A Randomized, Double Blind, Placebo-Controlled Trial to Investigate the Effects of Vitamin C, Hydrocortisone, and Thiamine on the Outcome of Patients with Sepsis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Guidelines on Food Fortification with Micronutrients
GUIDELINES ON FOOD FORTIFICATION FORTIFICATION FOOD ON GUIDELINES Interest in micronutrient malnutrition has increased greatly over the last few MICRONUTRIENTS WITH years. One of the main reasons is the realization that micronutrient malnutrition contributes substantially to the global burden of disease. Furthermore, although micronutrient malnutrition is more frequent and severe in the developing world and among disadvantaged populations, it also represents a public health problem in some industrialized countries. Measures to correct micronutrient deficiencies aim at ensuring consumption of a balanced diet that is adequate in every nutrient. Unfortunately, this is far from being achieved everywhere since it requires universal access to adequate food and appropriate dietary habits. Food fortification has the dual advantage of being able to deliver nutrients to large segments of the population without requiring radical changes in food consumption patterns. Drawing on several recent high quality publications and programme experience on the subject, information on food fortification has been critically analysed and then translated into scientifically sound guidelines for application in the field. The main purpose of these guidelines is to assist countries in the design and implementation of appropriate food fortification programmes. They are intended to be a resource for governments and agencies that are currently implementing or considering food fortification, and a source of information for scientists, technologists and the food industry. The guidelines are written from a nutrition and public health perspective, to provide practical guidance on how food fortification should be implemented, monitored and evaluated. They are primarily intended for nutrition-related public health programme managers, but should also be useful to all those working to control micronutrient malnutrition, including the food industry. -

Validation of Hplc Method for Determination of Thiamine Hydrochloride, Riboflavin, Nicotinamide, and Pyridoxine Hydrochl0ride in Syrup Preparation
Canadian Journal on Scientific and Industrial Research Vol. 2 No. 7, August 20ll VALIDATION OF HPLC METHOD FOR DETERMINATION OF THIAMINE HYDROCHLORIDE, RIBOFLAVIN, NICOTINAMIDE, AND PYRIDOXINE HYDROCHL0RIDE IN SYRUP PREPARATION NOVI YANTIH*, DIAH WIDOWATI, WARTINI, TIWI ARYANI Faculty of Pharmacy, University of Pancasila Email: novi_yantih @ yahoo.com Faculty of Pharmacy, University of Pancasila, Srengseng Sawah, Jagakarsa, 12640 South Jakarta, Indonesia ABSTRACT Multivitamin syrup containing various substances of varying characteristics may have a problem in quantitative analysis. This research has developed and validated of HPLC method for determination of four vitamin components, that is thiamine hydrochloride, riboflavin, nicotinamide, and pyridoxine hydrochloride in syrup multivitamin-mineral. The chromatographic separation was achieved by using a C18 column with dimension of 3.9x300mm and particle size of l0µm. A mixture of methanol - l% acetic acid by using 7mM 1-hexane sulphonic acid sodium salt (20:80) as mobile phase with flow rate of 1 mL/min. The effluent was monitored at 280 nm. Effective separation and quantification was achieved in less than 20 min. That method was simple, accurate, precise, and could be successfully applied for the analysis of thiamine hydrochloride, riboflavin, nicotinamide, and pyridoxine hydrochloride syrup multivitamin- mineral. Keywords: Thiamine hydrochloride, riboflavin, nicotinamide, pyridoxine hydrochloride, syrup, HPLC. 269 270 INTRODUCTION Syrup multivitamin and mineral preparations containing various substances of varying characteristics may have many problems in quantitative analysis. High performance liquid chromatography (HPLC) due to its high capacity in separating a mixture of substances was applicable in determining each component in multivitamin preparations simultaneously. Several investigator have reported the used of HPLC methods for the determination of water-soluble vitamins, such as thiamine hydrochloride, riboflavin, nicotinarnide, and pyridoxine hydrochloride in pharmaceuticals preparations [l,2,3]. -
