CVD: Primary Care Intelligence Packs NHS West Suffolk CCG
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WSC Planning Decisions 24/19
PLANNING AND REGULATORY SERVICES DECISIONS WEEK ENDING 14/06/2019 PLEASE NOTE THE DECISIONS LIST RUN FROM MONDAY TO FRIDAY EACH WEEK DC/19/0852/TCA Tree in a Conservation Area Notification - 1 Walnut Tree Cottage DECISION: no Walnut Tree - Lateral reduction on north Knox Lane No Objections aspect to create 1metre clearance from Bardwell DECISION TYPE: telephone cable IP31 1AX Delegated ISSUED DATED: APPLICANT: Mr Richard Combes 11 Jun 2019 WARD: Bardwell PARISH: Bardwell DC/19/0962/TCA Trees in a Conservation Area Notification - Bardwell Cevc Primary DECISION: 1no.Yew (circled red on plan) - Reduce School No Objections height by up to 3 metres and crown raise School Lane DECISION TYPE: to 2 metres above ground level. Bardwell Delegated IP31 1AD ISSUED DATED: APPLICANT: Ms Sarah Allman 11 Jun 2019 WARD: Bardwell PARISH: Bardwell DC/19/0717/HH Householder Planning Application - (i) Rose Cottage DECISION: Proposed two storey rear extension (ii) Stanton Road Approve Application Proposed single storey side extension Barningham DECISION TYPE: IP31 1BS Delegated APPLICANT: Mr & Mrs R Vansittant ISSUED DATED: 11 Jun 2019 AGENT: Mr David Hart WARD: Barningham PARISH: Barningham DC/19/0802/HH Householder Planning Application - (i) Orchard End DECISION: Replace existing garage roof with a pitched 17 Mill Lane Approve Application tiled roof (ii) render walls to match Barrow DECISION TYPE: approved alteration work Bury St Edmunds Delegated Suffolk ISSUED DATED: APPLICANT: Tina Mc Carthy IP29 5BS 11 Jun 2019 WARD: Barrow AGENT: Mr Mark Cleveland PARISH: Barrow Cum Denham Planning and Regulatory Services, West Suffolk Council, West Suffolk House, Western Way, Bury St Edmunds, Suffolk, IP33 3YU DC/19/1036/TCA Trees in a Conservation Area Application - 29 The Street DECISION: 1no. -

Onward Travel Information Bury St Edmunds Station
Bury St Edmunds Station i Onward Travel Information Buses and Taxis Local area map Bury St Edmunds is a PlusBus area. Contains Ordnance Survey data © Crown copyright and database right 2018 & also map data © OpenStreetMap contributors, CC BY-SA PlusBus is a discount price ‘bus pass’ that you buy with Rail Replacement buses stop at the bus stop on the station forecourt. your train ticket. It gives you unlimited bus travel around your chosen town, on participating buses. Visit www.plusbus.info Main destinations by bus (Data correct at July 2019) DESTINATION BUS ROUTES BUS STOP DESTINATION BUS ROUTES BUS STOP DESTINATION BUS ROUTES BUS STOP Badwell Ash 338 A Chevington 14, 15 Bus Station 8 Stowlangtoft 338 A A A Stradishall Bardwell 304 Fornham All Saints 16, 355 14, 15 Bus Station 8 16, 84, 86, 332, (for HM Prison Highpoint) Barnham 84, 86 A A Fornham St Genevieve Sudbury 753 Bus Station 6 Barningham 338 A 355 16, 84, 86, 304, Thetford 84, 86, 332 A Barrow 312 Bus Station 8 { Fornham St Martin A 332, 338, 355 Walsham-le-Willows 338 A Botesdale 304 A Garboldisham 338 A Wattisfield 304 A Brandon 86 A Great Barton 304, 338 A Westley Village 312 Bus Station 8 10 minutes walk (approx.) from Great Whelnetham 753 Bus Station 6 this Station Wickhambrook 14, 15 Bus Station 8 (see Local area map) Haverhill 14, 15 Bus Station 8 753, "Breeze 1 Hepworth 304, 338 A A { - Bus Station/Town Centre # & Breeze 2" Hoggards Green 753 Bus Station 6 