Neuro-Immune Interactions in Allergic Diseases: Novel Targets for Therapeutics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Histamine H4 Receptor: a Novel Target for Safe Anti-Inflammatory
GASTRO ISSN 2377-8369 Open Journal http://dx.doi.org/10.17140/GOJ-1-103 Review The Histamine H4 Receptor: A Novel Target *Corresponding author Maristella Adami, PhD for Safe Anti-inflammatory Drugs? Department of Neuroscience University of Parma Via Volturno 39 43125 Parma Italy * 1 Tel. +39 0521 903943 Maristella Adami and Gabriella Coruzzi Fax: +39 0521 903852 E-mail: [email protected] Department of Neuroscience, University of Parma, Via Volturno 39, 43125 Parma, Italy Volume 1 : Issue 1 1retired Article Ref. #: 1000GOJ1103 Article History Received: May 30th, 2014 ABSTRACT Accepted: June 12th, 2014 th Published: July 16 , 2014 The functional role of histamine H4 receptors (H4Rs) in the Gastrointestinal (GI) tract is reviewed, with particular reference to their involvement in the regulation of gastric mucosal defense and inflammation. 4H Rs have been detected in different cell types of the gut, including Citation immune cells, paracrine cells, endocrine cells and neurons, from different animal species and Adami M, Coruzzi G. The Histamine H4 Receptor: a novel target for safe anti- humans; moreover, H4R expression was reported to be altered in some pathological conditions, inflammatory drugs?. Gastro Open J. such as colitis and cancer. Functional studies have demonstrated protective effects of H4R an- 2014; 1(1): 7-12. doi: 10.17140/GOJ- tagonists in several experimental models of gastric mucosal damage and intestinal inflamma- 1-103 tion, suggesting a potential therapeutic role of drugs targeting this new receptor subtype in GI disorders, such as allergic enteropathy, Inflammatory Bowel Disease (IBD), Irritable Bowel Syndrome (IBS) and cancer. KEYWORDS: Histamine H4 receptor; Stomach; Intestine. -

Insulin and Insulin-Like Growth Factor II Permit Nerve Growth Factor Binding
Proc. Natl. Acad. Sci. USA Vol. 81, pp. 2562-2566, April 1984 Neurobiology Insulin and insulin-like growth factor II permit nerve growth factor binding and the neurite formation response in cultured human neuroblastoma cells (axons/differentiation/nerve growth factor receptor/pheochromocytoma PC12) ESPERANZA RECIO-PINTO, FREDERICK F. LANG, AND DOUGLAS N. ISHII* Department of Pharmacology and Cancer Research Center, College of Physicians and Surgeons of Columbia University, New York, NY 10032 Communicated by I. S. Edelman, January 3, 1984 ABSTRACT In serum-free medium, SH-SY5Y human mouse saliva (16); purity was confirmed by the single band in neuroblastoma cells specifically and reversibly lost the capaci- polyacrylamide gels subjected to isoelectric focusing (pH ty to bind 1251-labeled nerve growth factor (NGF) to the high- 3.5-10), or NaDodSO4 gel electrophoresis and by bioassay affinity sites (slow sites) and to respond by neurite outgrowth, (17). Anti-insulin antiserum was from Cappel Laboratories unless physiological concentrations of insulin or insulin-like (Cochranville, PA). The cloned cell line SH-SY5Y (7) was a growth factor II were present. In serum-containing medium, kind gift from June L. Biedler and Barbara A. Spengler. anti-insulin antiserum decreased the neurite formation re- Cells between passage numbers 9 and 29 were studied. The sponse to NGF, and insulin supplementation increased the cloned PC12 cell line (18) was the kind gift of Lloyd A. number of available NGF slow sites. The low-affinity NGF fast Greene and was subcloned prior to use. sites are absent from SH-SY5Y cells and did not emerge on Cell Culture. -
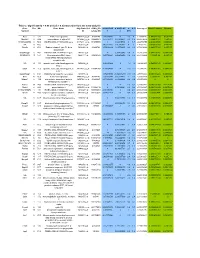
Table 2. Significant
