Assessing Value in Ontario Health Links. Part 3: Measures of System Performance in Ontario’S Health Links
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2021 Market Rent Index & Indices for Non-Profit Projects
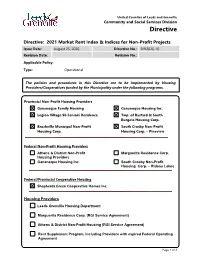
United Counties of Leeds and Grenville Community and Social Services Division Directive Directive: 2021 Market Rent Index & Indices for Non-Profit Projects Issue Date: August 25, 2020 Directive No.: DIR2020-10 Revision Date: Revision No.: Applicable Policy: Type: Operational The policies and procedures in this Directive are to be implemented by Housing Providers/Cooperatives funded by the Municipality under the following programs. Provincial Non-Profit Housing Providers Gananoque Family Housing Gananoque Housing Inc. Legion Village 96 Seniors Residence Twp. of Bastard & South Burgess Housing Corp. Brockville Municipal Non-Profit South Crosby Non-Profit Housing Corp. Housing Corp. – Pineview Federal Non-Profit Housing Providers Athens & District Non-Profit Marguerita Residence Corp. Housing Providers Gananoque Housing Inc. South Crosby Non-Profit Housing Corp. – Rideau Lakes Federal/Provincial Cooperative Housing Shepherds Green Cooperative Homes Inc. Housing Providers Leeds Grenville Housing Department Marguerita Residence Corp. (RGI Service Agreement) Athens & District Non-Profit Housing (RGI Service Agreement) Rent Supplement Program, including Providers with expired Federal Operating Agreement Page 1 of 3 United Counties of Leeds and Grenville Community and Social Services Division Directive Directive: 2021 Market Rent Index & Indices for Non-Profit Projects Issue Date: August 25, 2020 Directive No.: DIR2020-10 Revision Date: Revision No.: BACKGROUND Each year, the Ministry provides indices for costs and revenues to calculate subsidies under the Housing Services Act (HSA). The indices to be used for 2021 are contained in this directive. PURPOSE The purpose of this directive is to advise housing providers of the index factors to be used in the calculation of subsidy for 2021. ACTION TO BE TAKEN Housing providers shall use the index factors in the table below to calculate subsidies under the Housing Services Act, 2011 (HSA) on an annual basis. -
DIRECTORY Répertoire 2018 TABLE of CONTENTS Table Des Matières
CRAWFORD DIRECTORY Répertoire 2018 TABLE OF CONTENTS Table des Matières 3 EXECUTIVE CONTACTS Contacts exécutifs 4 National Claims Management Centre (NCMC) Contacts Centre de Gestion de Réclamations National, Contrats 6 Global Technical Services (GTS®) Contacts Services Techniques Mondiaux, Contrats 8 Contractor Connection® Contacts Connection Contracteur, Contrats 10 ALBERTA 13 BRITISH COLUMBIA Colombie-Britannique 16 MANITOBA 17 NEW BRUNSWICK Nouveau-Brunswick 19 NEWFOUNDLAND & LABRADOR Terre-Neuve-et-Labrador 20 NORTHWEST TERRITORIES Territoires du Nord-Ouest 21 NOVA SCOTIA Nouvelle-Écosse 24 ONTARIO 40 PRINCE EDWARD ISLAND l’Île-du-Prince-Édouard 41 QUÉBEC 45 SASKATCHEWAN EXECUTIVE CONTACTS CONTACTS EXECUTIVE EXECUTIVE CONTACTS Contacts exécutifs Pat Van Bakel, Heather Matthews President and CEO, Senior Vice President, Crawford & Company (Canada) Inc. National Claims Management Centre Président et chef de la direction Vice-présidente senior, centre national Crawford & Compagnie (Canada) inc. de gestion des réclamations Contacts exécutifs 55 University Avenue, Suite 400 539 Riverbend Dr. P.O. Box 36 Kitchener, ON N2K 3S3 Toronto, ON, M5J 2H7 Tel: 519 578 5540 x2672 Tel: 416 957 5003 Fax: 519 578 2868 [email protected] [email protected] Jim Eso Greg Smith Senior Vice President, Senior Vice President, Property & Casualty Administration Vice-président senior et Expert en Vice-président senior de dommages direct et accidents l’administration 539 Riverbend Dr. 55 University Avenue, Suite 400 Kitchener, ON N2K 3S3 P.O. Box 36 Tel: 519 578 5540 x2681 Toronto, ON, M5J 2H7 Fax: 519 578 2868 Tel: 416 957 5012 [email protected] Fax: 416 364 1641 [email protected] Gary Gardner Senior Vice President, Global Client Development Vice-président senior, Développement clients international 55 University Avenue, Suite 400 P.O. -

