Up-Regulation of Heme Oxygenase-1 Expression and Inhibition of Disease-Associated Features by Cannabidiol in Vascular Smooth Muscle Cells
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antioxidants and Second Messengers of Free Radicals
antioxidants Antioxidants and Second Messengers of Free Radicals Edited by Neven Zarkovic Printed Edition of the Special Issue Published in Antioxidants www.mdpi.com/journal/antioxidants Antioxidants and Second Messengers of Free Radicals Antioxidants and Second Messengers of Free Radicals Special Issue Editor Neven Zarkovic MDPI • Basel • Beijing • Wuhan • Barcelona • Belgrade Special Issue Editor Neven Zarkovic Rudjer Boskovic Institute Croatia Editorial Office MDPI St. Alban-Anlage 66 4052 Basel, Switzerland This is a reprint of articles from the Special Issue published online in the open access journal Antioxidants (ISSN 2076-3921) from 2018 (available at: https://www.mdpi.com/journal/ antioxidants/special issues/second messengers free radicals) For citation purposes, cite each article independently as indicated on the article page online and as indicated below: LastName, A.A.; LastName, B.B.; LastName, C.C. Article Title. Journal Name Year, Article Number, Page Range. ISBN 978-3-03897-533-5 (Pbk) ISBN 978-3-03897-534-2 (PDF) c 2019 by the authors. Articles in this book are Open Access and distributed under the Creative Commons Attribution (CC BY) license, which allows users to download, copy and build upon published articles, as long as the author and publisher are properly credited, which ensures maximum dissemination and a wider impact of our publications. The book as a whole is distributed by MDPI under the terms and conditions of the Creative Commons license CC BY-NC-ND. Contents About the Special Issue Editor ...................................... vii Preface to ”Antioxidants and Second Messengers of Free Radicals” ................ ix Neven Zarkovic Antioxidants and Second Messengers of Free Radicals Reprinted from: Antioxidants 2018, 7, 158, doi:10.3390/antiox7110158 ............... -

Plant Secondary Metabolites .Pdf
PLANT SECONDARY METABOLITES W W W . T R C - C A N A D A . C O M +1 (416) 665-9696 www.trc-canada.com 2 Brisbane Road, Toronto [email protected] Plant Secondary Metabolites Product CAS No CAT No Acanthopanax senticosides B 114902-16-8 Please Inquire Acetyl resveratrol 42206-94-0 R150055 Acetylshikonin 24502-78-1 Please Inquire Acronycine 7008-42-6 Please Inquire Acteoside 61276-17-3 V128000 Agrimol B 55576-66-4 Please Inquire Alisol-B-23-acetate 26575-95-1 A535970 Alisol-C-monoacetate 26575-93-9 Please Inquire Alizarin 72-48-0 A536600 Alkannin 517-88-4 Please Inquire Allantoin 97-59-6 A540500 Allantoin-13C2,15N4 1219402-51-3 A540502 Alliin 556-27-4 A543530 Aloe emodin 481-72-1 A575400 Aloe-emodin-d5 1286579-72-3 A575402 Aloenin A 38412-46-3 Please Inquire Aloin A 1415-73-2 A575415 Amentoflavone 1617-53-4 A576420 Amygdalin 29883-15-6 A576840 Andrographolide 5508-58-7 A637475 Angelicin 