Practical Approach to Microscopic Colitis and Inflammatory Bowel Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Microscopic Colitis: Collagenous Colitis and Lymphocytic Colitis
Microscopic Colitis: Collagenous Colitis and Lymphocytic Colitis National Digestive Diseases Information Clearinghouse What is microscopic colitis? The term bowel refers to any part of the small or large intestine. The large intes- Microscopic colitis is inflammation of the tine includes the colon and the rectum, and bowel that is only visible using a microscope. together they are about 5 feet long. The Microscopic colitis is a type of inflammatory U.S. Department small intestine can be 12 to 20 feet long. bowel disease (IBD), which refers to a group of Health and Colitis means inflammation of the colon. Human Services of conditions that causes inflammation in the Microscopic colitis is inflammation of the bowel due to an excessive build-up of white colon and rectum. NATIONAL blood cells in the bowel lining. Microscopic INSTITUTES OF HEALTH colitis is less severe than other types of IBD because it does not lead to cancer and rarely What are collagenous colitis requires surgery. However, microscopic and lymphocytic colitis? colitis can cause considerable pain and Microscopic colitis has two main forms: discomfort. collagenous colitis and lymphocytic colitis. The symptoms of and treatment for both are identical. Some scientists believe the two forms may be different presentations of the same disease. Slight differences in the way intestinal tissues appear when seen with a microscope set them apart. In both forms, an increase in white blood cells can be seen within the intestinal epithelium—the layer of Stomach Liver cells that lines the intestine. Increased white blood cells are a sign of inflammation. But with collagenous colitis, the layer of collagen Colon (shaded) beneath the epithelium appears thicker than normal. -
Familial Occurrence of Lymphocytic Colitis
BRIEF COMMUNICATION Familial occurrence of lymphocytic colitis Hugh J Freeman MD HJ Freeman. Familial occurrence of lymphocytic colitis. Can J Occurrence familiale de la colite Gastroenterol 2001;15(11):757-760. The familial occurrence lymphocytaire of lymphocytic colitis in a female parent and her two female children is reported. No other genetically based disorder, includ- RÉSUMÉ : On fait ici état de l’occurrence familiale de la colite lym- ing celiac disease, was evident. For both children, the age of phocytaire chez une patiente et ses deux filles. Aucune autre maladie diagnosis was more than two decades younger than the age of d’origine génétique, comme la maladie cæliaque, ne s’est manifestée. recognition of disease in the parent, and some clinical features, Pour les deux enfants, le diagnostic a été posé plus d’une vingtaine d’an- including the requirement for pharmacological agents in both nées avant l’âge qu’avait la mère au moment de son diagnostic et cer- taines caractéristiques cliniques, dont le traitement pharmacologique children, suggested that their disease severity was more signifi- chez les deux enfants, donnent à penser que leur maladie est plus grave cant than that of the involved parent. These characteristics of a que chez le parent atteint. Ces caractéristiques de la maladie familiale familial disease have been previously reported and labelled ont déjà été mentionnées et ont été appelées "anticipation génétique" ‘genetic anticipation’ in some monogenetic forms of neurologi- dans le cas de certaines formes monogénétiques de maladies neu- cal disease, as well as in other types of inflammatory bowel dis- rologiques, de même que dans d’autres types de maladies inflammatoires eases, including Crohn’s disease. -

Colitis and Proctitis
Customer Name, Street Address, City, State, Zip code Phone number, Alt. phone number, Fax number, e-mail address, web site Colitis and Proctitis (Inflammation of the Colon and Rectum) Basics OVERVIEW • “Colitis” is inflammation of the colon • “Proctitis” is inflammation of the rectum GENETICS • Breed susceptibility to histiocytic ulcerative colitis in boxers; histiocytic ulcerative colitis is inflammation characterized by a thickened lining of the colon with varying degrees of loss of the superficial lining (known as “ulceration”); the thickening is due to infiltration of various cells (histiocytes, plasma cells, and lymphocytes) in the layers under the lining • Possible association between inflammation of the colon (colitis) and one or multiple draining tracts around the anus (known as “perianal fistulas”) in German shepherd dogs SIGNALMENT/DESCRIPTION OF PET Species • Dogs • Cats Breed Predilections • Boxers—histiocytic ulcerative colitis; histiocytic ulcerative colitis is inflammation characterized by a thickened lining of the colon with varying degrees of loss of the superficial lining (known as “ulceration”); the thickening is due to infiltration of various cells (histiocytes, plasma cells, and lymphocytes) in the layers under the lining • German shepherd dogs—possible association between inflammation of the colon (colitis) and one or multiple draining tracts around the anus (perianal fistulas) Mean Age and Range • Any age • Boxers usually have clinical signs by 2 years of age SIGNS/OBSERVED CHANGES IN THE PET • Feces vary from semiformed -