Table 2. Significant (Q < 0.05 and |d | > 0.5) transcripts from the meta-analysis Gene Chr Mb Gene Name Affy ProbeSet cDNA_IDs d HAP/LAP d HAP/LAP d d IS Average d Ztest P values Q-value Symbol ID (study #5) 1 2 STS B2m 2 122 beta-2 microglobulin 1452428_a_at AI848245 1.75334941 4 3.2 4 3.2316485 1.07398E-09 5.69E-08 Man2b1 8 84.4 mannosidase 2, alpha B1 1416340_a_at H4049B01 3.75722111 3.87309653 2.1 1.6 2.84852656 5.32443E-07 1.58E-05 1110032A03Rik 9 50.9 RIKEN cDNA 1110032A03 gene 1417211_a_at H4035E05 4 1.66015788 4 1.7 2.82772795 2.94266E-05 0.000527 NA 9 48.5 --- 1456111_at 3.43701477 1.85785922 4 2 2.8237185 9.97969E-08 3.48E-06 Scn4b 9 45.3 Sodium channel, type IV, beta 1434008_at AI844796 3.79536664 1.63774235 3.3 2.3 2.75319499 1.48057E-08 6.21E-07 polypeptide Gadd45gip1 8 84.1 RIKEN cDNA 2310040G17 gene 1417619_at 4 3.38875643 1.4 2 2.69163229 8.84279E-06 0.0001904 BC056474 15 12.1 Mus musculus cDNA clone 1424117_at H3030A06 3.95752801 2.42838452 1.9 2.2 2.62132809 1.3344E-08 5.66E-07 MGC:67360 IMAGE:6823629, complete cds NA 4 153 guanine nucleotide binding protein, 1454696_at -3.46081884 -4 -1.3 -1.6 -2.6026947 8.58458E-05 0.0012617 beta 1 Gnb1 4 153 guanine nucleotide binding protein, 1417432_a_at H3094D02 -3.13334396 -4 -1.6 -1.7 -2.5946297 1.04542E-05 0.0002202 beta 1 Gadd45gip1 8 84.1 RAD23a homolog (S. -

Nerve Growth Factor- and Neurotrophin-3-Induced Changes in Nociceptive Threshold and the Release of Substance P from the Rat Isolated Spinal Cord
The Journal of Neuroscience, November 1, 1997, 17(21):8459–8467 Nerve Growth Factor- and Neurotrophin-3-Induced Changes in Nociceptive Threshold and the Release of Substance P from the Rat Isolated Spinal Cord Marzia Malcangio, Neil E. Garrett, Simon Cruwys, and David R. Tomlinson Department of Pharmacology, St. Bartholomew’s and the Royal London School of Medicine and Dentistry, Queen Mary and Westfield College, London E1 4NS, United Kingdom Acute superfusion of nerve growth factor (NGF; 1–100 ng/ml) istration, NGF had induced thermal and mechanical hyperalge- through a naive rat spinal cord preparation did not alter basal or sia in the rat hindpaw, and NT-3 had induced mechanical, but electrically evoked release of substance P-like immunoreactiv- not thermal, hypoalgesia. NT-3 administered six times over a 2 ity (SP-LI). In contrast, neurotrophin-3 (NT-3; 1–100 ng/ml), week period (at 1 mg/kg) did not alter thermal threshold but although not modifying SP-LI basal outflow, dose-dependently significantly reduced electrically evoked release of SP-LI from inhibited the electrically evoked, but not capsaicin (10 nM)- the spinal cord. An identical treatment regimen with 1 mg/kg induced, release of the peptide. This NT-3 (10 ng/ml)-induced NGF induced a significant increase in evoked release of SP-LI. inhibition persisted even in the presence of 100 ng/ml NGF in However, this was not associated with a significant hyperalge- the perfusion fluid and was still significant when the evoked sia. Although finding that NGF-induced hyperalgesia does not release of SP-LI was enhanced by a prolonged in vivo treatment clearly correlate with changes in the release of SP-LI in the with NGF. -

Differential Effects of Dehydroepiandrosterone and Testosterone in Prostate and Colon Cancer Cell Apoptosis: the Role of Nerve Growth Factor (NGF) Receptors
DHEA e testosterona e apoptose no câncer de próstata e de colon, papel do NGF – fator de crescimento neural. Differential effects of dehydroepiandrosterone and testosterone in prostate and colon cancer cell apoptosis: the role of nerve growth factor (NGF) receptors. Anagnostopoulou V1, Pediaditakis I, Alkahtani S, Alarifi SA, Schmidt EM, Lang F, Gravanis A, Charalampopoulos I, Stournaras C. Endocrinology. 