523-50-2 A637575 Anhydroicaritin 118525-40-9 I163700 Anisodamine 55869-99-3 Please Inquire Anthraquinone 84-65-1 A679245 Anthraquinone-D8 10439-39-1 A679247 Apigenin 520-36-5 A726500 Apigenin-d5 263711-74-6 A726502 Araloside X 344911-90-6 Please Inquire www.trc-canada.com I +1 (416) 665-9696 I [email protected] Plant Secondary Metabolites Arbutin 497-76-7 A766510 Arbutin-13C6 A766512 Arctigenin 7770-78-7 A766580 Arctiin 20362-31-6 A766575 Aristolochic acid I 313-67-7 A771300 Aristolochic acid II 475-80-9 A771305 Aristolochic acid sodium salt 10190-99-5 Please Inquire Aristololactam 13395-02-3 A771200 Artemisinin 63968-64-9 A777500 Artemisinin-d3 176652-07-6 -

Otto-Catalog-2019-20.Pdf
Lab Chemicals & More..... Otto Catalog 2019-20 1 CODE PRODUCT NAME CAS NO. PACKING RATE ` PACKING RATE ` A 1214 ABSCISIC ACID practical grade 10% 14375-45-2 100mg 2007 1gm 13059 A 1215 ABSCISIC ACID for biochemistry 99% 14375-45-2 25mg 1395 100mg 3609 500 mg 17469 A 1217 (7-AMINO CEPHALOSPORANIC ACID) 7-ACA 98% 957-68-6 1gm 2403 5gm 9396 A 1225 ACACIA 9000-01-5 500gm 504 5kg 4392 A 1226 ACACIA spray dried powder 9000-01-5 500gm 684 5kg 6309 A 1227 ACACIA GR 9000-01-5 500gm 828 5kg 7407 A 0855 ACARBOSE, >95% 56180-94-0 1 gm 18099 A 1229 ACENAPHTHENE pract 83-32-9 100gm 306 500gm 1395 5 kg 11907 A 1230 ACENAPHTHENE for synthesis 97% 83-32-9 100gm 450 500gm 1692 A 1231 ACENAPHTHENE GR for HLPC 83-32-9 100gm 1359 500gm 5533 A 1234 ACES BUFFER 99% 7365-82-4 5gm 864 25gm 2385 [N-(2-Acetamido)-2-aminoethane sulfonic acid] 100 gm 8739 A 1233 ACETALDEHYDE 20-30% solution for synthesis 75-07-0 500ml 477 5lt 4095 A 1235 ACETAMIDE for synthesis 99% 60-35-5 500 gm 801 A 1240 ACETAMIDINE CHLORIDE for synthesis 124-42-5 100gm 3159 250gm 7830 A 1242 N-(2-ACETAMIDO) IMINODIACETIC ACID (ADA BUFFER) 26239-55-4 25gm 855 100gm 2592 250 gm 5994 A 1245 ACETANILIDE for synthesis 98.5% 103-84-4 500gm 918 5kg 8289 A 1248 ACETATE BUFFER SOLUTION pH 4.6 - - - - - 500ml 180 5lt 1449 A 1250 ACETIC ACID glacial 99% 64-19-7 500ml 207 5lt 1602 A 1251 ACETIC ACID glacial GR 99%+ 64-19-7 500ml 252 5lt 1908 A 1252 ACETIC ACID GLACIAL GR 99.7% 64-19-7 500ml 315 5lt 1998 A 1253 ACETIC ACID GLACIAL EL 99.9% 64-19-7 500ml 378 5lt 2502 A 1254 ACETIC ACID 99.8% for HPLC 64-19-7 -

Dr. Duke's Phytochemical and Ethnobotanical Databases List of Chemicals for Tinnitus
Dr. Duke's Phytochemical and Ethnobotanical Databases List of Chemicals for Tinnitus Chemical Activity Count (+)-ALPHA-VINIFERIN 1 (+)-AROMOLINE 1 (+)-BORNYL-ISOVALERATE 1 (+)-CATECHIN 1 (+)-EUDESMA-4(14),7(11)-DIENE-3-ONE 1 (+)-HERNANDEZINE 2 (+)-ISOLARICIRESINOL 1 (+)-NORTRACHELOGENIN 1 (+)-PSEUDOEPHEDRINE 1 (+)-SYRINGARESINOL-DI-O-BETA-D-GLUCOSIDE 1 (+)-T-CADINOL 1 (-)-16,17-DIHYDROXY-16BETA-KAURAN-19-OIC 1 (-)-ALPHA-BISABOLOL 1 (-)-ANABASINE 1 (-)-APOGLAZIOVINE 1 (-)-BETONICINE 1 (-)-BORNYL-CAFFEATE 1 (-)-BORNYL-FERULATE 1 (-)-BORNYL-P-COUMARATE 1 (-)-CANADINE 1 (-)-DICENTRINE 1 (-)-EPICATECHIN 2 (-)-EPIGALLOCATECHIN-GALLATE 1 (1'S)-1'-ACETOXYCHAVICOL-ACETATE 