Microscopic Colitis: Collagenous Colitis and Lymphocytic Colitis
A SPECIAL ARTICLE Microscopic Colitis: Collagenous Colitis and Lymphocytic Colitis Brennan A. Scott Thomas P. Prindiville Collagenous colitis and lymphocytic colitis are chronic relapsing diarrheal illnesses, which are often referred to together as microscopic colitis. It most commonly occurs in women in their fifth to sixth decade. The symptoms usually include profuse watery diarrhea and crampy abdominal pain. Laboratory and endoscopic studies are gener- ally normal but microscopic inflammation is seen when colonic biopsies are performed. In collagenous colitis there is a subepithelial collagen band in addition to chronic inflammation in the lamina propria. The etiology is not known but multiple theories exist including autoimmune, infectious, and medication-induced. Although the course is generally benign, patients may have multiple relapses over many years. Treatment regimens vary and have included anti-diarrheals, antibiotics, 5-aminosalicylates, steroids, and immunosuppressive agents. INTRODUCTION abdominal pain. Both conditions have normal mucosa ollagenous colitis (CC) (Figure 1) and lympho- when viewed endoscopically, however biopsy speci- cytic colitis (LC) (Figure 2) are uncommon mens show chronic mucosal inflammation. In CC C chronic relapsing diarrheal illnesses. The major- there is a subepithelial collagen band of varying thick- ity of patients are women in their fifth to sixth decade ness in association with an inflammatory cell infiltrate who complain of profuse, watery diarrhea, and crampy in the lamina propria (1). The collagen band is absent in LC (2,3). The term microscopic colitis (MC) was Brennan A. Scott, MD, Clinical Fellow, Division of Gas- originally used to describe patients with chronic diar- troenterology, University of California, Davis Medical rhea and normal endoscopic and barium enema stud- Center. -

Digestive Involvement in Primary Sjögren's Syndrome: Analysis from the Sjögrenser Registry
Digestive involvement in primary Sjögren’s syndrome: analysis from the Sjögrenser registry S. Melchor1, C. Sánchez-Piedra2, M. Fernández Castro3, J.L. Andreu3, V. Martínez Taboada4, A. Olivé5, J. Rosas6, R. Menor7, Á. García-Aparicio8, F.J. López Longo9, S. Manrique-Arija10, J.A. García Vadillo11, R. López-González12, J. Narváez13, C. Galisteo14, J. González Martín15, A. Naranjo16, Ó. Illera17, B. Moreira18, E. Raya19, M. Rodríguez López20, E. Júdez21, C. Moriano22, V. Torrente-Segarra23, B. García Magallón24, C. Guillén Astete25, I. Castellvi26, C. Bohórquez27, J. Loricera4, J. Belzunegui28, P.E. Carreira1, on behalf of the Sjögrenser group, part of the Spanish Society of Rheumatology Systemic Autoimmune Diseases Study Group (EASSER) Affiliations: page S115. ABSTRACT pancreatic involvement presented more Sheila Melchor, Carlos Sánchez-Piedra, Objective. Digestive involvement (DI) central nervous system and renal in- Mónica Fernández Castro, Jose Luis has been reported in 10–30% of prima- volvement, Raynaud’s phenomenon, Andreu, Víctor Martínez Taboada, ry Sjögren’s syndrome (pSS) patients, lymphoma and C3/C4 hypocomplemen- Alejandro Olivé, José Rosas, Raúl Menor, Ángel García-Aparicio, Francisco Javier and few studies have systematically taemia. López Longo, Sara Manrique-Arija, Jesús analysed the prevalence of DI in pSS Conclusion. DI is frequent in Sjög- Alberto García Vadillo, Ruth López- patients. The aim of this study was to renser patients, mainly in the form of González, Javier Narváez, Carlos Galisteo, describe DI prevalence in pSS patients autoimmune disorders, and seem to be Jorge González Martín, Antonio Naranjo, from the Sjögrenser Study, and to ana- associated with a more severe pheno- Óscar Illera, Begoña Moreira, Enrique Raya, Marina Rodríguez López, Enrique lyse its clinical associations. -