2013 Jul;154(7):2446-56. Author information 1 Department of Biochemistry, University of Crete Medical School, GR-71003 Heraklion, Greece. Abstract Tumor growth is fostered by inhibition of cell death, which involves the receptiveness of tumor to growth factors and hormones. We have recently shown that testosterone exerts proapoptotic effects in prostate and colon cancer cells through a membrane-initiated mechanism. In addition, we have recently reported that dehydroepiandrosterone (DHEA) can control cell fate, activating nerve growth factor (NGF) receptors, namely tropomyosin-related kinase (Trk)A and p75 neurotrophin receptor, in primary neurons and in PC12 tumoral cells. NGF was recently involved in cancer cell proliferation and apoptosis. In the present study, we explored the cross talk between androgens (testosterone and DHEA) and NGF in regulating apoptosis of prostate and colon cancer cells. DHEA and NGF strongly blunted serum deprivation-induced apoptosis, whereas testosterone induced apoptosis of both cancer cell lines. The antiapoptotic effect of both DHEA and NGF was completely reversed by testosterone. In line with this, DHEA or NGF up-regulated, whereas testosterone down- regulated, the expression of TrkA receptor. The effects of androgens were abolished in both cell lines in the presence of TrkA inhibitor. DHEA induced the phosphorylation of TrkA and the interaction of p75 neurotrophin receptor with its effectors, Rho protein GDP dissociation inhibitor and receptor interacting serine/threonine-protein kinase 2. -

Histamine Receptors
Tocris Scientific Review Series Tocri-lu-2945 Histamine Receptors Iwan de Esch and Rob Leurs Introduction Leiden/Amsterdam Center for Drug Research (LACDR), Division Histamine is one of the aminergic neurotransmitters and plays of Medicinal Chemistry, Faculty of Sciences, Vrije Universiteit an important role in the regulation of several (patho)physiological Amsterdam, De Boelelaan 1083, 1081 HV, Amsterdam, The processes. In the mammalian brain histamine is synthesised in Netherlands restricted populations of neurons that are located in the tuberomammillary nucleus of the posterior hypothalamus.1 Dr. Iwan de Esch is an assistant professor and Prof. Rob Leurs is These neurons project diffusely to most cerebral areas and have full professor and head of the Division of Medicinal Chemistry of been implicated in several brain functions (e.g. sleep/ the Leiden/Amsterdam Center of Drug Research (LACDR), VU wakefulness, hormonal secretion, cardiovascular control, University Amsterdam, The Netherlands. Since the seventies, thermoregulation, food intake, and memory formation).2 In histamine receptor research has been one of the traditional peripheral tissues, histamine is stored in mast cells, eosinophils, themes of the division. Molecular understanding of ligand- basophils, enterochromaffin cells and probably also in some receptor interaction is obtained by combining pharmacology specific neurons. Mast cell histamine plays an important role in (signal transduction, proliferation), molecular biology, receptor the pathogenesis of various allergic conditions. After mast cell modelling and the synthesis and identification of new ligands. degranulation, release of histamine leads to various well-known symptoms of allergic conditions in the skin and the airway system. In 1937, Bovet and Staub discovered compounds that antagonise the effect of histamine on these allergic reactions.3 Ever since, there has been intense research devoted towards finding novel ligands with (anti-) histaminergic activity. -

H4R) and the Human Free Fatty Acid Receptor 4 (FFA4)
