Urine Drug Screening
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fact Sheet on Methadone
Fact Sheet: Methadone Common Questions about Methadone • What is the typical dose of methadone and how is it taken? • How does someone know methadone is working? • How long does a person take methadone? • Who can prescribe methadone? • Can a person overdose on methadone? What is the typical dose of methadone and how is it taken? • Due to methadone’s slow and steady activation of opioid receptors, a person requires only one methadone dose per day. • Every person is different, and dosing should be individualized, based on a person’s experience of a reduction of withdrawal symptoms and cravings. • Most people start with an initial dose of 30-35 mg. It is then increased by 5mg every 3 days until a person experiences a relief from withdrawal symptoms.1 • Methadone is taken by mouth in a liquid form. • The recommended therapeutic (i.e., effective) dose of methadone is between 60 and 120 mg.1 How does someone know methadone is working? • The person will stop feeling withdrawal symptoms. • The person will also experience fewer cravings to use opioids. The intensity of their cravings will go down, but they may not completely go away.1 o Someone taking methadone may still have cravings to use other substances such as cocaine, benzodiazepines, alcohol, etc. The 3 Dimensions of Cravings: Frequency Duration Severity Number of separate times Once a craving starts, it Cravings range in a person starts to can range in how long it intensity, such as how experience a craving lasts at a high, distracting overwhelming, distracting, during the day. level. This could be and painful they feel. -

Medical Review Officer Manual
Department of Health and Human Services Substance Abuse and Mental Health Services Administration Center for Substance Abuse Prevention Medical Review Officer Manual for Federal Agency Workplace Drug Testing Programs EFFECTIVE OCTOBER 1, 2010 Note: This manual applies to Federal agency drug testing programs that come under Executive Order 12564 dated September 15, 1986, section 503 of Public Law 100-71, 5 U.S.C. section 7301 note dated July 11, 1987, and the Department of Health and Human Services Mandatory Guidelines for Federal Workplace Drug Testing Programs (73 FR 71858) dated November 25, 2008 (effective October 1, 2010). This manual does not apply to specimens submitted for testing under U.S. Department of Transportation (DOT) Procedures for Transportation Workplace Drug and Alcohol Testing Programs (49 CFR Part 40). The current version of this manual and other information including MRO Case Studies are available on the Drug Testing page under Medical Review Officer (MRO) Resources on the SAMHSA website: http://www.workplace.samhsa.gov Previous Versions of this Manual are Obsolete 3 Table of Contents Chapter 1. The Medical Review Officer (MRO)........................................................................... 6 Chapter 2. The Federal Drug Testing Custody and Control Form ................................................ 7 Chapter 3. Urine Drug Testing ...................................................................................................... 9 A. Federal Workplace Drug Testing Overview.................................................................. -

Methadone Hydrochloride Tablets, USP) 5 Mg, 10 Mg Rx Only
ROXANE LABORATORIES, INC. Columbus, OH 43216 DOLOPHINE® HYDROCHLORIDE CII (Methadone Hydrochloride Tablets, USP) 5 mg, 10 mg Rx Only Deaths, cardiac and respiratory, have been reported during initiation and conversion of pain patients to methadone treatment from treatment with other opioid agonists. It is critical to understand the pharmacokinetics of methadone when converting patients from other opioids (see DOSAGE AND ADMINISTRATION). Particular vigilance is necessary during treatment initiation, during conversion from one opioid to another, and during dose titration. Respiratory depression is the chief hazard associated with methadone hydrochloride administration. Methadone's peak respiratory depressant effects typically occur later, and persist longer than its peak analgesic effects, particularly in the early dosing period. These characteristics can contribute to cases of iatrogenic overdose, particularly during treatment initiation and dose titration. In addition, cases of QT interval prolongation and serious arrhythmia (torsades de pointes) have been observed during treatment with methadone. Most cases involve patients being treated for pain with large, multiple daily doses of methadone, although cases have been reported in patients receiving doses commonly used for maintenance treatment of opioid addiction. Methadone treatment for analgesic therapy in patients with acute or chronic pain should only be initiated if the potential analgesic or palliative care benefit of treatment with methadone is considered and outweighs the risks. Conditions For Distribution And Use Of Methadone Products For The Treatment Of Opioid Addiction Code of Federal Regulations, Title 42, Sec 8 Methadone products when used for the treatment of opioid addiction in detoxification or maintenance programs, shall be dispensed only by opioid treatment programs (and agencies, practitioners or institutions by formal agreement with the program sponsor) certified by the Substance Abuse and Mental Health Services Administration and approved by the designated state authority. -