Steinberg GI Board Review Course Washington DC September 2016
Steinberg GI Board Review Course Washington DC September 2016 Non-IBD Colitis Christina M. Surawicz, MD Professor of Medicine University of Washington School of Medicine 1 Diagnosing Colitis Classic symptoms of colitis are diarrhea, usually bloody, and abdominal pain. Possible accompanying symptoms include fever, cramps, malaise, nausea, vomiting, chills, and myalgia. The most frequent differential diagnosis of colitis is between acute self-limited colitis (i.e. ASLC or infectious colitis) and first attacks of idiopathic inflammatory bowel disease (IBD). In addition, there are multiple other causes of colitis. TYPES OF COLITIS I. Distinguishing Acute Self-Limited Colitis from Idiopathic Inflammatory Bowel Disease History and Physical Exam. Acute onset suggests infectious colitis, inflammatory bowel disease is usually a chronic illness with a more indolent onset. Fever does favor infectious colitis but the symptoms are otherwise nonspecific. Physical exam is noncontributory. Laboratory evaluation is helpful if the stool culture is positive but this is positive in only 40-60% of patients with acute self-limited colitis. The most common pathogens are Campylobacter, Salmonella, Shigella and E. coli 0157:H7 (Shiga toxin E. coli). Laboratory evaluation is usually nonspecific. Anemia and elevated sed rate (ESR) favor inflammatory bowel disease. Fecal leukocytes are insensitive because they can be seen in both IBD and infectious colitis. Appearance of the colonic mucosa. The appearance suggesting infectious colitis is focal changes, hemorrhage with focal edema and erythema. However, this does not differentiate one infection from another nor is it specific for infectious colitis. Mucosal biopsy can be very helpful in distinguishing between inflammatory bowel disease, especially ulcerative colitis, and acute self-limiting colitis, because crypt distortion which is a hallmark of the former is rare in infectious colitis. -

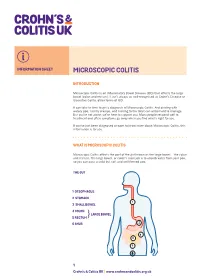
Microscopic Colitis What Is Microscopic Colitis?
Microscopic Colitis What is microscopic colitis? Microscopic colitis is an inflammation of the colon that a health care provider can see only with a microscope. Inflammation is the body’s normal response to injury, irritation, or infection of tissues. Microscopic colitis is a type of inflammatory bowel disease—the general name for diseases that cause irritation and inflammation in the intestines. The two types of microscopic colitis are collagenous colitis and lymphocytic colitis. Health care providers often use the term microscopic colitis to describe both types because their symptoms and treatments are the same. Some scientists believe that collagenous colitis and lymphocytic colitis may be different phases of the same condition rather than separate conditions. In both types of microscopic colitis, an increase in the number of lymphocytes, a type of white blood cell, can be seen in the epithelium—the layer of cells that lines the colon. An increase in the number of white blood cells is a sign of inflammation. The two types of colitis affect the colon tissue in slightly different ways: Lymphocytic colitis. The number of lymphocytes is higher, and the tissues and lining of the colon are of normal thickness. Collagenous colitis. The layer of collagen, a threadlike protein, underneath the epithelium builds up and becomes thicker than normal. When looking through a microscope, the health care provider may find variations in lymphocyte numbers and collagen thickness in different parts of the colon. These variations may indicate an overlap of the two types of microscopic colitis. What causes microscopic colitis? The exact cause of microscopic colitis is unknown. -