Evaluation of signalling and phosphorylation responses of the human histamine H4 receptor (H4R) and the human free fatty acid receptor 4 (FFA4) Thesis Submitted for the Degree of Doctor of Philosophy at the University of Leicester By Sajjad Ali Riaz Department of Molecular and Cellular Biology University of Leicester May 2016 Abstract The knowledge that G protein-coupled receptors (GPCRs) are regulated by phosphorylation in a process that results in the recruitment of arrestins, leading to receptor desensitisation is now well known. The histamine H4 receptor (H4R) and the free fatty acid receptor 4 (FFA4) are family A GPCRs that both have the ability to become phosphorylated in their third intracellular loops and C-terminal tails by kinases found in the cytosolic milieu of the cells and tissues they are expressed in. Investigations into the phosphorylation status of the histamine H4 receptor have revealed a receptor that is highly phosphorylated even in the basal state. The endogenous, full agonist for the human H4R, histamine, induced a robust increase in receptor phosphorylation. However, the β-arrestin-biased agonist JNJ7777120 did not. Extending this study using mass spectrometry revealed the individual sites of phosphorylation. Histamine and JNJ7777120 also caused H4R internalisation. Our data suggests a similar level of endocytosis induced by histamine and JNJ7777120 at 5 or 30 min stimulation. Thus, we show that JNJ7777120, while previously demonstrating its differing effects on H4R signalling, also shows differences in the phosphorylation of the H4R when compared to histamine. Using the wild type FFA4 receptor and its phosphorylation-deficient mutants, we show the importance of phosphorylation in the recruitment of arrestin to the receptor as well as delineating G protein-dependent and independent downstream signalling pathways. -
Effects of BNN27, a Novel C17-Spiroepoxy Steroid Derivative
www.nature.com/scientificreports OPEN Efects of BNN27, a novel C17- spiroepoxy steroid derivative, on experimental retinal detachment- Received: 18 July 2017 Accepted: 26 June 2018 induced photoreceptor cell death Published: xx xx xxxx Pavlina Tsoka 1,4, Hidetaka Matsumoto4, Daniel E. Maidana 4, Keiko Kataoka4, Irene Naoumidi1, Achille Gravanis2,3, Demetrios G. Vavvas4 & Miltiadis K. Tsilimbaris1 Retinal detachment (RD) leads to photoreceptor cell death secondary to the physical separation of the retina from the underlying retinal pigment epithelium. Intensifying photoreceptor survival in the detached retina could be remarkably favorable for many retinopathies in which RD can be seen. BNN27, a blood-brain barrier (BBB)-permeable, C17-spiroepoxy derivative of dehydroepiandrosterone (DHEA) has shown promising neuroprotective activity through interaction with nerve growth factor receptors, TrkA and p75NTR. Here, we administered BNN27 systemically in a murine model of RD. TUNEL+ photoreceptors were signifcantly decreased 24 hours post injury after a single administration of 200 mg/kg BNN27. Furthermore, BNN27 increased infammatory cell infltration, as well as, two markers of gliosis 24 hours post RD. However, single or multiple doses of BNN27 were not able to protect the overall survival of photoreceptors 7 days post injury. Additionally, BNN27 did not induce the activation/phosphorylation of TrkAY490 in the detached retina although the mRNA levels of the receptor were increased in the photoreceptors post injury. Together, these fndings, do not demonstrate neuroprotective activity of BNN27 in experimentally-induced RD. Further studies are needed in order to elucidate the paradox/contradiction of these results and the mechanism of action of BNN27 in this model of photoreceptor cell damage. -

Gene Standard Deviation MTOR 0.12553731 PRPF38A