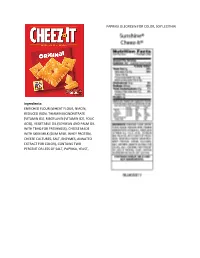
Enriched Flour
PAPRIKA OLEORESIN FOR COLOR, SOY LECITHIN. Ingredients: ENRICHED FLOUR (WHEAT FLOUR, NIACIN, REDUCED IRON, THIAMIN MONONITRATE [VITAMIN B1], RIBOFLAVIN [VITAMIN B2], FOLIC ACID), VEGETABLE OIL (SOYBEAN AND PALM OIL WITH TBHQ FOR FRESHNESS), CHEESE MADE WITH SKIM MILK (SKIM MILK, WHEY PROTEIN, CHEESE CULTURES, SALT, ENZYMES, ANNATTO EXTRACT FOR COLOR), CONTAINS TWO PERCENT OR LESS OF SALT, PAPRIKA, YEAST, INGREDIENTS CRUST: WHOLE GRAIN OATS, ENRICHED FLOUR (WHEAT FLOUR, NIACIN, REDUCED IRON, VITAMIN B1 [THIAMIN MONONITRATE], VITAMIN B2 [RIBOFLAVIN], FOLIC ACID), WHOLE WHEAT FLOUR, SOYBEAN AND/OR CANOLA OIL, SOLUBLE CORN FIBER, SUGAR, DEXTROSE, FRUCTOSE, CALCIUM CARBONATE, WHEY, WHEAT BRAN, SALT, CELLULOSE, POTASSIUM BICARBONATE, NATURAL AND ARTIFICIAL FLAVOR, CINNAMON, MONO- AND DIGLYCERIDES, SOY LECITHIN, WHEAT GLUTEN, NIACINAMIDE, VITAMIN A PALMITATE, CARRAGEENAN, ZINC OXIDE, REDUCED IRON, GUAR GUM, VITAMIN B6 (PYRIDOXINE HYDROCHLORIDE), VITAMIN B1 (THIAMIN HYDROCHLORIDE), VITAMIN B2 (RIBOFLAVIN), FILLING: INVERT SUGAR, CORN SYRUP, APPLE PUREE CONCENTRATE, GLYCERIN, SUGAR, MODIFIED CORN STARCH, SODIUM ALGINATE, MALIC ACID, METHYLCELLULOSE, DICALCIUM PHOSPHATE, CINNAMON, CITRIC ACID, CARAMEL COLOR. CONTAINS WHEAT, MILK AND SOY INGREDIENTS CRUST: WHOLE GRAIN OATS, ENRICHED FLOUR (WHEAT FLOUR, NIACIN, REDUCED IRON, VITAMIN B1 [THIAMIN MONONITRATE], VITAMIN B2 [RIBOFLAVIN], FOLIC ACID), WHOLE WHEAT FLOUR, SOYBEAN AND/OR CANOLA OIL, SOLUBLE CORN FIBER, SUGAR, DEXTROSE, FRUCTOSE, CALCIUM CARBONATE, WHEY, WHEAT BRAN, SALT, CELLULOSE, POTASSIUM -

Circulatory and Urinary B-Vitamin Responses to Multivitamin Supplement Ingestion Differ Between Older and Younger Adults
nutrients Article Circulatory and Urinary B-Vitamin Responses to Multivitamin Supplement Ingestion Differ between Older and Younger Adults Pankaja Sharma 1,2 , Soo Min Han 1 , Nicola Gillies 1,2, Eric B. Thorstensen 1, Michael Goy 1, Matthew P. G. Barnett 2,3 , Nicole C. Roy 2,3,4,5 , David Cameron-Smith 1,2,6 and Amber M. Milan 1,3,4,* 1 The Liggins Institute, University of Auckland, Auckland 1023, New Zealand; [email protected] (P.S.); [email protected] (S.M.H.); [email protected] (N.G.); [email protected] (E.B.T.); [email protected] (M.G.); [email protected] (D.C.-S.) 2 Riddet Institute, Palmerston North 4474, New Zealand; [email protected] (M.P.G.B.); [email protected] (N.C.R.) 3 Food & Bio-based Products Group, AgResearch, Palmerston North 4442, New Zealand 4 High-Value Nutrition National Science Challenge, Auckland 1023, New Zealand 5 Department of Human Nutrition, University of Otago, Dunedin 9016, New Zealand 6 Singapore Institute for Clinical Sciences, Agency for Science, Technology, and Research, Singapore 117609, Singapore * Correspondence: [email protected]; Tel.: +64-(0)9-923-4785 Received: 23 October 2020; Accepted: 13 November 2020; Published: 17 November 2020 Abstract: Multivitamin and mineral (MVM) supplements are frequently used amongst older populations to improve adequacy of micronutrients, including B-vitamins, but evidence for improved health outcomes are limited and deficiencies remain prevalent. Although this may indicate poor efficacy of supplements, this could also suggest the possibility for altered B-vitamin bioavailability and metabolism in older people. -

About Thiamine (B1) and Thiamine Deficiency