Lymphocytic Colitis: a Retrospective Clinical Study of 199 Gut: First Published As 10.1136/Gut.2003.023440 on 11 March 2004
536 INFLAMMATION Lymphocytic colitis: a retrospective clinical study of 199 Gut: first published as 10.1136/gut.2003.023440 on 11 March 2004. Downloaded from Swedish patients M Olesen, S Eriksson, J Bohr, G Ja¨rnerot, C Tysk ............................................................................................................................... Gut 2004;53:536–541. doi: 10.1136/gut.2003.023440 Background: Lymphocytic colitis is characterised by chronic diarrhoea and specific microscopic changes in a macroscopically normal colonic mucosa. We report clinical features and treatment outcome in a large patient cohort. Methods: Patients were searched for in 24 Swedish gastroenterology clinics. The biopsy material was reassessed using strict histopathological criteria. Clinical data were obtained from medical notes. See end of article for Results: Lymphocytic colitis was diagnosed in 199 cases. The female:male ratio was 2.4:1. Median age at authors’ affiliations diagnosis was 59 (48–70) years. The most frequent symptoms were diarrhoea (96%), abdominal pain ....................... (47%), and weight loss (41%). The course was chronic intermittent in 30% of patients, chronic continuous in Correspondence to: 7%, and a single attack in 63%, and in these cases the disease duration was 6 (4–11) months. Seventy Associate Professor nine (40%) patients reported associated diseases, of which thyroid disorders, coeliac disease, and C Tysk, Department of diabetes mellitus were the most common. In 34 first or second degree relatives of 24 (12%) patients, a Medicine, Division of family history of ulcerative colitis, Crohn’s disease, collagenous colitis, or coeliac disease was reported. Gastroenterology, O¨ rebro University Hospital, Drug induced disease was suspected in 19 (10%) patients. A non-significant peak of disease onset was 701 85 O¨ rebro, Sweden; seen in December-January. -

Microscopic Colitis Associated with Exposure to Lansoprazole
LESSONS FROM PRACTICE Microscopic colitis associated with exposure to lansoprazole Clinical record Patient 1* A 78-year-old woman who normally had one to two bowel motions a day presented with a 3-week history of gradual onset of more frequent and looser motions up to six times a day and occasionally at night. She had urgency and episodes of faecal incontinence. Her motions were watery. There was no improvement after she was treated with tinidazole. Her regular medications were alendronate, hydrochlorothiazide, irbesartan, raloxifene, thyroxine, temazepam, aspirin, thiamine, vitamin C, glucosamine, and evening primrose oil. She had also taken lansoprazole (30 mg capsules) daily for 2 months to treat possible reflux. Sigmoidoscopy showed yellowish, watery stool with mucus and a few tiny scattered patches of intramucosal haemorrhage. Biopsy (Figure A) showed mild lymphocytic colitis (defined by the presence of more than one lymphocyte per 20 epithelial cells). Lansoprazole therapy was ceased and the diarrhoea settled within 24 hours. Patient 2* A 53-year-old woman presented to hospital with a 2-month history of diarrhoea and abdominal pain. She was admitted with suspected diverticulitis. Nine months before presentation, she had started taking lansoprazole (30 mg capsules) daily for heartburn. She described having bowel motions seven or eight times per day, and occasionally at night. The diarrhoea had not responded to tinidazole, metronidazole or norfloxacin. Her regular medications were gemfibrozil, tibolone, indapamide and perindopril. Colonoscopy did not detect significant abnormalities. Biopsy showed mild collagenous colitis (Figure B). Lansoprazole therapy was ceased. She was treated with loperamide, then cholestyramine and budesonide. Within 6 months, she was symptom-free without antidiarrhoeal medication. -
Microscopic Colitis (PDF)
INFORMATION SHEET MICROSCOPIC COLITIS INTRODUCTION Microscopic Colitis is an Inflammatory Bowel Disease (IBD) that affects the large bowel (colon and rectum). It isn’t always as well-recognised as Crohn’s Disease or Ulcerative Colitis, other forms of IBD. It can take to time to get a diagnosis of Microscopic Colitis. And dealing with watery poo, tummy cramps, and rushing to the toilet can all be hard to manage. But you’re not alone; we’re here to support you. Many people respond well to treatment and often symptoms go away when you find what’s right for you. If you’ve just been diagnosed or want to know more about Microscopic Colitis, this information is for you. WHAT IS MICROSCOPIC COLITIS Microscopic Colitis affects the part of the gut known as the large bowel – the colon and rectum. The large bowel, or colon’s main job is to absorb water from your poo, so you can pass a solid but soft and well-formed poo. THE GUT 1 OESOPHAGUS 2 STOMACH 1 3 SMALL BOWEL 2 4 COLON LARGE BOWEL 5 RECTUM} 6 ANUS 2 4 3 5 6 1 Crohn’s & Colitis UK | www.crohnsandcolitis.org.uk MICROSCOPIC COLITIS The walls of your bowel have layers. In Microscopic Colitis the inner lining becomes inflamed. But this change can only be seen when a sample of tissue (biopsy) is taken from your colon and looked at under a microscope. BOWEL LAYERS INNER LINING MIDDLE LAYER OUTER LAYER There are two types of Microscopic Colitis: • Lymphocytic Colitis (LC) – where the inner lining has more white blood cells (lymphocytes) than usual. -