1 (E)-4-(3',4'-DIMETHOXYPHENYL)-BUT-3-EN-OL 1 1,7-BIS-(4-HYDROXYPHENYL)-1,4,6-HEPTATRIEN-3-ONE 1 1,8-CINEOLE 4 Chemical Activity Count 1-ETHYL-BETA-CARBOLINE 2 10-ACETOXY-8-HYDROXY-9-ISOBUTYLOXY-6-METHOXYTHYMOL 1 10-DEHYDROGINGERDIONE 1 10-GINGERDIONE 1 12-(4'-METHOXYPHENYL)-DAURICINE 1 12-METHOXYDIHYDROCOSTULONIDE 1 13',II8-BIAPIGENIN 1 13-HYDROXYLUPANINE 1 13-OXYINGENOL-ESTER 1 16,17-DIHYDROXY-16BETA-KAURAN-19-OIC 1 16-HYDROXY-4,4,10,13-TETRAMETHYL-17-(4-METHYL-PENTYL)-HEXADECAHYDRO- 1 CYCLOPENTA[A]PHENANTHREN-3-ONE 16-HYDROXYINGENOL-ESTER 1 2'-O-GLYCOSYLVITEXIN 1 2-BETA,3BETA-27-TRIHYDROXYOLEAN-12-ENE-23,28-DICARBOXYLIC-ACID 1 2-METHYLBUT-3-ENE-2-OL 2 2-VINYL-4H-1,3-DITHIIN 1 20-DEOXYINGENOL-ESTER 1 22BETA-ESCIN 1 24-METHYLENE-CYCLOARTANOL 2 3,3'-DIMETHYLELLAGIC-ACID 1 3,4-DIMETHOXYTOLUENE 2 3,4-METHYLENE-DIOXYCINNAMIC-ACID-BORNYL-ESTER 1 3,4-SECOTRITERPENE-ACID-20-EPI-KOETJAPIC-ACID -

Antiviral, Antibacterial, Antifungal, and Antiparasitic Properties of Propolis: a Review
foods Review Antiviral, Antibacterial, Antifungal, and Antiparasitic Properties of Propolis: A Review Felix Zulhendri 1,* , Kavita Chandrasekaran 2 , Magdalena Kowacz 3, Munir Ravalia 4, Krishna Kripal 5, James Fearnley 6 and Conrad O. Perera 7,* 1 Kebun Efi, Kabanjahe, North Sumatra 2217, Indonesia 2 Peerzadiguda, Uppal, Hyderabad 500039, Telangana, India; [email protected] 3 Institute of Animal Reproduction and Food Research, Polish Academy of Sciences, Tuwima 10 St., 10-748 Olsztyn, Poland; [email protected] or [email protected] 4 The Royal London Hospital, Whitechapel Rd, Whitechapel, London E1 1FR, UK; [email protected] 5 Rajarajeswari Dental College & Hospital, No.14, Ramohalli Cross, Mysore Road, Kumbalgodu, Bengaluru 560074, Karnataka, India; [email protected] 6 Apiceutical Research Centre, Unit 3b Enterprise Way, Whitby, North Yorkshire YO18 7NA, UK; [email protected] 7 Food Science Program, School of Chemical Sciences, University of Auckland, 23 Symonds Street, Auckland CBD, Auckland 1010, New Zealand * Correspondence: authors:[email protected] (F.Z.); [email protected] or [email protected] (C.O.P.) Abstract: Propolis is a complex phytocompound made from resinous and balsamic material harvested by bees from flowers, branches, pollen, and tree exudates. Humans have used propolis therapeutically Citation: Zulhendri, F.; for centuries. The aim of this article is to provide comprehensive review of the antiviral, antibacterial, Chandrasekaran, K.; Kowacz, M.; antifungal, and antiparasitic properties of propolis. The mechanisms of action of propolis are Ravalia, M.; Kripal, K.; Fearnley, J.; discussed. There are two distinct impacts with regards to antimicrobial and anti-parasitic properties of Perera, C.O. -

Syzygium Aromaticum (L.) Merr. & Perry