Opioid Powders Page: 1 of 9
Federal Employee Program® 1310 G Street, N.W. Washington, D.C. 20005 202.942.1000 Fax 202.942.1125 5.70.64 Section: Prescription Drugs Effective Date: April 1, 2020 Subsection: Analgesics and Anesthetics Original Policy Date: October 20, 2017 Subject: Opioid Powders Page: 1 of 9 Last Review Date: March 13, 2020 Opioid Powders Description Buprenorphine Powder, Butorphanol Powder, Codeine Powder, Hydrocodone Powder, Hydromorphone Powder, Levorphanol Powder, Meperidine Powder, Methadone Powder, Morphine Powder, Oxycodone Powder, Oxymorphone Powder Background Pharmacy compounding is an ancient practice in which pharmacists combine, mix or alter ingredients to create unique medications that meet specific needs of individual patients. Some examples of the need for compounding products would be: the dosage formulation must be changed to allow a person with dysphagia (trouble swallowing) to have a liquid formulation of a commercially available tablet only product, or to obtain the exact strength needed of the active ingredient, to avoid ingredients that a particular patient has an allergy to, or simply to add flavoring to medication to make it more palatable. Buprenorphine, butorphanol, codeine, hydrocodone, hydromorphone, levorphanol, meperidine, methadone, morphine, oxycodone, and oxymorphone powders are opioid drugs that are used for pain control. The intent of the criteria is to provide coverage consistent with product labeling, FDA guidance, standards of medical practice, evidence-based drug information, and/or published guidelines. Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, and because of the greater risks of overdose and death (1-15). Regulatory Status 5.70.64 Section: Prescription Drugs Effective Date: April 1, 2020 Subsection: Analgesics and Anesthetics Original Policy Date: October 20, 2017 Subject: Opioid Powders Page: 2 of 9 FDA-approved indications: 1. -
Quantitative Drug Test Menu Section 2
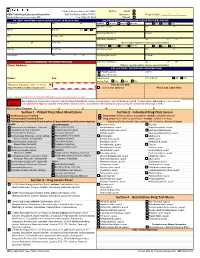
1 Guthrie Square, Sayre, PA 18840 Bill To: Client GMG Toxicology Laboratory Requisition Toll Free Phone (844) 617-4719 Insurance Request Date: _____/______/______ Medical Director: Hani Hojjati, MD Fax (570) 887-4729 Patient PATIENT INFORMATION (PLEASE PRINT IN BLACK INK) INSURANCE BILLING INFORMATION (PLEASE PRINT IN BLACK INK) Pt Last Name First M I PRIMARY Medicare Medicaid Other Ins. Self Spouse Child __ Subscriber Last Name First M Address Birth Date Sex M F Beneficiary/Member # Group # City Pt. SS# or MRN Claims Name and Address City ST ZIP ST ZIP Home Phone (Attach a copy of the patient's insurance card and information) SECONDARY Medicare Medicaid Other Ins. Self Spouse Child Employer Work Phone Subscriber Last Name First M Work Address City ST ZIP Beneficiary/Member # Group # __ CLIENT INFORMATION - REFERRING PHYSICIAN Claims Name and Address City ST ZIP Client Address: (Atttach a copy of the patient's insurance card and information) COLLECTION / REPORTING INFORMATION Copy to: FAX Results to __ CALL Results to Phone: Fax: Date Collected: Time Collected: AM PM Specimen Type: Urine Saliva Other ___________________ Physician Signature (legible - No Stamp) For Lab Use Only (Required for Medicare & Medicaid patient orders) Signed ABN Obtained Place Lab Label Here Contact Laboratory Medical Director (570-887-4719) with questions concerning medical necessity PHYSICIAN When ordering tests, the physician is required to make an independent medical necessity decision with regard to each test thelaboratory will bill. The physician also understands he or she is required NOTICE to (1) submit ICD-10 diagnosis supported in the patient's medical record as documentation of the medical necessity or (2) explain and have the patient sign an ABN. -