NLOSS North London Obesity Surgery Service About Thiamine (B1) and Thiamine Deficiency What does thiamine do? Thiamine (vitamin B1) is an important nutrient for taking energy from food and turning it into energy for your brain, nerves and heart. It is needed by the body to process carbohydrates, fats, and proteins – but it is most important for how we process carbohydrates (sugars and starches). What happens if my thiamine is low/if I don’t get enough thiamine? Your body stores very little thiamine, so deficiency can happen very quickly – especially if you are not eating much or if you are vomiting for any reason. Thiamine deficiency may be called Beriberi or Wernicke’s Encephalopathy depending on how it presents. When you don’t get enough thiamine, you may first have nausea, vomiting, loss of appetite, fatigue and difficulty concentrating. You may also have weakness, sleepiness, changes in personality and memory, leg and foot cramping, burning feet, headache, constipation, and cramping. If thiamine deficiency is severe, serious problems can result including loss of hearing, permanent nerve damage, coma, permanent brain damage, heart damage, liver damage, and death. What are other symptoms? Other symptoms of thiamine deficiency include: • Blurred or double vision • Difficulty urinating • Difficulty taking/swallowing • Numb/painful hands/feet • Facial weakness • Foot drop, leg weakness • Amnesia, memory loss, dementia • Clumsiness, loss of balance, • Rapid heartbeat falling • Faintness on standing up • Loss of muscle • Leg swelling Where can I get thiamine? Thiamine is found throughout the diet, but fortified cereals, beans/peas, nuts and pork are very good sources. Other sources are also milk, cheese, fresh and dried fruit, and eggs. -

Development of a Multivariable Prediction Model for Identification of Patients at Risk for Medication Transfer Errors at ICU Discharge
RESEARCH ARTICLE Development of a multivariable prediction model for identification of patients at risk for medication transfer errors at ICU discharge 1,2 1,3 2,4 Liesbeth B. E. BosmaID *, Nienke van Rein , Nicole G. M. Hunfeld , Ewout W. Steyerberg5, Piet H. G. J. Melief6, Patricia M. L. A. van den Bemt2 1 Haga Teaching Hospital, Department of Clinical Pharmacy, Els Borst-Eilersplein CH, The Hague, The Netherlands, 2 Erasmus University Medical Center, Department of Hospital Pharmacy, CA, Rotterdam, The Netherlands, 3 Leiden University Medical Center, Department of Clinical Pharmacy and Toxicology, Leiden, The Netherlands, 4 Erasmus University Medical Center, Department of Intensive Care, CA, Rotterdam, The a1111111111 Netherlands, 5 Clinical Biostatistics and Medical Decision Making at Erasmus MC, Rotterdam and Leiden a1111111111 University Medical Center, ZA Leiden, The Netherlands, 6 Haga Teaching Hospital, Department of Intensive Care, CH, The Hague, The Netherlands a1111111111 a1111111111 * [email protected] a1111111111 Abstract OPEN ACCESS Introduction Citation: Bosma LBE, van Rein N, Hunfeld NGM, Steyerberg EW, Melief PHGJ, van den Bemt PMLA Discharge from the intensive care unit (ICU) is a high-risk process, leading to numerous (2019) Development of a multivariable prediction potentially harmful medication transfer errors (PH-MTE). PH-MTE could be prevented by model for identification of patients at risk for medication reconciliation by ICU pharmacists, but resources are scarce, which renders the medication transfer errors at ICU discharge. PLoS ONE 14(4): e0215459. https://doi.org/10.1371/ need for predicting which patients are at risk for PH-MTE. The aim of this study was to journal.pone.0215459 develop a prognostic multivariable model in patients discharged from the ICU to predict who Editor: Shane Patman, University of Notre Dame is at increased risk for PH-MTE after ICU discharge, using predictors of PH-MTE that are Australia, AUSTRALIA readily available at the time of ICU discharge. -

Safety and Efficacy of Vitamin C, Vitamin B1, and Hydrocortisone In
European Journal of Molecular & Clinical Medicine ISSN 2515-8260 Volume 08, Issue 02, 2021 Safety and Efficacy of Vitamin C, Vitamin B1, and Hydrocortisone in clinical outcome of septic shock receiving standard care: A quasi experimental randomized open label two arm parallel group study Dr. Kondle Raghu1*, Dr. Krishnan Ramalingam2 1Department of Medical Sciences, Lincoln University College, Malaysia, 2Department of Biochemistry, Narayana Medical College, Chinthareddypalem, Nellore, AP, India, [email protected] [email protected] Abstract: Aim: Current study designed to identify whether the combination of vitamin C, hydrocortisone, and thiamine, to decrease the mortality and free of vasopressor administration in patients with