Freedom Liberty
2013 ACCESS AND PRIVACY Office of the Information and Privacy Commissioner Ontario, Canada FREEDOM & LIBERTY 2013 STATISTICS In free and open societies, governments must be accessible and transparent to their citizens. TABLE OF CONTENTS Requests by the Public ...................................... 1 Provincial Compliance ..................................... 3 Municipal Compliance ................................... 12 Appeals .............................................................. 26 Privacy Complaints .......................................... 38 Personal Health Information Protection Act (PHIPA) .................................. 41 As I look back on the past years of the IPC, I feel that Ontarians can be assured that this office has grown into a first-class agency, known around the world for demonstrating innovation and leadership, in the fields of both access and privacy. STATISTICS 4 1 REQUESTS BY THE PUBLIC UNDER FIPPA/MFIPPA There were 55,760 freedom of information (FOI) requests filed across Ontario in 2013, nearly a 6% increase over 2012 where 52,831 were filed TOTAL FOI REQUESTS FILED BY JURISDICTION AND RECORDS TYPE Personal Information General Records Total Municipal 16,995 17,334 34,329 Provincial 7,029 14,402 21,431 Total 24,024 31,736 55,760 TOTAL FOI REQUESTS COMPLETED BY JURISDICTION AND RECORDS TYPE Personal Information General Records Total Municipal 16,726 17,304 34,030 Provincial 6,825 13,996 20,821 Total 23,551 31,300 54,851 TOTAL FOI REQUESTS COMPLETED BY SOURCE AND JURISDICTION Municipal Provincial Total -

List of Streets in Toronto East York That Can Be Converted to Permit Parking Page 1 of 53
List of streets in Toronto East York that can be converted to Permit Parking Page 1 of 53 Ward Street Between Length (m) 14 Budapest Lane Lake Shore Boulevard West and the south end of Budapest Lane 35.4 14 Cowan Avenue Milky Way and Queen Street West 49.0 T.T.C loop immediately south of Springhurst Avenue and 14 Dufferin Street Springhurst Avenue 84.8 Dundas Street West and Lane first west of Dundas Street West 14 Edna Avenue north of Edna Avenue 41.4 Lane first east of Dorval Road north of Edna Avenue and Dorval 14 Edna Avenue Road 45.3 Lane first west of Dundas Street West north of Edna Avenue and 14 Edna Avenue Lane first east of Dorval Road north of Edna Avenue 77.1 14 Elm Grove Avenue Milky Way and Queen Street West 49.7 14 Fraser Avenue Liberty Street and King Street West 215.7 14 Fraser Avenue The south end of Fraser Avenue and Liberty Street 276.0 14 Glenavon Road Dowling Avenue and the west end of Glenavon Road 93.7 14 Gwynne Avenue Milky Way and Queen Street West 50.0 Bloor Street West and Lane first north of Bloor Street West east 14 Indian Road of Indian Road 48.0 Lane first north of Bloor Street West east of Indian Road and 14 Indian Road Edna Avenue 50.8 Lane first south of King Street West east of Jefferson Avenue and 14 Jefferson Avenue King Street West 147.1 Lane first south of Liberty Street east of Jefferson Avenue and 14 Jefferson Avenue Liberty Street 65.9 Liberty Street and Lane first south of King Street West east of 14 Jefferson Avenue Jefferson Avenue 68.1 The south end of Jefferson Avenue and Lane first south -

Old Town Toronto East
ST NTO EA TORO TOWN OLD Come and explore Toronto’s historic heart. N Sherbourne S Sac 5 kvi Geo ll Queen Street East e St rge Sum Bri Stre 4 ght Pow tre ach et Stre et er St Stre ree et St. t et Richmond Street East La Ber wre keley nce St Str 2 3 reet East ee Sac g Street t Adelaide Street East Kin kvi lle Str Jar Parli Bayv ee vis 6 t ament iew Cyp Street 1 ue Av St ven ress by Eri King Street East 7 enue Street Der n A n St ter St Eas ree E W t 14 Front Street East Don Ri Ove Tri 13 12 nity rend 11 ver St St reet The Esplanade 9 Mill Street Che 1O rry Geo 8 Street rge Scadding Ave Hah St South n Pl Longboat Avenue Lakeshore Blvd S Legend_ The Daniel Brooke Building 6 Little Trinity Church & Parish House 11 The Berkeley Street Theatre Bus, Streetcar Route Architectural/ 1 Historical 2 The Bank of Upper Canada 7 Enoch Turner School House 12 Canadian Opera Company Municipal Parking Interest 3 Toronto’s First Post Office 8 The Distillery Historic District 13 The Lorraine Kimsa Theatre Outdoor Art, Museum for Young People d Nixon 9 First Parliament Buildings Site One-way Street Statues & St. Paul’s Basilica 14 The Toronto Sun Mural Structures 4 10 Crombie Park Greenspace 5 Dominion Square riting: Edwar W EAST RONTO OWN TO OLD T Come and explore Toronto’s historic heart. Points of interest 1 The Daniel Brooke Building (King outskirts of town and the only Roman 9 First Parliament Buildings Site, Street East & Jarvis Street) Built in Catholic parish between Kingston and Parliament Square The block bounded 1833 for merchant Daniel Brooke, Windsor. -