16, 84, 86, 304, Holywell Row 355 A 332, 338, 355, B M44, M55, Honington 332 A 851* Horringer Village 14, 15 Bus Station 8 "Breeze 2", 14, Bus Station 8 (for Ickworth House NT) { - Horringer Court 15, M88 12 Hunston 338 A "Breeze 1", Icklingham 16, 355 A { - Howard Estate M44, M55, A A 851* Ingham 84, 86, 332 "Breeze 1, Ixworth 304, 338 A { - Mildenhall Road Estate M44, M55, A 16 A Kentford 851* 11 C M33 C Lackford 16, 355 A Notes { - Moreton Hall Estate Bus Station 7 384, 385, 854* 10 Lavenham 753 Bus Station 6 { PlusBus destination, please see below for details. -

Babergh District Council Work Completed Since April
WORK COMPLETED SINCE APRIL 2015 BABERGH DISTRICT COUNCIL Exchange Area Locality Served Total Postcodes Fibre Origin Suffolk Electoral SCC Councillor MP Premises Served Division Bildeston Chelsworth Rd Area, Bildeston 336 IP7 7 Ipswich Cosford Jenny Antill James Cartlidge Boxford Serving "Exchange Only Lines" 185 CO10 5 Sudbury Stour Valley James Finch James Cartlidge Bures Church Area, Bures 349 CO8 5 Sudbury Stour Valley James Finch James Cartlidge Clare Stoke Road Area 202 CO10 8 Haverhill Clare Mary Evans James Cartlidge Glemsford Cavendish 300 CO10 8 Sudbury Clare Mary Evans James Cartlidge Hadleigh Serving "Exchange Only Lines" 255 IP7 5 Ipswich Hadleigh Brian Riley James Cartlidge Hadleigh Brett Mill Area, Hadleigh 195 IP7 5 Ipswich Samford Gordon Jones James Cartlidge Hartest Lawshall 291 IP29 4 Bury St Edmunds Melford Richard Kemp James Cartlidge Hartest Hartest 148 IP29 4 Bury St Edmunds Melford Richard Kemp James Cartlidge Hintlesham Serving "Exchange Only Lines" 136 IP8 3 Ipswich Belstead Brook David Busby James Cartlidge Nayland High Road Area, Nayland 228 CO6 4 Colchester Stour Valley James Finch James Cartlidge Nayland Maple Way Area, Nayland 151 CO6 4 Colchester Stour Valley James Finch James Cartlidge Nayland Church St Area, Nayland Road 408 CO6 4 Colchester Stour Valley James Finch James Cartlidge Nayland Bear St Area, Nayland 201 CO6 4 Colchester Stour Valley James Finch James Cartlidge Nayland Serving "Exchange Only Lines" 271 CO6 4 Colchester Stour Valley James Finch James Cartlidge Shotley Shotley Gate 201 IP9 1 Ipswich -

Marks Farm Wickhambrook, Suffolk Marks Farm, Farley Green, Wickhambrook, Suffolk CB8 8PY
Marks Farm Wickhambrook, Suffolk Marks Farm, Farley Green, Wickhambrook, Suffolk CB8 8PY Wickhambrook is a lovely rural village with a vibrant community served by a Public House, shop, school, surgery and parish Church, closely linked to the A143 which provides fast access to the Cathedral town of Bury St Edmunds, approximately 11 miles, in turn providing access to the A14 trunk road to London via the M11. Newmarket (home to British Horseracing) is approximately 7 miles, Cambridge 20 miles and Stansted Airport is approximately 40 minutes. This unique detached property is situated in a quiet rural location enjoying stunning views over open countryside. The property which offers the potential for further enlargement (subject to the necessary planning consents) sits within mature gardens, affording ample parking with a double cart lodge, stable block and pony paddock. In all about 0.43 of an acre. A unique detached property set within 0.43 of an acre with a cart lodge, stables and small paddock. ENTRANCE into: ENTRANCE LOBBY with coat rails and doors leading to the boot room BEDROOM Enjoying views over open countryside and a double and