Wakefield Transformation Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WAKEFIELD SOUTH and RURAL - City Centre, Alverthorpe, Thornes, Agbrigg, Sandal, Crigglestone, Hall Green and Kettlethorpe
Local Support and Social Groups to aid independence and healthy living WAKEFIELD SOUTH AND RURAL - City Centre, Alverthorpe, Thornes, Agbrigg, Sandal, Crigglestone, Hall Green and Kettlethorpe This information has been compiled by the Live Well Wakefield Service South West Yorkshire Partnership NHS Foundation Trust. We aim to provide accurate and useful information and every effort has been made to ensure this information is correct. This directory was updated on the date shown below. If that date is not within the last 6 months there will be a more up to date version available. Please note: This directory is not exhaustive and inclusion is not an endorsement. No responsibility can be taken for advice or services provided by any support service or social group listed. If you notice any errors or would like more information, please telephone our office on 01924 255363. Live Well Wakefield, the Agbrigg and Belle Vue Community Centre, Montague Street, Agbrigg, Wakefield WF1 5BB Updated October 2019 Areas covered in this Directory Page Wakefield City Centre, Alverthorpe and Thornes 3 - 19 Agbrigg and Sandal 20 - 31 Crigglestone, Hall Green and Kettlethorpe 32 - 38 Each area contains the following headings: Hobbies and Social Groups Lunch Clubs Physical Activity Support Groups Other Useful Contact s Other Directories cover the following areas: PONTEFRACT, Carleton, Darrington, East Hardwick, Knottingley and Ferrybridge CASTLEFORD and Airedale SOUTH EAST – Ackworth, South Elmsall, South Kirkby, Upton, Hemsworth, Ryhill, and Havercroft NORMANTON, -

Wakefield College
CASE STUDY: WAKEFIELD COLLEGE Wakefield College gives Brand-Rex top marks Based nine miles southeast of Leeds and 28 miles southwest of York on the eastern edge of the UK’s Pennines district, Wakefield College first opened its doors in 1868. After experiencing gradual expansion, it is now West Yorkshire’s largest college and is currently home to 700 staff and over 10,000 students of all ages and abilities, studying a broad range of academic and vocational courses. CASE STUDY: WAKEFIELD COLLEGE “We recognised the need to install a top quality cabling system and after assessing what was available with our chosen installation partner, Connect IP, it was clear that Brand-Rex could meet our requirements.” Wakefield College has gained an enviable reputation for the quality of Brand-Rex has continually set the standard within its own industry and the education it offers. A level pass rates have been above 95 per cent beyond and, as well as boasting carbon neutrality to ISO 14064 and and it currently has an established higher education provision, which is PAS 2060 certifications, it recently won the Vision In Business for the branded as the University Centre Wakefield. What’s more, a recent Ofsted Environment in Scotland (VIBES) Award in the Energy Management report praised its approach to working with the local community and its and Efficiency category. commitment to equality and diversity. ‘Getting to a point where we can describe Cat6Plus as carbon neutral was a Students attend one of three campuses, all located in the Wakefield complex but highly worthwhile exercise,’ says Kennedy Miller, technology and district. -

Wakefield College Wakefield College
Wakefield College Wakefield City Campus General Telephone: Margaret Street 01924 789789 Wakefield WF1 2DH [email protected] Castleford Campus Course Information: Thunderhead Ridge 01924 789111 Castleford WF10 4UA [email protected] www.wakefield.ac.uk All our guides and prospectuses are available in PDF format on our website. Alternative formats are available on request - telephone 01924 789585 for details. School Leaver Prospectus 2020/21 A Levels, Apprenticeships, Vocational & Foundation Learning Courses Contents Find out... A Levels Ofsted - we are a Good provder ������������������������������������������������������������� 04 Art, Design & Media ����������������������������������������������������������������������������������������������������82 How to apply ������������������������������������������������������������������������������������������������������������������������06 Media Studies �����������������������������������������������������������������������������������������������������������������83 WF9 Bus ��������������������������������������������������������������������������������������������������������������������������������������07 Photography����������������������������������������������������������������������������������������������������������������������83 Routes to success ������������������������������������������������������������������������������������������������������� 08 Business & Management ������������������������������������������������������������������������������������83 Which level -

