presentation, treatment strategies, and outcomes were documented. Surgery, Atatürk University, Erzurum, 4Department of We retrospectively reviewed the medical records of these unusual patients. General Surgery, Ordu Public Results: Eleven patients were involved in this study. All patients were male with Hospital, Ordu, 5Department their mean age was 49.81 (range, 23–71) years. The time of the presentation to of General Surgery, Faculty the removal of the foreign bodies ranged between 2 h and 96 h with a mean of of Medicine, Giresun 19.72 h. Ten patients inserted AFBs in the anus with the purpose of eroticism but University, Giresun, Turkey one patient’s reason to relieve constipation. -

Historical Note
East African Orthopaedic Journal HISTORICAL NOTE AMBROISE PARE 1510-1590 Pare was born in 1510 in Bourge-Hersent in North- were failing to emerge from the gums due to lack of West France. He initially worked with his brother who a pathway, and this failure was a cause of death. This was a surgeon cum barber. He practiced at Hotel Dieu, belief and practice persisted for centuries, with some Frances oldest Hospital. He was an anatomist and exceptions, until towards the end of the nineteenth invented several surgical instruments. He became a century lancing became increasingly controversial and war injury doctor at Piedmont where he used boiled oil was then abandoned (2). for treating gunshot wounds. One day he improvised In 1567, Ambroise Pare described an experiment using oil of roses, egg white and turpentine with very to test the properties of bezor stones. At the time, the good results. Henceforth he stopped the cauterization stones were commonly believed to be able to cure and hot oil method. the effects of any poison, but Pare believed this to be Pare was a keen observer and did not allow the impossible. It happened that a cook at Pare court was beliefs of the day to supersede the evidence at hand. In caught stealing fine silver cutlery, and was condemned his autobiographical book, Journeys in Diverse Places, to be hanged. The cook agreed to be poisoned, on the Pare inadvatienty practiced the scientific method when conditions that he would be given a bezoar straight he returned the following morning to a battlefield. -
Foreign Body Insertions: a Review
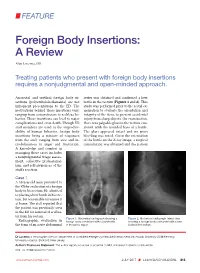
FEATURE Foreign Body Insertions: A Review Alan Lucerna, DO Treating patients who present with foreign body insertions requires a nonjudgmental and open-minded approach. Anorectal and urethral foreign body in- series was obtained and confirmed a beer sertions (polyembolokoilamania) are not bottle in the rectum (Figures 1 and 2). This infrequent presentations to the ED. The study was performed prior to the rectal ex- motivations behind these insertions vary, amination to evaluate the orientation and ranging from autoeroticism to reckless be- integrity of the item, to prevent accidental havior. These insertions can lead to major injury from sharp objects. On examination, complications and even death. Though ED there was palpable glass in the rectum con- staff members are used to the unpredict- sistent with the rounded base of a bottle. ability of human behavior, foreign body The glass appeared intact and no gross insertions bring a mixture of responses bleeding was noted. Given the orientation from the staff, ranging from awe and in- of the bottle on the X-ray image, a surgical credulousness to anger and frustration. consultation was obtained and the patient A knowledge and comfort in managing these cases includes a nonjudgmental triage assess- ment, collective professional- ism, and self-awareness of the staff’s reaction. Case 1 A 58-year-old man presented to the ED for evaluation of a foreign body in his rectum. He admitted to placing a beer bottle in his rec- tum, but was unable to remove it at home. The staff reported that the patient was previously seen in the ED for removal of a vibra- tor from his rectum. -

Foreign Rectal Body – Systematic Review and Meta-Analysis
REVIEW 61 Foreign rectal body – Systematic review and meta-analysis M. Ploner1, A. Gardetto2, F. Ploner3, M. Scharl4, S. Shoap5, H. C. Bäcker5 (1) Department of Anesthesiology and Intensiver Care, Cantonal Spital Lucerne, Lucerne, Switzerland ; (2) Department of Plastic Surgery, Hospital Sterzing, Sterzing, South Tirol, Italy ; (3) Department of Anesthesiology and Emergency Medicine, Hospital Sterzing, South Tirol, Italy ; (4) Department of Gastroenterology and Hepatology, University Hospital Zurich, University of Zurich, Swetzerland ; (5) Department of Orthopaedic Surgery, Columbia University Medical Center, New York, USA. Abstract instrumentation (7). The most common complication is a rectal injury, which can result from a variety of agents and Background : Self-inserted foreign rectal bodies are an objects (8). Often, nonsurgical removal of foreign bodies infrequent occurrence, however they present a serious dilemma to the surgeon, due to the variety of objects, and the difficulty of has been described to be successful – in 11% to 65% – extraction. The purpose of this study is to give a comprehensive (9), however, in many situations, a surgical treatment review of the literature regarding the epidemiology, diagnostic may be essential. There have been a variety of algorithms tools and therapeutic approaches of foreign rectal body insertion. Methods : A comprehensive systematic literature review on introduced for the management of extraction, however, Pubmed/ Medline and Google for ‘foreign bodies’ was performed because of the diversity of foreign bodies, improvisation, on January 14th 2018. A meta-analysis was carried out to evaluate as well creativity of the treating emergency physician the epidemiology, diagnostics and therapeutic techniques. 1,551 abstracts were identified, of which 54 articles were included. -

Book of Abstracts
Dr. John Miller (University of Sheffield) Animals, Capital, Literature and the Victorians: Writing the Fur Trade The difference between what we think of as ‘animal’ and what we think of as ‘human’ is routinely conceptualised as a fullness on the side of the human against a poverty on the side of the animal. In response, animal studies, in its emergence over the last twenty years or so, has set about dismantling this crude logic and broadening the scope of humanities research to include the nonhuman. Although at this juncture of the twenty first century, animal studies has the status of an emerging field of study, many of its central concerns are significant ingredients of nineteenth-century thought. Evolutionary theory radically destabilised entrenched ideas of human–animal difference; animal advocacy flowered, through the work of the RSPCA, the vegetarian society and the humanitarian League amongst others; the connections of discourses of species to discourses of race, class and gender became increasingly clear, and increasingly subject to debate, as the century progressed. At the same time, the use of animal bodies in a developing commodity culture accelerated to a remarkable degree, marking the Victorian period, in particular, as an era of extraordinary violence. This paper explores one of the most disturbing examples of this objectification of animal life: the global fur trade. I am interested especially in the ways in which literary fiction both bolstered and contested the conceptions of value behind the fur trade’s commodifying processes. How, I ask, do literature and capital entwine in the imagining of animals as resources to be consumed? Simone Rebora (Università di Verona) “It’s as semper as oxhousehumper!” James Joyce’s animalisation of the human Few animals can be met through the works of James Joyce.