utility room. wardrobe. SITTING ROOM A charming spacious room enjoying a pleasant outlook to BEDROOM Also with a double wardrobe whilst enjoying a double aspect the front and wood burning stove. outlook. First Floor KITCHEN/BREAKFAST ROOM The hub of the home, tastefully fitted with a range of units under wooden worktops with a Belfast sink inset. MASTER BEDROOM An impressive double bedroom with a storage Appliances include a double oven range cooker with six ring hob and hood, cupboard and far-reaching views over open countryside. -
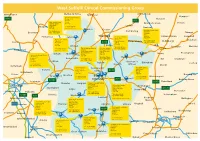
West Suffolk Commiss Map V5
West Suffolk Clinical Commissioning Group Welney Wimblington Methwold Hythe Mundford Attleborough Hempnall Brandon Medical Practice A141 31 High Street Bunwell Brandon A11 Lakenheath Surgery Suffolk 135 High Street IP27 0AQ New Buckenham Shelton Lakenheath Larling Littleport Suffolk Tel: 01842 810388 Fax: 01842 815750 Banham IP27 9EP Brandon Croxton Botesdale Health Centre Tel: 01842 860400 East Harling Back Hills Downham Fax: 01842 862078 Botesdale Alburgh Diss Prickwillow Lakenheath Thetford Dr Hassan & Partners Norfolk Pulham St Mary Redenhall 10 The Chase IP22 1DW Market Cross Surgery Stanton Mendham Ely 7 Market Place Bury St Edmunds Garboldisham Tel: 01379 898295 Dickleburgh Sutton Mildenhall A134 Suffolk Fax: 01379 890477 Suffolk IP31 2XA IP28 7EG Eriswell Euston Diss Tel: 01359 251060 Brockdish Metfield Tel: 01638 713109 The Guildhall and Barrow The Swan Surgery Fax: 01359 252328 Scole Haddenham Fax: 01638 718615 Surgery Northgate Street Lower Baxter Street Bury St Edmunds Bury St Edmunds Suffolk Botesdale Fressingfield Isleham Mildenhall Suffolk IP33 1AE Brome The Rookery Medical Centre IP33 1ET The Rookery Tel: 01284 770440 Stanton Newmarket Barton Mills Tel: 01284 701601 Fax: 01284 723565 Eye Stradbroke Suffolk Fax: 01284 702943 CB8 8NW Wicken Fordham Walsham le Ingham Gislingham Laxfield Tel: 01638 665711 Ixworth Willows Occold Cottenham Fax: 01638 561280 Victoria Surgery Fornham All The Health Centre Burwell Victoria Street Heath Road Bury St Edmunds Saints A143 Woolpit Waterbeach Suffolk SuffolkBacton IP33 3BB IP30 9QU Histon -

Discover Suffolk Wickhambrook Walks
2 1 5 0 0 1 - E S E - 4 1 8 0 0 6 0 6 2 3 7 4 1 0 H u 0 2 P i t n i r P & n g i s e D y b d e t n i r P . s n g i s l a c o l d n a e c i v d a w o l l o F . d e r a p e r p e b d n a d a e h a n a l P . l o r t n o c e v i t c e f f e r e d n u s g o d p e e k . e m o h r e t t i l r u o y e k a t d n a t i s i v r u o y f o e c a r t o n e v a e L . l i c n u o C y t n u o C k l o f f u S . e l b a l i a v a s i s s e c c a r e d i w s s e l n u s h t a p w o l l o f d n a d n a l i c n u o C h s i r a P k o o r b m a h k c i W y b d e c u d o r P m e h t d n i f d l u o w u o y s a y t r e p o r p d n a s e t a g e v a e L . -

Suffolk Record Office New Accessions 1 Jan 2012-31 Dec 2012
SUFFOLK RECORD OFFICE NEW ACCESSIONS 1 JAN 2012-31 DEC 2012 Bury branch SCALTBACK MIDDLE SCHOOL, NEWMARKET: Headmaster of Scaltback School, J. D Eastham's desk diaries 1976-1990; 14, A5 volumes; 22 colour photocopy images of school; colour photos of school; 1st Prospectus; Postcard for school; 4 maps/plans of school site (copies):annotated and labelled 'landscaping', relating to intruder alarm areas, 'copy of original site plan, 12.70 acres' with covering letter and photocopy of the original conveyance attached, showing