Biological Evaluation and Semi-synthesis of Isolated Compounds from (Syzygium aromaticum (L.) Merr. & Perry) Buds Submitted in Partial Fulfillment for MSc. Degree in Organic Chemistry. In the Department of Chemistry, Faculty of Science and Agriculture, University of Fort Hare, Alice By Rali Sibusiso (200806318) Supervisor: Dr. O. O. Oyedeji Co-supervisor: Prof. B. N. Nkeh-Chungag 2014 DECLARATION I, RALI SIBUSISO (200806318), declare that this dissertation and the work presented in it are my own and has been generated by me as the result of my own original research. Biological evaluation and semi-synthesis of isolated compounds from (Syzygium aromaticum (L.) Merr. & Perry) buds I confirm that: 1. This work was done wholly or mainly while in candidature for a research degree at University of Fort Hare. 2. Where any part of this dissertation has previously been submitted for a degree or any other qualification at University of Fort Hare or any other institution, this has been clearly stated. 3. Where I have consulted the published work of others, this is always clearly attributed. 4. Where I have quoted from the work of others, the source is always given. With the exception of such quotations, this dissertation is entirely my own work. 5. I have acknowledged all main sources of help. 6. Where the dissertation is based on work done by myself jointly with others, I have made clear exactly what was done by others and what I have contributed myself. Signed: ………………………………………… Date: …………………………………………… i CERTIFICATE OF APPROVAL We hereby declare that this dissertation is from the student’s own work and effort, and all other sources of information used have been acknowledged. -
Reference Substances for Herbal Products Our Services
Reference Substances for Herbal Products Our Services As one of the leading manufacturers internationally, PhytoLab offers a broad portfolio of over 1,000 extensively documented herbal reference substances. Our product range reflects the whole diversity of natural product chemistry – from A for Anthocy- ans to X for Xanthones, PhytoLab offers you numerous representatives of all classes of natural substances phyproof® Reference Substances are Primary Reference Substances as defined by the European Pharmacopoeia and other international organizations. phyproof® Reference Substances are delivered at no extra cost together with: a data sheet with general information including the structural formula, molecular formula, molecular weight, CAS registry number, as well as the recommended storage conditions, handling instructions, and general safety information a certificate of analysis usually including* a description of general properties a list of the identity tests the substance passed a certified absolute content considering chromatographic purity as well as content of water, residual solvents and inorganic impurities * Very few exceptions apply to phyproof® Reference Substances available in limited quantities only. For detailed information on the analytical documentation delivered with each reference substance please visit our webshop at http://phyproof.phytolab.de or contact our reference substance team. Material safety data sheets (MSDS) are automatically