The Canadian Parliamentary Guide
NUNC COGNOSCO EX PARTE THOMAS J. BATA LI BRARY TRENT UNIVERSITY us*<•-« m*.•• ■Jt ,.v<4■■ L V ?' V t - ji: '^gj r ", •W* ~ %- A V- v v; _ •S I- - j*. v \jrfK'V' V ■' * ' ’ ' • ’ ,;i- % »v • > ». --■ : * *S~ ' iJM ' ' ~ : .*H V V* ,-l *» %■? BE ! Ji®». ' »- ■ •:?■, M •* ^ a* r • * «'•# ^ fc -: fs , I v ., V', ■ s> f ** - l' %% .- . **» f-•" . ^ t « , -v ' *$W ...*>v■; « '.3* , c - ■ : \, , ?>?>*)■#! ^ - ••• . ". y(.J, ■- : V.r 4i .» ^ -A*.5- m “ * a vv> w* W,3^. | -**■ , • * * v v'*- ■ ■ !\ . •* 4fr > ,S<P As 5 - _A 4M ,' € - ! „■:' V, ' ' ?**■- i.." ft 1 • X- \ A M .-V O' A ■v ; ■ P \k trf* > i iwr ^.. i - "M - . v •?*»-• -£-. , v 4’ >j- . *•. , V j,r i 'V - • v *? ■ •.,, ;<0 / ^ . ■'■ ■ ,;• v ,< */ ■" /1 ■* * *-+ ijf . ^--v- % 'v-a <&, A * , % -*£, - ^-S*.' J >* •> *' m' . -S' ?v * ... ‘ *•*. * V .■1 *-.«,»'• ■ 1**4. * r- * r J-' ; • * “ »- *' ;> • * arr ■ v * v- > A '* f ' & w, HSi.-V‘ - .'">4-., '4 -' */ ' -',4 - %;. '* JS- •-*. - -4, r ; •'ii - ■.> ¥?<* K V' V ;' v ••: # * r * \'. V-*, >. • s s •*•’ . “ i"*■% * % «. V-- v '*7. : '""•' V v *rs -*• * * 3«f ' <1k% ’fc. s' ^ * ' .W? ,>• ■ V- £ •- .' . $r. « • ,/ ••<*' . ; > -., r;- •■ •',S B. ' F *. ^ , »» v> ' ' •' ' a *' >, f'- \ r ■* * is #* ■ .. n 'K ^ XV 3TVX’ ■■i ■% t'' ■ T-. / .a- ■ '£■ a« .v * tB• f ; a' a :-w;' 1 M! : J • V ^ ’ •' ■ S ii 4 » 4^4•M v vnU :^3£'" ^ v .’'A It/-''-- V. - ;ii. : . - 4 '. ■ ti *%?'% fc ' i * ■ , fc ' THE CANADIAN PARLIAMENTARY GUIDE AND WORK OF GENERAL REFERENCE I9OI FOR CANADA, THE PROVINCES, AND NORTHWEST TERRITORIES (Published with the Patronage of The Parliament of Canada) Containing Election Returns, Eists and Sketches of Members, Cabinets of the U.K., U.S., and Canada, Governments and Eegisla- TURES OF ALL THE PROVINCES, Census Returns, Etc. -