schools in Newmarket near Scaltback Middle School; DVD of Scaltback Middle School 1972-2012; 41 assorted certificates for fundraising and music festival entries with associated correspondence (1972-2011); press cuttings re School (1970s and 1980s ADB523 ROUGHAM PRIMARY SCHOOL: Admission Register 1971-2001 ADB716 TOSTOCK PARISH COUNCIL: folder of Parish Council minutes 2006-2009 EG503 GREAT CORNARD TOWN LAND CHARITY: Financial Statement for year ending 18th Jan 2012 EG532 DRINKSTONE PARISH COUNCIL: Minutes 1968-2003 ¶Annual Parish Meeting Minutes 1952-2001 EG534 SUDBURY TOWN COUNCIL: Sudbury Borough Council Account Book, 1930-1931; Petty accounts book, nd; Sudbury Borough Council Minutes, 1955-1957; Indexed account book, 1897-1904; Finance and General Purposes Committee, 1943-1946; Copy letter book (fragile) nd; Indexed copy letter book, nd; Sudbury Burial Board book accounting workmen's names, labour and wages, 1888; Sudbury and Ballingdon Burial Board Labour Account, 1892-1907 EG574 ELMSETT PARISH: 4 marriage registers: 1961-1996; Baptism Register 1887-2010 FB61 WISSINGTON PARISH: Banns Book 1824-2010 FB65 POLSTEAD PARISH: Burial register 1876-1981 FB78 WICKHAMBROOK UNITED REFORMED CHURCH: Congregationalism in Wickhambrook, Suffolk' by Oswald Henry Coleman 1844; Order of Service, 1937; 2 (presumably copy) photos, one of a horse and trap, one of a car, both with passengers. -

Baxter House, Meadow View, Thorns Corner, Wickhambrook, Suffolk, Cb8 8Xw
BAXTER HOUSE, MEADOW VIEW, THORNS CORNER, WICKHAMBROOK, SUFFOLK, CB8 8XW FINISHED TO A HIGH SPECI FICATION. This spacious new home offers 1292 sq ft of living accommodation and is situated in a quiet tucked away location in a popular Suffolk Village. The property offers a flexible layout and enjoys fine views over open countryside with a cartlodge garage and parking. Guide £285,000 Baxter House, Meadow View, Thor ns Corner, Accommodation Wickhambrook, Newmarket, Suffolk, CB8 8XW Second Floor Master Bedroom with En Suite Wickhambrook is a lovely rural village served by Public House, 3 Further Bedrooms Garden shop and parish Church. Closely linked to the A143 which provides Sitting/Dining Room Parking fast access to the Cathedral town of Bury St Edmunds , Kitchen Cartlodge approximately 10 miles, in turn providing access to the A14 trunk Cloakroom road to London via the M11. Newmarket (home to British Horseracing) is approximately 7 miles and Cambridge 20 miles. Family Bathroom Features Specification • Individually architect-designed homes. • Double glazed timber windows and French doors. • Exclusive development backing onto countryside. • Classic kitchen with ceramic sink and solid oak worktops. • High specification blended with traditional materials. • • Walking distance of village store, public house, village hall Integrated oven, 4 ring hob and hood. and primary school. • Ceramic tiled flooring in wet areas. • Quiet, tucked away position. • White contemporary sanitary ware to cloakrooms • 10 year NHBC warranty. and bathrooms. • Ample TV, satellite, telephone and power points. Additional information and viewing Cambridge and County Developments approaches each development individually, tailoring its specification and design Services: Main water, electricity and drainage. -

Accessions 1 October 1999 – 30 September 2000