provided with hazardous substances and are available for all other phyproof® Reference Substances upon request. Furthermore, the exact eight with two decimals is given on the label of each phyproof® Reference Substance vial, thus allowing the preparation of well-defined standard solutions without losing any valuable material. For marketing authorization purposes we deliver phyproof® Reference Substances upon request with full documentation (CTD module 3.2.S.5 /3.2.P.6) including the following data and information: NMR ( 1H and 13C) incl. -

External Preparation for the Skin and Beautifying Agents
Europäisches Patentamt *EP001295587A1* (19) European Patent Office Office européen des brevets (11) EP 1 295 587 A1 (12) EUROPEAN PATENT APPLICATION published in accordance with Art. 158(3) EPC (43) Date of publication: (51) Int Cl.7: A61K 7/00, A61K 7/48, 26.03.2003 Bulletin 2003/13 A61P 17/16 (21) Application number: 01917726.0 (86) International application number: PCT/JP01/02787 (22) Date of filing: 30.03.2001 (87) International publication number: WO 01/072265 (04.10.2001 Gazette 2001/40) (84) Designated Contracting States: (72) Inventors: AT BE CH CY DE DK ES FI FR GB GR IE IT LI LU • KUNO, Noriyasu; MC NL PT SE TR c/o THE NISSHIN OIL MILLS, LTD. Designated Extension States: Yokosuka-shi, Kanagawa 239-0832 (JP) AL LT LV MK RO SI • SHINOHARA, Gou; c/o THE NISSHIN OIL MILLS, LTD. (30) Priority: 31.03.2000 JP 2000097428 Yokosuka-shi, Kanagawa 239-0832 (JP) 29.08.2000 JP 2000258995 28.12.2000 JP 2000403353 (74) Representative: Bawden, Peter Charles et al Bawden & Associates, (71) Applicant: The Nisshin OilliO, Ltd. 4 The Gatehouse Tokyo 104-8285 (JP) 2 High Street Harpenden, Hertfordshire AL5 2TH (GB) (54) EXTERNAL PREPARATION FOR THE SKIN AND BEAUTIFYING AGENTS (57) The present invention relates to an external agent for the skin comprising at least one member selected from the group consisting of maslinic acid, erythrodiol, uvaol, betulinic acid, betulin, physiologically acceptable salts thereof and derivatives thereof. EP 1 295 587 A1 Printed by Jouve, 75001 PARIS (FR) EP 1 295 587 A1 Description Technical Field 5 [0001] The present invention relates to an external agent for the skin and more particularly to an external agent for the skin having a whitening effect as well as a whitening agent. -

Dr. Duke's Phytochemical and Ethnobotanical Databases List of Chemicals for Jaundice
Dr. Duke's Phytochemical and Ethnobotanical Databases List of Chemicals for Jaundice Chemical Activity Count (+)-ALPHA-VINIFERIN 2 (+)-CAMPHOR 1 (+)-CATECHIN 2 (+)-CATECHIN-7-O-GALLATE 1 (+)-CATECHOL 1 (+)-CYANIDANOL-3 1 (+)-EUDESMA-4(14),7(11)-DIENE-3-ONE 1 (+)-HERNANDEZINE 1 (+)-PSEUDOEPHEDRINE 1 (-)-16,17-DIHYDROXY-16BETA-KAURAN-19-OIC 1 (-)-ALPHA-BISABOLOL 1 (-)-BETONICINE 1 (-)-BORNYL-CAFFEATE 1 (-)-BORNYL-FERULATE 1 (-)-BORNYL-P-COUMARATE 1 (-)-EPICATECHIN 3 (-)-EPICATECHIN-3-O-GALLATE 1 (-)-EPIGALLOCATECHIN-GALLATE 3 (1'S)-1'-ACETOXYCHAVICOL-ACETATE 2 (E)-4-(3',4'-DIMETHOXYPHENYL)-BUT-3-EN-OL 1 1,2,3,4,6-PENTA-O-GALLOYL-GLUCOSE 1 1,4-DICAFFEOYLQUINIC-ACID 1 1,7-BIS-(4-HYDROXYPHENYL)-1,4,6-HEPTATRIEN-3-ONE 1 1,8-CINEOLE 3 1-O-GALLOYL-PEDUNCULAGIN 1 10-ACETOXY-8-HYDROXY-9-ISOBUTYLOXY-6-METHOXYTHYMOL 1 10-DEHYDROGINGERDIONE 2 Chemical Activity Count 10-GINGERDIONE 1 10-GINGEROL 1 10-METHOXYCAMPTOTHECIN 1 11-DEHYDROPAPYRIOGENIN 1 11-DEOXYGLYCYRRHETINIC-ACID 1 13',II8-BIAPIGENIN 2 13-OXYINGENOL-ESTER 1 16,17-DIHYDROXY-16BETA-KAURAN-19-OIC 1 16-EPISAIKOGENIN-C 1 16-HYDROXYINGENOL-ESTER 1 2'-O-GLYCOSYLVITEXIN 1 2,7-DIHYDROXYCADALENE 1 2-BETA,3BETA-27-TRIHYDROXYOLEAN-12-ENE-23,28-DICARBOXYLIC-ACID 1 2-METHYLTRICOSANE-8-ONE-23-OL 1 2-O-CAFFEOYL-(+)-ALLOHYDROXYCITRIC-ACID 1 20-DEOXYINGENOL-ESTER 1 22BETA-ESCIN 1 24-METHYLENE-CYCLOARTANOL 1 3,3'-DIMETHYLELLAGIC-ACID 1 3,3'-DIMETHYLQUERCETIN 1 3,4-METHYLENE-DIOXYCINNAMIC-ACID-BORNYL-ESTER 1 3,4-SECOTRITERPENE-ACID-20-EPI-KOETJAPIC-ACID 1 3,7'-DIMETHYLQUERCETIN 1 3-ACETYLACONITINE 1 3-BETA-HYDROXY-2,3-DIHYDROWITHANOLIDE-F -
Secondary Metabolites
PLANT SECONDARY METABOLITES WWW.TRC-CANADA.COM +1 (416) 665-9696 www.trc-canada.com 2 Brisbane Road, Toronto [email protected] Plant Secondary Metabolites Product CAS No CAT No Acanthopanax senticosides B 114902-16-8 Please Inquire Acetyl resveratrol 42206-94-0 R150055 Acetylshikonin 24502-78-1 Please Inquire Acronycine 7008-42-6 Please Inquire Acteoside 61276-17-3 V128000 Agrimol B 55576-66-4 Please Inquire Alisol-B-23-acetate 26575-95-1 A535970 Alisol-C-monoacetate 26575-93-9 Please Inquire Alizarin 72-48-0 A536600 Alkannin 517-88-4 Please Inquire Allantoin 97-59-6 A540500 Allantoin-13C2,15N4 1219402-51-3 A540502 Alliin 556-27-4 A543530 Aloe emodin 481-72-1 A575400 Aloe-emodin-d5 1286579-72-3 A575402 Aloenin A 38412-46-3 Please Inquire Aloin A 1415-73-2 A575415 Amentoflavone 1617-53-4 A576420 Amygdalin 29883-15-6 A576840 Andrographolide 5508-58-7 A637475 Angelicin 523-50-2 A637575 Anhydroicaritin 118525-40-9 I163700 Anisodamine 55869-99-3 Please Inquire Anthraquinone 84-65-1 A679245 Anthraquinone-D8 10439-39-1 A679247 Apigenin 520-36-5 A726500 Apigenin-d5 263711-74-6 A726502 Araloside X 344911-90-6 Please Inquire www.trc-canada.com I +1 (416) 665-9696 I [email protected] Plant Secondary Metabolites Arbutin 497-76-7 A766510 Arbutin-13C6 A766512 Arctigenin 7770-78-7 A766580 Arctiin 20362-31-6 A766575 Aristolochic acid I 313-67-7 A771300 Aristolochic acid II 475-80-9 A771305 Aristolochic acid sodium salt 10190-99-5 Please Inquire Aristololactam 13395-02-3 A771200 Artemisinin 63968-64-9 A777500 Artemisinin-d3 176652-07-6 A777502 Asiatic -

Anticancer Potential of Betulonic Acid Derivatives