septic shock. Method: An open-label, randomized Quasi experimental study conducted in 240 cases of sepsis at intensive care unit for the duration of 3 years. Standard care group consists 120 and Interventional consists 120 (Standard care with Hydrocortisone, Vitamin C, and Thiamine). The primary endpoint hospital survival and secondary outcome the duration of vasopressor therapy and other outcomes were measured. Result: Among 240 patients who were randomized, the primary outcome measurement recorded as 3cases (1.25%) in Interventional and 31cases (12.91%) in Standard groups. All patients in the interventional group were weaned off vasopressors with a mean of 17.5±10.2 hrs after starting treatment with the vitaminC+thiamine+hydrocortisone infusion. The mean duration of vasopressor use was 35.8±21.5 h in the standard group (p=0.001); 25% patients in the standard group received higher dose of vasopressors and died due to refractory septic shock. The mean duration of vasopressor treatment is 61.4± 33.8 h in the control patients who died compared with 39.5±12.5h in those who survived. -

Anatomical Classification Guidelines V2021 EPHMRA ANATOMICAL CLASSIFICATION GUIDELINES 2021
EPHMRA ANATOMICAL CLASSIFICATION GUIDELINES 2021 Anatomical Classification Guidelines V2021 "The Anatomical Classification of Pharmaceutical Products has been developed and maintained by the European Pharmaceutical Marketing Research Association (EphMRA) and is therefore the intellectual property of this Association. EphMRA's Classification Committee prepares the guidelines for this classification system and takes care for new entries, changes and improvements in consultation with the product's manufacturer. The contents of the Anatomical Classification of Pharmaceutical Products remain the copyright to EphMRA. Permission for use need not be sought and no fee is required. We would appreciate, however, the acknowledgement of EphMRA Copyright in publications etc. Users of this classification system should keep in mind that Pharmaceutical markets can be segmented according to numerous criteria." © EphMRA 2021 Anatomical Classification Guidelines V2021 CONTENTS PAGE INTRODUCTION A ALIMENTARY TRACT AND METABOLISM 1 B BLOOD AND BLOOD FORMING ORGANS 28 C CARDIOVASCULAR SYSTEM 36 D DERMATOLOGICALS 51 G GENITO-URINARY SYSTEM AND SEX HORMONES 58 H SYSTEMIC HORMONAL PREPARATIONS (EXCLUDING SEX HORMONES) 68 J GENERAL ANTI-INFECTIVES SYSTEMIC 72 K HOSPITAL SOLUTIONS 88 L ANTINEOPLASTIC AND IMMUNOMODULATING AGENTS 96 M MUSCULO-SKELETAL SYSTEM 106 N NERVOUS SYSTEM 111 P PARASITOLOGY 122 R RESPIRATORY SYSTEM 124 S SENSORY ORGANS 136 T DIAGNOSTIC AGENTS 143 V VARIOUS 145 Anatomical Classification Guidelines V2021 INTRODUCTION The Anatomical Classification was initiated in 1971 by EphMRA. It has been developed jointly by Intellus/PBIRG and EphMRA. It is a subjective method of grouping certain pharmaceutical products and does not represent any particular market, as would be the case with any other classification system. -

Vitamin C, Hydrocortisone and Thiamine in Patients with Septic Shock (VITAMINS) Trial: Study Protocol and Statistical Analysis Plan
ORIGINAL ARTICLES Vitamin C, Hydrocortisone and Thiamine in Patients with Septic Shock (VITAMINS) trial: study protocol and statistical analysis plan Tomoko Fujii, Andrew A Udy, Adam M Deane, Nora Luethi, Michael Bailey, Glenn M Eastwood, Daniel Frei, Craig French, Neil Orford, Yahya Shehabi, Paul J Young and Rinaldo Bellomo, on behalf of the VITAMINS trial investigators Sepsis is a dysregulated host response to infection. ABSTRACT Adjunctive therapies targeting the inflammatory cascade are being increasingly explored, although, to date, they Background: Septic shock is associated with poor outcomes. have failed to demonstrate consistent benefit, and sepsis Vitamin C (ascorbic acid) is a cellular antioxidant and has and septic shock continue to lead to poor outcomes. anti-inflammatory properties. Whether the combination Hospital mortality in patients with septic shock remains as therapy of vitamin C, thiamine and hydrocortisone reduces high as 22% in Australia and New Zealand.1 From a global vasopressor dependency in septic shock