ACCESSIONS 1 OCTOBER 1999 – 30 SEPTEMBER 2000 BURY ST EDMUNDS BRANCH OFFICIAL Lakenheath and Brandon Great Fen Drainage Board: minutes 1924-1946 (EK502) Sudbury Poor Law Union: Guardians’ minutes 1895-1927 (ADA501) LOCAL PUBLIC Jane Walker Hospital, Nayland: East Anglian Sanatorium Company Ltd: minutes, accounts, photographs, films, correspondence and papers 1900-(1988) (ID507) Walnuttree Hospital, Sudbury Sudbury Union Workhouse/Sudbury Poor Law Institution/Walnut Tree Hospital: male ward report books 1934-1939, female ward report books 1934-1939; ward diet books 1935-1939; admission and discharge register 1970-1979; miscellaneous volumes and papers 1937-1973 (ID502) SCHOOLS Great Barton VCP School: Millennium time capsule details 2000 (ADB731) Bury St Edmunds, County Grammar School for Girls: school magazines 1956-1959; photocopy of form photograph (1957) (HD2349) Bury St Edmunds, St Alban’s Catholic First School: photographs and miscellaneous material late 20th cent. (ADB732) Risby CEVCP School: admission register 1943-1993; log book 1989-1998; governors’ minutes and related papers 1988-1999; photographs 1971-1999; certificates 1969-c1971 (ADB524) Great Whelnetham VCP School: log books 1980-1999; punishment book 1907-1936; Friends’ minutes 1979-1982 (ADB526) CIVIL PARISH Haverhill Town Council: council/committee minutes 1989-1998; correspondence and papers relating to setting up the council in 1989 (EG714) Kedington: minutes 1978-1991 (EG546) Rattlesden: minutes 1894-1975; declarations on acceptance of office 1926-1962; Burial Board -

West Suffolk PCN Groupings
West Suffolk PCN Groupings Bury St Edmunds PCN Clinical Director: Mark Hunter Pharmacy Lead: GP Practices Pharmacies Angel Hill Abbey / Guildhall Pharmacy Guildhall Asda Pharmacy, Western Way Mount Farm Barrow Pharmacy Victoria Boots Pharmacy, Cornhill Swan Croasdale & Sons Pharmacy Croasdale Chemist, Mountpharm Day Lewis Pharmacy, St Olaves Lloyds in Sainsburys Pharmacy, Bedingfield Way Lloyds Pharmacy, Victoria Street Superdrug Stores Plc Pharmacy, Cornhill Swan Pharmacy Tesco Instore Pharmacy, St Saviours Thurston Pharmacy Haverhill PCN Clinical Director: Firas Watfeh Pharmacy Lead: GP Practices Pharmacies Clements Boots Pharmacy, High Street Haverhill Family Practice David Holland Pharmacy Haverhill Pharmacy, Camps Rd Lloyds in Sainsburys Pharmacy, Haycocks Rd Tesco Instore Pharmacy, Cangle Rd Well Pharmacy, Mill Rd WGGL PCN Clinical Director: Christopher Browning Pharmacy Lead: GP Practices Pharmacies Guildhall- Clare Clare Pharmacy Long Melford Glemsford Pharmacy Glemsford Lavenham Pharmacy Wickhambrook The Pharmacy, Long Melford Sudbury GP PCN Clinical Director: Bob Morgan/ Bahram Pharmacy Lead: Talebpour GP Practices Pharmacies Hardwick House Boots Pharmacy, Market Hill Siam Boots Pharmacy, Great Cornard Lloyds in Sainsburys Pharmacy, Cornard Road Lloyds Pharmacy, North St Parade Pharmacy Superdrug Pharmacy, North St Tesco Instore Pharmacy, Springlands Way West Suffolk PCN Groupings Forest Heath PCN Clinical Director: Lee Bower/Nick Rayner Pharmacy Lead: GP Practices Pharmacies Orchard House Boots Pharmacy, Bury Rd, Brandon Rookery Boots Pharmacy, High Street, Brandon Oakfield Boots Pharmacy, High St, Newmarket BMP Day Lewis Pharmacy, Red Lodge Reynard Lakenheath Pharmacy Market Cross Lloyds Pharmacy, Market Place, Mildenhall Lakenheath Lloyds Pharmacy, Manor Court, Mildenhall Forest Surgery Lords Pharmacy Newmarket Superdrug Pharmacy, Newmarket Tesco Stores Ltd Pharmacy, Newmarket Blackbourne Rural PCN Clinical Director: Richard West/Jude Pharmacy Lead: Chapman GP Practices Pharmacies Stanton Station Pharmacy Botesdale Woolpit Pharmacy Woolpit . -