Guidelines for Ketamine Use
St Joseph's Mercy Hospice Auckland NZ Guidelines for Ketamine Use Ketamine is a dissociative anaesthetic agent which has analgesic properties in sub- anaesthetic doses 1 Its principal site of action is in the dorsal horn of the spinal cord where it blocks the N-methyl D-aspartate (NMDA) receptor complex. Ketamine is used in palliative care settings primarily for neuropathic pain which is unresponsive or poorly responsive to first-line analgesics (which may include one or more of opioid drug, NSAID, tricyclic antidepressant, or anticonvusant) It has also been used for phantom limb and ischaemic pain and for intractable incident pain or prior to procedures such as dressing changes. Potential side effects Ketamine Routine use of ketamine is limited by its cost and potential side effects which may occur in up to 40% of patients; These may include: Psychotomimetic phenomena – “feeling strange” - dysphoria, vivid dreams, nightmares, hallucinations, altered body image. These effects may be minimised or treated by concurrent use of haloperidol or a benzodiazepine Delirium Hypertension, tachycardia Diplopia, nystagmus Erythema and pain at injection site Contraindications to ketamine use Ketamine has the potential to increase intra-cranial and intra-ocular pressures. It is contraindicated in patients with a history of hypertension, cerebrovascular disease or epilepsy and should be used with caution in patients with raised intra-cranial pressure and/or known cerebral metastases. Dosage regimens for Ketamine use 1. “Burst ketamine” 2 Ketamine is prescribed as a ‘burst’or ‘pulse’ course for a maximum of 5 days. The dose is titrated up, in a stepwise fashion, and once the lowest effective dose is achieved it is continued for 3 days at that dose then stopped. -

Substance Abuse in the Workplace Policy
Substance Abuse in the Workplace Policy Rexnord (herein referred to as “Rexnord” or the “Company”) has a strong commitment to its employees to provide a safe work environment and to promote high standards of employee performance. Consistent with the spirit and intent of this commitment, the Company has established a policy regarding substance abuse in the workplace. Further, the Company is committed to maintaining a drug-free workplace as required by “The Drug-Free Workplace Act of 1988.” Therefore, compliance with this Policy is a condition of continued employment with Rexnord. I. PURPOSE To outline the procedures to be followed by each location in order to ensure that the safety and performance of employees is not impaired by alcohol, illegal drugs or other substances. II. APPLICABILITY This policy shall apply to all employees (full-time, part-time, exempt, and non-exempt employees) as well as to all applicants who have received a conditional offer of employment. Personnel who perform their services on Company property or on a third party’s property at the request of the Company (e.g., a Company customer site), as provided under a contract either directly with the Company or through the services of an outside firm, are required to abide by this policy. It is the responsibility of the contracting firm (at its cost and expense) to ensure that its personnel are tested in conformance with this policy prior to working at / on behalf of Rexnord. III. SUBSTANCE ABUSE It is the Company’s policy that the following is prohibited and will result in discipline up to and including termination: A. -