Bruntcliffe 2017 Leaver Destinations
Bruntcliffe 2017 Leaver Destinations This is the third year that C&K Careers has tracked and monitored destinations for the Year 11 leavers from Bruntcliffe Academy. After GCSE results day the careers adviser in school has been contacting the Year 11 leavers, parents, colleges and training providers to confirm their plans and destinations now that they have left school. The careers department has also provided extra support over the summer holidays to discuss alternative courses or colleges if students’ GCSE grades were not what they needed. Out of 174 students: 169 – (97.1%) are meeting the duty to participate in learning 5 – (2.8%) are not meeting the duty to participate and these include: 1 (0.57%) who is not in education, employment and training (NEET) 1 (0.57%) who is taking a temporary break from learning (teenage parent) 3 (1.72%) in employment without training, no accredited learning or part time or temporary work Pupil Premium 66 students out of 174 cohort are Pupil Premium with 64 (96.9%) students meeting the duty to participate in learning. 2 (3.0%) Pupil Premium students are not meeting the duty. 1 of the 2 (1.5%) is NEET. Further analysis is provided below; In Learning Apprenticeships – 5.7% Apprenticeships are one of the areas the careers team in school promote and inform students about. A wide range of occupations are available and the new Higher Apprenticeships are also generating interest. This year Careers built on the existing apprenticeship programme in school by organising mock job interviews delivered by Carillion Construction. This gave students an idea of what a job interview entails and hopefully helped to quell some nerves. -

WAKEFIELD SOUTH and RURAL - City Centre, Alverthorpe, Thornes, Agbrigg, Sandal, Crigglestone, Hall Green and Kettlethorpe
Local Support and Social Groups to aid independence and healthy living WAKEFIELD SOUTH AND RURAL - City Centre, Alverthorpe, Thornes, Agbrigg, Sandal, Crigglestone, Hall Green and Kettlethorpe This information has been compiled by the Live Well Wakefield Service South West Yorkshire Partnership NHS Foundation Trust. We aim to provide accurate and useful information and every effort has been made to ensure this information is correct. This directory was updated on the date shown below. If that date is not within the last 6 months there will be a more up to date version available. Please note: This directory is not exhaustive and inclusion is not an endorsement. No responsibility can be taken for advice or services provided by any support service or social group listed. If you notice any errors or would like more information, please telephone our office on 01924 255363. Live Well Wakefield, the Agbrigg and Belle Vue Community Centre, Montague Street, Agbrigg, Wakefield WF1 5BB Updated September 2018 Areas covered in this Directory Page Wakefield City Centre, Alverthorpe and Thornes 2 - 16 Agbrigg and Sandal 17 - 28 Crigglestone, Hall Green and Kettlethorpe 29 - 37 Each area contains the following headings: Hobbies and Social Groups Lunch Clubs Physical Activity Support Groups Other Useful Contact s Other Directories cover the following areas: PONTEFRACT, Carleton, Darrington, East Hardwick, Knottingley and Ferrybridge CASTLEFORD and Airedale SOUTH EAST – Ackworth, South Elmsall, South Kirkby, Upton, Hemsworth, Ryhill, and Havercroft -