Intraepithelial Lymphocytes in the Gastrointestinal Tract: to Celiac Disease and Beyond
6/4/2019 Disclosures Intraepithelial Lymphocytes in the Gastrointestinal Tract: • BHB Therapeutics (spouse is co‐founder) To Celiac Disease and Beyond Soo‐Jin Cho, MD, PhD Current Issues in Anatomic Pathology May 25, 2019 Outline Did you know… • Celiac disease and lymphocytosis of the small bowel • “Sprue” is an Anglicized form of the • Clinical features Dutch word “sprouw,” a term applied • Histopathology in 1669 to a chronic diarrheal disease • Differential diagnosis of unknown etiology accompanied by • Intraepithelial lymphocytes elsewhere in the GI tract aphthous ulcers that was prevalent in • Esophagus Belgium • Stomach • Colon • Other conditions with GI tract lymphocytosis • Drugs (esp. immune checkpoint inhibitors) www.TheAwkwardYeti.com 1 6/4/2019 Celiac disease and other gluten‐related disorders Celiac disease • Celiac disease (CD) • Virtually unknown condition in mid‐20th century • Non‐IgE immune‐mediated • Seroprevalence currently ~1% in European and US populations • Triggered by dietary gluten ingestion • But majority of these individuals have not been diagnosed with celiac disease • In genetically susceptible individuals • Early diagnosis is challenging in children and adults • Non‐celiac gluten sensitivity (NCGS) • Presentation of diagnosed CD has been changing, with shift toward • Patients develop intestinal and extraintestinal symptoms after gluten exposure older individuals with milder disease • Do NOT meet criteria for CD or WA • Increased awareness • Wheat allergy (WA) • Better diagnostics • Hypersensitivity reaction -

Increased Production of Lysozyme Associated with Bacterial
ANTICANCER RESEARCH 35: 6365-6372 (2015) Review Increased Production of Lysozyme Associated with Bacterial Proliferation in Barrett’s Esophagitis, Chronic Gastritis, Gluten-induced Atrophic Duodenitis (Celiac Disease), Lymphocytic Colitis, Collagenous Colitis, Ulcerative Colitis and Crohn’s Colitis CARLOS A. RUBIO Department of Pathology, Karolinska Instutute and University Hospital, Stockholm, Sweden Abstract. The mucosa of the esophagus, the stomach, the resistance to anti-bacterial drugs. Further research on natural small intestine, the large intestine and rectum are anti-bacterial enzymes such as lysozyme, appears mandatory. unremittingly challenged by adverse micro-environmental factors, such as ingested pathogenic and non-pathogenic The cells that line the mucosa of the human gastrointestinal bacteria, and harsh secretions with digestive properties with (GI) tract are continuously exposed to adverse micro- disparate pH, as well as bacteria and secretions from environmental conditions, such as digestive juices of upstream GI organs. Despite the apparently inauspicious different pH, a wide variety of active natural enzymes and mixture of secretions and bacteria, the normal GI mucosa large amount of bacteria. The density of the bacterial flora retains a healthy state of cell renewal. To by-pass the tough in the GI tract is huge; it varies from 103/ml near the gastric microenvironment, the epithelia of the GI react by speeding- outlet to 1010/ml at the ileo-cecal valve to 1011 to 1012/ml in up cell exfoliation, by increasing peristalsis, eliminating the colon. The total microbial population (aproximatelly bacteria through secretion of plasma cell-immunoglobulins 1014) exceeds the total number of cells in the GI tract. About and by increasing production of natural antibacterial enzymes 500 to 1,000 different species exist, a biomass that weights (lysozyme) and host defense peptides (defensin-5).