Methadone and the Anti-Medication Bias in Addiction Treatment
White, W. & Coon, B. (2003). Methadone and the anti-medication bias in addiction treatment. Counselor 4(5): 58-63. Methadone and the Anti-medication Bias in Addiction Treatment William L. White, MA and Brian F. Coon, MA, CADC An Introductory Note: This article is long overdue. Like many addiction counselors personally and professionally rooted in the therapeutic community and Minnesota model programs of the 1960s and 1970s, I exhibited a rabid animosity toward methadone and protected these beliefs in a shell of blissful ignorance. That began to change in the late 1970s when a new mentor, Dr. Ed Senay, gently suggested that the great passion I expressed on the subject of methadone seemed to be in inverse proportion to my knowledge about methadone. I hope this article will serve as a form of amends for that ignorance and arrogance. (WLW) There is a deeply entrenched anti-medication bias within the field of addiction treatment. This bias is historically rooted in the iatrogenic insults that have resulted from attempts to treat drug addiction with drugs. The most notorious of these professional practices includes: coaching alcoholics to substitute wine and beer for distilled spirits, treating alcoholism and morphine addiction with cocaine and cannabis, switching alcoholics from alcohol to morphine, failing repeatedly to find an alcoholism vaccine, employing aversive agents that linked alcohol or morphine to the experience of suffocation and treating alcoholism with drugs that later emerged as problems in their own right, e.g., barbiturates, amphetamines, tranquilizers, and LSD. A history of harm done in the name of good culturally and professionally imbedded a deep distrust of drugs in the treatment of alcohol and other drug addiction (White, 1998). -

Hydromorphone
Hydromorphone WHAT IS HYDROMORPHONE? sedation, and reduced anxiety. It may also cause Hydromorphone belongs to a class of drugs mental clouding, changes in mood, nervousness, called “opioids,” which includes morphine. It and restlessness. It works centrally (in the has an analgesic potency of two to eight times brain) to reduce pain and suppress cough. greater than that of morphine and has a rapid Hydromorphone use is associated with both onset of action. physiological and psychological dependence. WHAT IS ITS ORIGIN? What is its effect on the body? Hydromorphone is legally manufactured and Hydromorphone may cause: distributed in the United States. However, • Constipation, pupillary constriction, urinary retention, users can obtain hydromorphone from nausea, vomiting, respiratory depression, dizziness, forged prescriptions, “doctor-shopping,” impaired coordination, loss of appetite, rash, slow or theft from pharmacies, and from friends and rapid heartbeat, and changes in blood pressure acquaintances. What are its overdose effects? What are the street names? Acute overdose of hydromorphone can produce: Common street names include: Severe respiratory depression, drowsiness • D, Dillies, Dust, Footballs, Juice, and Smack progressing to stupor or coma, lack of skeletal muscle tone, cold and clammy skin, constricted What does it look like? pupils, and reduction in blood pressure and heart Hydromorphone comes in: rate • Tablets, capsules, oral solutions, and injectable Severe overdose may result in death due to formulations respiratory depression. How is it abused? Which drugs cause similar effects? Users may abuse hydromorphone tablets by Drugs that have similar effects include: ingesting them. Injectable solutions, as well as • Heroin, morphine, hydrocodone, fentanyl, and tablets that have been crushed and dissolved oxycodone in a solution may be injected as a substitute for heroin. -