Annual Accounts 2017/18
Report & Financial Statements 2017/18 WAKEFIELD COLLEGE REPORT AND FINANCIAL STATEMENTS FOR THE YEAR ENDED 31 JULY 2018 Key Management Personnel, Board of Governors and Professional Advisers Key management personnel Key management personnel are represented by the following in 2017/18: Post Title Post Holder Date Date of Appointed Resignation Principal, Chief Executive and Sam Wright 01/03/2011 N/A Accounting Officer Executive Director: Finance and Jason Pepper 12/06/2017 N/A Resources Executive Director: Quality and Sue Slassor 01/09/1991 N/A Planning Executive Director: Curriculum Lisa 01/02/2012 N/A Macdonald Executive Director: Student Clare Allcock 14/05/2012 N/A Experience and Student Support Executive Director: Human Karen Sykes 30/09/2002 N/A Resources and Organisational Development Executive Director: Employer Joanne Taylor 01/01/2017 N/A Engagement and Apprenticeships Assistant Principal: Commercial Ian Wainwright 01/08/2011 31/01/2018 Development and External Relations Director: Higher Education Clare Hagerup 10/09/2014 N/A Director: Higher Education Tony Rex 18/02/2002 N/A Development Director: Estates Jon Howard 04/01/2005 N/A Clerk to Corporation Nils Elgar 07/02/2005 N/A Board of Governors A full list of Governors is given on page 29 of these financial statements. Dr N Elgar acted as Clerk to the Corporation throughout the period. Page 2 Professional Advisers Financial Statements and Bankers: Regularity auditor: Close Brothers Limited Grant Thornton UK LLP 10 Crown Place 2 Broadfield Court London Sheffield EC2A 4FT S8 0XF -
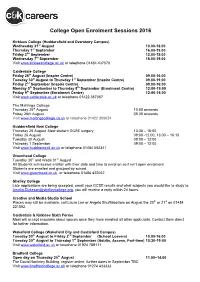
College Open Enrolment Sessions 2016
College Open Enrolment Sessions 2016 Kirklees College (Huddersfield and Dewsbury Campus) Wednesday 31st August 10.00-18.00 Thursday 1st September 16.00-19.00 Friday 2nd September 12.00-15.00 Wednesday 7th September 16.00-19.00 Visit www.kirkleescollege.ac.uk or telephone 01484 437070 Calderdale College Friday 26th August (Inspire Centre) 09.00-16.00 Tuesday 30th August to Thursday 1st September (Inspire Centre) 09.00-19.00 Friday 2nd September (Inspire Centre) 09.00-16:00 Monday 5th September to Thursday 8th September (Enrolment Centre) 12:00-19:00 Friday 9th September (Enrolment Centre) 12:00-16.00 Visit www.calderdale.ac.uk or telephone 01422 357357 The Maltings College Thursday 25th August 10:00 onwards Friday 26th August 08.30 onwards Visit www.maltingscollege.co.uk or telephone 01422 300024 Huddersfield New College Thursday 25 August -New student GCSE surgery 13:30 – 16:00 Friday 26 August 09:00 -12.00, 13:00 – 16:15 Tuesday 30 August 09:00 – 12:00 Thursday 1 September 09:00 – 12:00 Visit www.huddnewcoll.ac.uk or telephone 01484 652341 Greenhead College Tuesday 30th and Weds 31st August All Students will receive a letter with their date and time to enrol on so it isn’t open enrolment Students are enrolled and grouped by school. Visit www.greenhead.ac.uk or telephone 01484 422032 Shelley College Late applications are being accepted, email your GCSE results and what subjects you would like to study to [email protected], you will receive a reply within 24 hours. -

Yorkshire & Humberside Service Report September
Yorkshire & Humberside Service Report September 2019 1 Yorkshire & Humberside Service Report September 2019 Service Availability The SLA target sets a minimum of 99.7% availability for each customer, averaged over a 12 month rolling period Periods of scheduled and emergency maintenance are discounted when calculating availability of services Monthly and annual availabilities falling below 99.7% are highlighted * Service has resilience - where an organisation retains connectivity during an outage period by means of a second connection, the outage is not counted against its availability figures 12 Month Service Oct 18 Nov 18 Dec 18 Jan 19 Feb 19 Mar 19 Apr 19 May 19 Jun 19 Jul 19 Aug 19 Sep 19 Rolling Availability Askham Bryan College, York Campus 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% Barnsley College 100% 100% 99.94% 100% 100% 100% 100% 100% 100% 100% 100% 100% >99.99% Barnsley College, Honeywell Lane 0.00% 0.00% 0.00% 100% 100% 100% 100% 100% 100% 100% 100% 100% <12 Months Barnsley Metropolitan Borough Council, Personal & 100% 100% 99.94% 100% 100% 100% 100% 100% 100% 100% 100% 100% >99.99% Community Development Bishop Burton College, Bishop Burton 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% Bradford College 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% Bradford College, The David Hockney Building 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% Calderdale College 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% Calderdale Metropolitan Borough -

MEADOWCROFT SCHOOL Welcome to Meadowcroft
MEADOWCROFT SCHOOL Welcome to Meadowcroft When you come through the doors at one of our three sites, When they leave Meadowcroft, we want every child to have you quickly realise that this is no ordinary school. We have a truly secured the skills and confidence they need to find sustainable amazing team who pride themselves on their relentless employment; developed interests and hobbies to keep them determination to help every child, no matter what their situation motivated; and learnt how to make and sustain healthy or circumstances, to achieve their potential. relationships. With these key skills, we know our children can be healthy, happy, successful adults. Our school is based on four sites, The Gallery, The Hub, The Works and The Allotment each providing very focused care for A highlight of my time as Headteacher here was seeing eight of the children we support. All our children have complex social, our students achieve their Gold Duke of Edinburgh Award. It was emotional and mental health needs and many have additional incredible to watch the young people grow in self-confidence as severe learning and communication difficulties. Most of the they persevered to complete the programme. They are a shining children we care for have struggled to engage in formal example of what can be achieved with the right care, support, education, so our job involves far more than simply providing an encouragement and determination. engaging and creative setting for them to learn in. We come I hope this brochure will give you an overview of the care and alongside our children, take an interest in their lives and help educational support offered by Meadowcroft. -