is unclear. perspective, perhaps 50 million patients with sepsis are Objectives: To describe the protocol and statistical analysis treated in hospitals every year.2 plan of a multicentre, open-label, prospective, phase 2 Moreover, the mortality from sepsis and septic shock in randomised clinical trial evaluating the effects of vitamin middle and low income countries is reported to be as high C, thiamine and hydrocortisone when compared with as 60%.3-5 In addition, patients with sepsis have numerous hydrocortisone monotherapy on the duration of vasopressor short and long term complications and are at increased risk administration in critically ill patients with septic shock. of death for up to several years following the acute event.6-9 Methods: VITAMINS is a multicentre cardiovascular efficacy Thus, effective, low cost and safe treatment strategies are trial in adult patients with septic shock. -
Hyperammonemia.Hyperammonemia
Hyperammonemia.Hyperammonemia. NaeemNaeem AslamAslam.. FellowFellow--20102010 Univ.Univ. ofof Louisville.Louisville. KYKY ContentsContents ofof discussion.discussion. InterestingInteresting Case.Case. CausesCauses ofof highhigh ammoniaammonia (cirrhosis(cirrhosis isis notnot onlyonly cause)cause) MetabolismMetabolism ofof ammonia.ammonia. DiscussionDiscussion aboutabout thethe case.case. CaseCase 3939 yrsyrs oldold AAFAAF withwith h/oh/o GastricGastric bypassbypass (type(type 1)1) surgerysurgery inin 20082008 admittedadmitted forfor reversalreversal ofof bypassbypass surgery.surgery. MultipleMultiple admissionsadmissions inin thethe pastpast forfor excessiveexcessive weightweight loss,loss, weaknessweakness andand peripheralperipheral neuropathiesneuropathies secondarysecondary toto weightweight loss.loss. WeighedWeighed aroundaround >> 400400 poundspounds inin 03/0803/08 WeighedWeighed 225225 poundspounds inin 04/0904/09 PatientPatient waswas diagnoseddiagnosed withwith multiplemultiple vitaminvitamin deficienciesdeficiencies includingincluding B12,B12, copper,copper, ironiron andand thiaminethiamine andand beingbeing supplemented.supplemented. OtherOther issuesissues Anasarca.Anasarca. AnemiaAnemia ofof chronicchronic disease.disease. WeaknessWeakness-- usesuses canecane toto walk.walk. PMHPMH ObesityObesity s/ps/p gastricgastric bypassbypass PreviousPrevious admission.admission. HadHad elevatedelevated LFtsLFts andand foundfound toto havehave elevatedelevated ammoniaammonia level.level. StartedStarted onon LactuloseLactulose -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

Vitamin C, Hydrocortisone and Thiamine for the Treatment of Severe Sepsis and Septic Shock Vitamin C, Hydrocortisone and Thiami
Vitamin C, Hydrocortisone and Thiamine For the treatment of Severe Sepsis and Septic Shock Vitamin C, Hydrocortisone and Thiamine dosing protocol Vitamin C: 1.5 g IV q 6 hourly for 4 days or until discharge from the ICU. Hydrocortisone: 50mg IV push q 6 hourly for 6 days or until discharge from the ICU. Taper is not required. Thiamine: 200mg IV q 12 hourly for 4 days or until discharge from the ICU Vitamin C: Vitamin C is provided by the manufacturer as a 50 ml vial at a concentration of 500mg/ml. Three (3) ml of vitamin C will be placed in a 100ml bag of either dextrose 5% in water (D5W) or normal saline and infused over 60 minutes. Hydrocortisone: Optional dosing strategy: Hydrocortisone 50 mg bolus, followed by a 24-hour continuous infusion of 200 mg for 4 days. Thiamine: Intravenous thiamine (200 mg) was placed in a piggyback in 50 ml of either D5W or normal saline and administered as a 15-minute infusion. 1 | Page Power Calculation: The published hospital mortality for patients with severe sepsis and septic shock in the USA approximates 40%. Based on our previous study and patient modeling we project that the combination of hydrocortisone, vitamin C and thiamine could reduce the mortality to 15%. Assuming a type 1 error of 5% (alpha of 0.05) and a power of 80% (the ability to detect a difference between two groups when a difference exists) would require a sample size of 100 patients. To account for dropouts and other exclusory factors we will therefore aim for a sample size of 140 patients.