Recommended Methods for the Identification and Analysis of Fentanyl and Its Analogues in Biological Specimens
Recommended methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Recommended Methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES UNITED NATIONS Vienna, 2017 Note Operating and experimental conditions are reproduced from the original reference materials, including unpublished methods, validated and used in selected national laboratories as per the list of references. A number of alternative conditions and substitution of named commercial products may provide comparable results in many cases. However, any modification has to be validated before it is integrated into laboratory routines. ST/NAR/53 Original language: English © United Nations, November 2017. All rights reserved. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. Mention of names of firms and commercial products does not imply the endorse- ment of the United Nations. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. Acknowledgements The Laboratory and Scientific Section of the UNODC (LSS, headed by Dr. Justice Tettey) wishes to express its appreciation and thanks to Dr. Barry Logan, Center for Forensic Science Research and Education, at the Fredric Rieders Family Founda- tion and NMS Labs, United States; Amanda L.A. -
Drug & Alcohol Testing Be a Driver in the Know
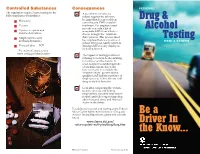
Controlled Substances Consequences FEDERAL The regulations require 5-panel testing for the 3 A positive test result or a following classes of substances: refusal requires the driver to be immediately removed from Drug & Marijuana n operating any CMV on public n Cocaine roadways. The employer must provide you with a list of Alcohol n Opiates — opium and acceptable SAPs from which to codeine derivatives choose to begin the “return-to- ” n Amphetamines and duty process. This process must Testing meth amphetamines be completed before a positive or REGULATIONS refusal driver can legally return to n Phencyclidine — PCP driving CMVs for any employer, including himself. For more information, visit www.usdoj.gov/dea/concern 3 The impact of testing positive or refusing to test can be devastating for a driver and his family. It often results in extended periods of unemployment, due to the time necessary to complete the “return-to-duty” process with a qualified SAP and the tendency of employers not to hire drivers with drug or alcohol histories. 3 Even after completing the “return- to-duty” process and finding employment, the additional return- to-duty and follow-up testing often adds increased stress and financial strain on the driver. For additional research and reading on the Federal Motor Carrier Safety Administration’s Drug and Be a Alcohol Testing Regulations, please visit our web site at: www.fmcsa.dot.gov/ Driver In rules-regulations/topics/drug/drug.htm the Know... FMCSA-E-06-003 Revised July 2010 The U.S. Department of Transportation (DOT) whenever they are involved in a fatal accident, or professional (SAP) drug and alcohol testing regulations for receive a traffic citation resulting from an injury or who signs the return- commercial driver licensed (CDL) employees are vehicle-disabling accident. -

Pre - PA Allowance Age 12 Years of Age Or Older – Ultracet (Tramadol and Acetaminophen) and Codeine/APAP Products
OPIOID IR COMBO DRUGS Apadaz* (benzhydrocodone-acetaminophen), Codeine-acetaminophen, Dvorah* (dihydrocodeine-caffeine-acetaminophen*), Hydrocodone-acetaminophen, Hydrocodone- acetaminophen solution 10-325mg*, Hydrocodone-ibuprofen, Nalocet* (oxycodone- acetaminophen*), Oxycodone-acetaminophen, Oxycodone-aspirin, Oxycodone-ibuprofen, Primlev*/Prolate* (oxycodone-acetaminophen*), Tramadol-acetaminophen, Trezix (dihydrocodeine-caffeine-acetaminophen) *Prior authorization for certain non-covered formulations applies only to formulary exceptions Pre - PA Allowance Age 12 years of age or older – Ultracet (tramadol and acetaminophen) and Codeine/APAP products Quantity Patients 18 years or older will be able to fill the Pre-PA Allowance after they have filled an initial 7 day supply of IR opioid therapy or if they have been on IR or ER opioid therapy in the last 180 days Patients age 17 and under will require a PA after they have filled a 3 day supply of the Pre- PA Allowance Patients with opioid addiction treatment or methadone in the last 30 days will not be eligible for Pre-PA Allowance Immediate Release Tablets or Capsules ≤ 50 MME/day Medication Strength Quantity Limit Codeine/APAP soln 120-12 mg/5 mL Hydrocodone/APAP soln 7.5/325 mg/15 mL 5400 mL per 90 days Hydrocodone/APAP elixir 10/300 mg/15 mL Oxycodone/APAP soln 5-325 mg/5 mL 3000 mL per 90 days Hydrocodone/ibuprofen 5/200 mg, 7.5/200 mg, 10/200 mg 270 units per 90 days Oxycodone/ibuprofen 5/400 mg Oxycodone/APAP 10/325 mg Codeine/APAP 60/300 mg Hydrocodone/APAP 7.5/300 mg, 7.5/325