International Journal of Molecular Sciences Review Anticancer Potential of Betulonic Acid Derivatives Adelina Lombrea 1,2 , Alexandra Denisa Scurtu 2,3,* , Stefana Avram 1,2, Ioana Zinuca Pavel 1,2 ,Maris¯ Turks 4, 4 5 2,3 2,6 1,2 Jevgen, ija Lugin, ina , Uldis Peipin, š , Cristina Adriana Dehelean , Codruta Soica and Corina Danciu 1 Department of Pharmacognosy, “Victor Babes” University of Medicine and Pharmacy, Eftimie Murgu Square, No. 2, 300041 Timisoara, Romania; [email protected] (A.L.); [email protected] (S.A.); [email protected] (I.Z.P.); [email protected] (C.D.) 2 Research Centre for Pharmaco-Toxicological Evaluation, “Victor Babes” University of Medicine and Pharmacy, Eftimie Murgu Square, No. 2, 300041 Timisoara, Romania; [email protected] (C.A.D.); [email protected] (C.S.) 3 Department of Toxicology, “Victor Babes” University of Medicine and Pharmacy, Eftimie Murgu Square, No. 2, 300041 Timisoara, Romania 4 Institute of Technology of Organic Chemistry, Faculty of Materials Science and Applied Chemistry, Riga Technical University, P. Valdena Str. 3, LV-1048 Riga, Latvia; [email protected] (M.T.); [email protected] (J.L.) 5 Nature Science Technologies Ltd., Saules Str. 19, LV-3601 Ventspils, Latvia; [email protected] 6 Department of Pharmaceutical Chemistry, “Victor Babes” University of Medicine and Pharmacy, Eftimie Murgu Square, No. 2, 300041 Timisoara, Romania * Correspondence: [email protected]; Tel.: +40-72-4688-140 Abstract: Clinical trials have evidenced that several natural compounds, belonging to the phytochem- ical classes of alkaloids, terpenes, phenols and flavonoids, are effective for the management of various types of cancer. -
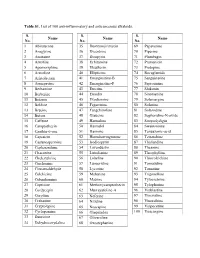
Table S1. List of 100 Anti-Inflammatory and Anticancerous Alkaloids
Table S1. List of 100 anti-inflammatory and anticancerous alkaloids. S. S. S. Name Name Name No. No. No. 1 Abiraterone 35 Deoxynojirimycin 69 Papaverine 2 Anagyrine 36 Dicentrine 70 Piperine 3 Anonaine 37 Diospyrin 71 Plumbagin 4 Antofine 38 Echitamine 72 Pramanicin 5 Apomorrphine 39 Eleutherin 73 Protopine 6 Arecoline 40 Ellipticine 74 Rocaglamide 7 Aristolactam 41 Emarginatine-B 75 Sanguinarine 8 Armepavine 42 Emarginatine-F 76 Saprosmine 9 Berbamine 43 Emetine 77 Shikonin 10 Berberine 44 Emodin 78 Sinomenine 11 Betanin 45 Evodiamine 79 Solamargine 12 Boldine 46 Fagaronine 80 Solanine 13 Brucine 47 Fangchinoline 81 Solasodine 14 Butein 48 Glaucine 82 Sophoridine-N-oxide 15 Caffeine 49 Harmaline 83 Streptolydigin 16 Camptothecin 50 Harmalol 84 Swainsonine 17 Canthin-6-one 51 Harmine 85 Tenuazonic-acid 18 Capsaicin 52 Homoharringtonine 86 Tetrandrine 19 Castanospermine 53 Isodiospyrin 87 Thaliandine 20 Cepharanthine 54 Lavendustin 88 Theanine 21 Chaconine 55 Liriodenine 89 Theophylline 22 Chelerythrine 56 Lobeline 90 Thiocolcichine 23 Cinchonine 57 Lunacridine 91 Tomatidine 24 Cinnamaldehyde 58 Lycorine 92 Tomatine 25 Colchicine 59 Mahanine 93 Trigonelline 26 Columbamine 60 Matrine 94 Tylocrebrine 27 Coptisine 61 Methoxycamptothecin 95 Tylophorine 28 Cordycepin 62 Murrayafoline-A 96 Vinblastine 29 Corydine 63 Neferine 97 Vincristine 30 Crebanine 64 Nitidine 98 Vinorelbine 31 Cryptolepine 65 Noscapine 99 Vinpocetine 32 Cyclopamine 66 Olaquindox 100 Voacangine 33 Dauricine 67 Oliveroline 34 Dehydrocorydaline 68 Oxostephanine Table S2. List