Aoc Sport Yorkshire & Humber National Championship Team 2019
AoC Sport Yorkshire & Humber National Championship Team 2019 Badminton Women’s Badminton Men’s Pos College Pos College 1 John Leggott College 1 New College Pontefract 2 Wyke Sixth Form College 2 Thomas Rotherham College 3 Greenhead College 3 New College Pontefract Women’s Basketball Men’s Basketball Pos College Pos College 1 Greenhead College 1 Greenhead College Cricket – Indoor24 Pos College 1 Huddersfield New College Cross Country – Women’s Regional Cross Country – Men’s Regional Pos College Pos College 1 Greenhead College 1 New College Pontefract 2 New College Pontefract 2 Greenhead College 3 Greenhead College 3 John Leggott College 4 John Leggott College 4 Huddersfield New College 5 John Leggott College 5 Thomas Rotherham College 6 New College Pontefract 6 Leeds City College 7 Barnsley College 7 Greenhead College 8 Barnsley College 8 Scarborough 6th Form College AoC Sport Yorkshire & Humber National Championship Team 2019 Women’s 7-a-side football Men’s 7-a-side football Pos College Pos College 1 York College 1 Barnsley College Football for Students with a disability Pos College 1 Shipley College Women’s Golf Men’s Golf Pos College Pos College 1 1 Greenhead College 2 2 North Lindsey College 3 3 Huddersfield New College 4 4 Scarborough Sixth Form College Women’s Hockey Men’s Hockey - Regional Pos College Pos College 1 Greenhead College 1 Franklin College 2 2 Franklin College 3 3 Franklin College 4 4 Franklin College 5 5 Greenhead College 6 6 Greenhead College 7 7 Greenhead College 8 8 Greenhead College 9 9 Greenhead College 10 10 New -

Fourteentosixteen 2019/20
fourteentosixteen prospectus 2019/20 14-16 prospectus 2018/19 Welcome School Partnerships Team Contents Contact Dear Colleague, General Telephone: 01924 789789 Working with our partner schools ....................................4 Diploma in Motor Vehicle Studies ..................................25 At Wakefield College, our Course Information: 01924 789111 learners are at the heart of Our School Liaison offer ........................................................4 Certificate in Vehicle Systems Maintenance .............26 Minicom: 01924 789270 all we do and we recognise that everyone has different Technical Awards ...........................................................................5 Extended Certificate in Music Practitioners .............. 27 General Enquiries: [email protected] ambitions and needs. Course Information: [email protected] First Award in Animal Care ..................................................6 Diploma in Performing Arts ............................................. 28 We offer a fantastic choice Website: www.wakefield.ac.uk of courses for 14-16 year Award in Motor Studies ........................................................7 Certificate in Performing Engineering Operations .29 olds and some of the best All Wakefield College prospectuses are available training facilities in the in text format on the College website. James Pennington Sandra Lockett Award in Child Development and Care .........................8 Diploma in Public Services .................................................30 region, -

College Enrolment Guide 2020 Please Look for Your First-Choice College and Follow the Guidance to Enrol. Greenhead College If Yo
College Enrolment Guide 2020 Please look for your first-choice college and follow the guidance to enrol. Greenhead College If you have accepted your conditional offer, you should have received a package of information in the post during the first week of August telling you what to do for pre-enrolment and enrolment. When you receive your GCSE results, you need to log onto Greenhead’s Moodle site (indicated by a ‘m’ in a circle at the top of the homepage website (www.greenhead.ac.uk). You need to click on the results link and enter your grades. You must do this before the deadline on the 31st August. You should have received a username and password for their Moodle site in the pack you received in August. If you do not want to take your place at Greenhead College, you need to send an email to the following address to let them know: [email protected] If you want to make a late application for Greenhead, you need to look for the ‘late application form’ on their website (www.greenhead.ac.uk). If you are doing this, you need to do it on results day as soon as possible as places will get filled very quickly. Any problems, please call them on 01484 422032 Heckmondwike Grammar School All students that have received an offer from HGS must upload details of their exam results using the following link: https://bit.ly/hgsenrol They will then contact you by telephone with one of three outcomes - a confirmed offer of a place, a rejection where grades do not meet the requirements, or an invitation to come into school for a meeting on Friday to discuss their options.