Consultation Guide Final
Citizens Talking to Citizens Public Consultation Guide Ontario Citizens’ Assembly on Electoral Reform Contact Information Print copies of this document are available at ServiceOntario/Government Information Centres in more than 60 communities around the province. For the location closest to you, please visit www.serviceontario.ca. Electronic copies are available in .pdf.Visit the Citizens’Assembly website at www.citizensassembly.gov.on.ca. Alternative-format copies are available on request at [email protected] Une publication équivalente est disponible en français au site web suivant : www.assembleedescitoyens.gouv.on.ca. © Queen’s Printer for Ontario, 2006 O ntario has changed significantly since Get Involved our first parliament was elected in 1792. Since that time the electoral system has The Assembly would like to hear from as never been publicly considered or evaluated. many Ontarians as possible: those who Some people think the current system know a lot about electoral systems, and has stood the test of time. Other people those who are just beginning to think or think it’s time for a change.The Citizens’ learn about the subject.The consultation Assembly process gives all Ontarians an period will run from late October 2006 to opportunity to learn more about Ontario’s the end of January 2007.What you tell us current electoral system, as well as others, will assist the Assembly when we discuss and to decide which one they think is what to recommend to the government. best for this province. This guide will help you present your The Citizens’ Assembly wants to ideas to the Assembly, however you hear what you think. -

Toronto North and East Office Market Report
First Quarter 2019 / Office Market Report Toronto North & East Quick Stats Leasing activity in the Toronto North its downward trend, dropping 30 bps 9.2% and East office markets started 2019 on during the quarter (the fourth consecutive North Yonge class A office a positive note, building on the overall quarter with a drop), but has risen 50 bps vacancy rate success of 2018. Collectively, occupancy year-over-year to 6.7%. The North market’s levels increased by 85,000 square feet (sf) most notable lease transactions during 34% with class C buildings marginally making up the quarter were in North Yonge, where Hwy. 404 & Steeles sublet the bulk of the gain. Quarter-over-quarter, Questrade consolidated operations from two available space as a percentage availability declined by 40 basis points (bps) buildings into one and extended its lease at of total available space to 11.3% while overall vacancy fell 40 bps Manulife’s North American Centre (105,000 to 7.1%. The amount of space on the sublet sf) and tech firm Alithya Technology leased a market increased by almost 250,000 sf full floor in RioCan’s 2 Sheppard Ave. E. 88,227 sf quarter-over-quarter, offering nearly 920,000 Sublet available area in Toronto After years in flux, Menkes Developments sf – mainly credited to new offerings in the North, vs. 829,143 sf in has reached a settlement with the City of Toronto East East market. Toronto for its development at 4800 Yonge Toronto North saw occupancy levels fall by St. (at the southwest corner of Yonge St. -

For a List of All Advisors Please Click Here
Ministry of Heritage, Sport, Tourism and Culture Industries Ministry for Seniors and Accessibility Regional Services and Corporate Support Branch – Contact List Region and Office Staff Member Program Delivery Area Central Region Laura Lee Dam Not Applicable Toronto Office Manager 400 University Avenue, 2nd Floor Toronto, Ontario M7A 2R9 Email: [email protected] Phone: (519) 741-7785 Central Region Roya Gabriele Not Applicable Toronto Office Regional Coordinator 400 University Avenue, 2nd Floor Toronto, Ontario M7A 2R9 Email: [email protected] Phone: (647) 631-8951 Central Region Sherry Gupta Not Applicable Toronto Office Public Affairs and Program 400 University Avenue, 2nd Coordinator Floor Toronto, Ontario M7A 2R9 Email: [email protected] Phone: (647) 620-6348 Central Region Irina Khvashchevskaya Toronto West (west of Bathurst Street, north to Steeles Toronto Office Regional Development Advisor Avenue) and Etobicoke 400 University Avenue, 2nd Sport/Recreation, Culture/Heritage, Floor Toronto, Ontario M7A 2R9 Seniors and Accessibility Portfolios Email: [email protected] Phone: (647) 629-4498 Central Region, Bilingual Mohamed Bekkal Toronto East (east of Don Valley Parkway, north to Steeles Toronto Office Regional Development Advisor Avenue) and Scarborough 400 University Avenue, 2nd Sport/Recreation, Culture/Heritage, Floor Toronto, Ontario M7A 2R9 Seniors and Accessibility Portfolios Francophone Organizations in Toronto Email: [email protected] Phone: (416) 509-5461 Central Region Shannon Todd -