Wickhambrook Parish Council Minutes
Page | 10486 Wickhambrook Parish Council Minutes Of an ordinary meeting of the Council held on Thursday 25th April 2019 Present: Cllrs J Barton, J Claydon, P Couzens, M Jolland, K Merritt, J Midwood, J Wilson Attending: Parish Clerk Hilary Workman Cllr Mary Evans (Suffolk County Council) 19.04.01 Noted: Apologies for absence were received from Cllr Sammons. Apologies had been received from District Councillor Clive Pollington. 19.04.02 Noted: Cllr Wilson declared a Disclosable Pecuniary Interest with reference to items 10.2.6; and 10.4.5. There were no other Members’ Declarations of Local Non-Pecuniary Interest or Disclosable Pecuniary Interest. There were no additions and/or deletions to the Council’s Register of Interests. 19.04.03 Resolved: That the Minutes of the Parish Council meeting held on 28th March, 2019, as tabled, were agreed as a true record. 19.04.04 Noted: Correspondence to this meeting not dealt with as an Agenda item or in the Clerk’s report. 4.1 SALC updates (circulated) & Great British Spring Clean 4.2 Suffolk County Council – Proposed cutting schedule (circulated) 4.3 West Suffolk Council 4.3.1 Completion of Register of Members’ Interests Form (circulated at meeting) 4.3.2 Planning Department Newsletter & Guidance Notes (circulated) 4.4 Healthwatch Suffolk – articles for website – the meeting asked the Clerk to arrange for these articles to be published on the Parish Website 4.5 Tempest Notice Boards 4.6 Explore4more – First Aid Training – the meeting asked the Clerk to include this on the May Agenda 19.04.05 Open Session: 7:35pm Noted: That when public comment or question on any Agenda item was invited, there was none. -

WSC Planning Decisions 51/19
PLANNING AND REGULATORY SERVICES DECISIONS WEEK ENDING 20/12/2019 PLEASE NOTE THE DECISIONS LIST RUN FROM MONDAY TO FRIDAY EACH WEEK DC/19/2229/TCA Trees in a Conservation Area Notification - Croft House DECISION: (i) mixed species (Front Boundary A-B on The Green No Objections plan) - reduce in height to measurements Bardwell DECISION TYPE: shown in attached survey (ii) 1no. Willow IP31 1AW Delegated (FL1 on plan) reduce height to 5 metres ISSUED DATED: (iii) mixed species (Front Boundary C-D on 18 Dec 2019 plan) reduce height of mixed hedge to 3 WARD: Bardwell metres (iv) 1no. apple (BL1 on plan) PARISH: Bardwell reduce in height to 5 metres with a 4 metre spread (v) 1no. Beech (BL2 on plan) prune overhanging branches to boundary line (vi) 1no. Pine (BL3 on plan) crown raise to 7 metres above ground level (vii) 1no. Maple (BL4 on plan) reduce to 7 metres in height (viii) mixed species (Back Boundary E-F) reduce to 3 metres from ground level (ix) 1no. Horse Chestnut (BR1 on plan) Thin crown by 15% and (x) 1no. Yew (BR2 on plan) Prune overhanging branches to boundary line. APPLICANT: Mrs Jacqueline Burns DC/19/2247/TCA Trees in a Conservation Area Notification - 1 Chalet Cottages DECISION: 2no. (i) Yew (T001 on plan) crown Church Road No Objections reduction of 2 metres to south/south Bardwell DECISION TYPE: eastern aspect and crown lift to 3 metres Bury St Edmunds Delegated (ii) (T004 on plan) raise branches to 4 Suffolk ISSUED DATED: metres over outbuildings IP31 1AH 18 Dec 2019 WARD: Bardwell APPLICANT: Mr G McMeechan PARISH: Bardwell