Regional Development Advisor
Ministry of Heritage, Sport, Tourism and Culture Industries Ministry for Seniors and Accessibility Regional Services Branch – Contact List Region and Office Staff Member Program Delivery Area Central Region Laura Lee Dam Not Applicable Toronto Office Manager 400 University Avenue, 2nd Floor Toronto, Ontario M7A Email: [email protected] 2R9 Phone: (519) 741-7785 Central Region Roya Gabriele Not Applicable Toronto Office Regional Coordinator 400 University Avenue, 2nd Floor Toronto, Ontario M7A Email: [email protected] 2R9 Phone: (647) 631-8951 Central Region Heather Gushulak Not Applicable Toronto Office Public Affairs and Program Coordinator 400 University Avenue, 2nd Floor Toronto, Ontario M7A Email: [email protected] 2R9 Phone: (647) 620-6348 Central Region Irina Khvashchevskaya Toronto West (west of Bathurst Street, north to Steeles Toronto Office Regional Development Advisor Avenue) and Etobicoke 400 University Avenue, 2nd Sport/Recreation, Culture/Heritage, Floor Toronto, Ontario M7A Seniors and Accessibility Portfolios 2R9 Email: [email protected] Phone: (647) 629-4498 Central Region, Bilingual Mohamed Bekkal Toronto East (east of Don Valley Parkway, north to Toronto Office Regional Development Advisor Steeles Avenue) and Scarborough 400 University Avenue, 2nd Sport/Recreation, Culture/Heritage, Floor Toronto, Ontario M7A Seniors and Accessibility Portfolios Francophone Organizations in Toronto 2R9 Email: [email protected] Phone: (416) 509-5461 Central Region Shannon Todd Toronto Central -

2021 Market Rent Index and Indices for Non-Profit Projects (Revised)
Jeeds(~ United Counties of Leeds and Grenville Gl'env1Tle Community and Social Services Division Directive Directive: 2021 Market Rent Index & Indices for Non-Profit Projects (Revised) Issue Date: August 25, 2020 Directive No.: DI R2020-10 Revision Date: December 18, 2020 Revision No.: 1 Applicable Policy: Type: Operational The policies and procedures in this Directive are to be implemented by Housing Providers/Cooperatives funded by the Municipality under the following programs. Provincial Non-Profit Housing Providers ~ Gananoque Family Housing ~ Gananoque Housing Inc. ~ Legion Village 96 Seniors Residence ~ Twp. of Bastard & South Burgess Housing Corp. ~ Brockville Municipal Non-Profit ~ South Crosby Non-Profit Housing Corp. Housing Corp. - Pineview Federal Non-Profit Housing Providers D Athens & District Non-Profit D Marguerita Residence Corp. Housing Providers D Gananoque Housing Inc. D South Crosby Non-Profit Housing Corp. - Rideau Lakes Federal/Provincial Cooperative Housing ~ Shepherds Green Cooperative Homes Inc. Housing Providers D Leeds Grenville Housing Department D Marguerita Residence Corp. (RGI Service Agreement) D Athens & District Non-Profit Housing (RGI Service Agreement) D Rent Supplement Program, including Providers with expired Federal Operating Agreement Page 1 of 3 J PedsC:~ United Counties of Leeds and Grenville Gretlv1TTe Community and Social Services Division Directive Directive: 2021 Market Rent Index & Indices for Non-Profit Projects (Revised) Issue Date: August 25, 2020 Directive No.: D1R2020-10 Revision Date: December 18, 2020 Revision No.: 1 BACKGROUND Each year, the Ministry provides indices for costs and revenues to calculate subsidies under the Housing Services Act (HSA) . The indices to be used for 2021 are contained in this directive. As you are aware, in late-September the province passed Bill 204, the Helping Tenants and Small Businesses Act, 2020. -

Our History Through the Eyes of Those Before Us… a Legacy of Gratitude Ontario Regional Conference (ORC) History
History of AA in 1 Ottawa Bob E/Caroline C AA Volume 1 ORC Archives Newsletter Our history through the eyes of those before us… A legacy of gratitude Inside this issue: Creating and saving our history Ontario Regional Conference (ORC) History David T. A Brief History of the Ontario Regional States, at Maple Leaf Gardens in Toronto, Eddy G Conference July 2-4. Local A.A. members had to Peter N December 16, 1943 our first dinner was held guarantee its financial viability. It was a part Bryan DeS at the Royal York Hotel with 80 people of their bid process. Fortunately, they didn’t present. A.A. had been successfully have to dig in their pockets as it was a established in Canada for almost one year. success. This dinner is now known as the Ontario The ORC was cancelled in 1965, as it was in Regional Conference banquet. 2005, when Toronto became the first city to January 28, 1944, a celebration was held to host the International Convention a second open “1170” Yonge Street, which, at the time time. In 1993, a convention was held at the was an office, clubhouse and whatever A.A. Toronto Convention Centre to celebrate 50 needed. “1170” was used for the annual Years of A.A. in Canada, and it also replaced celebration in 1945. the ORC. In 1946, 1947 and 1949, the celebration The name Ontario Regional Conference moved to Knights of Columbus Hall on evolved over time. In 1948 and 1949, Sherbourne Street. references were made to the Toronto Region In 1948, Bill and Lois came to Toronto and of Alcoholics Anonymous and a Regional the celebration was held on Saturday, Conference.