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) Gut Gene Standard Deviation MTOR 0.12553731 PRPF38A 0.141472605 EIF2B4 0.154700091 DDX50 0.156333027 SMC3 0.161420017 NFAT5 0.166316903 MAP2K1 0.166585267 KDM1A 0.16904912 RPS6KB1 0.170330192 FCF1 0.170391706 MAP3K7 0.170660513 EIF4E2 0.171572093 TCEB1 0.175363093 CNOT10 0.178975095 SMAD1 0.179164705 NAA15 0.179904998 SETD2 0.180182498 HDAC3 0.183971158 AMMECR1L 0.184195031 CHD4 0.186678211 SF3A3 0.186697697 CNOT4 0.189434633 MTMR14 0.189734199 SMAD4 0.192451524 TLK2 0.192702667 DLG1 0.19336621 COG7 0.193422331 SP1 0.194364189 PPP3R1 0.196430217 ERBB2IP 0.201473001 RAF1 0.206887192 CUL1 0.207514271 VEZF1 0.207579584 SMAD3 0.208159809 TFDP1 0.208834504 VAV2 0.210269344 ADAM17 0.210687138 SMURF2 0.211437666 MRPS5 0.212428684 TMUB2 0.212560675 SRPK2 0.216217428 MAP2K4 0.216345366 VHL 0.219735582 SMURF1 0.221242495 PLCG1 0.221688351 EP300 0.221792349 Sundar R, et al. Gut 2020;0:1–10. doi: 10.1136/gutjnl-2020-320805 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) Gut MGAT5 0.222050228 CDC42 0.2230598 DICER1 0.225358787 RBX1 0.228272533 ZFYVE16 0.22831803 PTEN 0.228595789 PDCD10 0.228799406 NF2 0.23091035 TP53 0.232683696 RB1 0.232729172 TCF20 0.2346075 PPP2CB 0.235117302 AGK 0.235416298 -
Neurotransmitter and Neuropeptide Regulation of Mast Cell Function
Xu et al. Journal of Neuroinflammation (2020) 17:356 https://doi.org/10.1186/s12974-020-02029-3 REVIEW Open Access Neurotransmitter and neuropeptide regulation of mast cell function: a systematic review Huaping Xu1, Xiaoyun Shi2, Xin Li3, Jiexin Zou4, Chunyan Zhou5, Wenfeng Liu5, Huming Shao5, Hongbing Chen5 and Linbo Shi4* Abstract The existence of the neural control of mast cell functions has long been proposed. Mast cells (MCs) are localized in association with the peripheral nervous system (PNS) and the brain, where they are closely aligned, anatomically and functionally, with neurons and neuronal processes throughout the body. They express receptors for and are regulated by various neurotransmitters, neuropeptides, and other neuromodulators. Consequently, modulation provided by these neurotransmitters and neuromodulators allows neural control of MC functions and involvement in the pathogenesis of mast cell–related disease states. Recently, the roles of individual neurotransmitters and neuropeptides in regulating mast cell actions have been investigated extensively. This review offers a systematic review of recent advances in our understanding of the contributions of neurotransmitters and neuropeptides to mast cell activation and the pathological implications of this regulation on mast cell–related disease states, though the full extent to which such control influences health and disease is still unclear, and a complete understanding of the mechanisms underlying the control is lacking. Future validation of animal and in vitro models also is needed, which incorporates the integration of microenvironment-specific influences and the complex, multifaceted cross-talk between mast cells and various neural signals. Moreover, new biological agents directed against neurotransmitter receptors on mast cells that can be used for therapeutic intervention need to be more specific, which will reduce their ability to support inflammatory responses and enhance their potential roles in protecting against mast cell–related pathogenesis. -

I AMYLIN MEDIATES BRAINSTEM
AMYLIN MEDIATES BRAINSTEM CONTROL OF HEART RATE IN THE DIVING REFLEX A Dissertation Submitted to The Temple University Graduate Board In Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy By Fan Yang May, 2012 Examination committee members: Dr. Nae J Dun (advisor), Dept. of Pharmacology, Temple University Dr. Alan Cowan, Dept. of Pharmacology, Temple University Dr. Lee-Yuan Liu-Chen, Dept. of Pharmacology, Temple University Dr. Gabriela Cristina Brailoiu, Dept. of Pharmacology, Temple University Dr. Parkson Lee-Gau Chong, Dept. of Biochemistry, Temple University Dr. Hreday Sapru (external examiner), Depts. of Neurosciences, Neurosurgery & Pharmacology/Physiology, UMDNJ-NJMS. i © 2012 By Fan Yang All Rights Reserved ii ABSTRACT AMYLIN’S ROLE AS A NEUROPEPTIDE IN THE BRAINSTEM Fan Yang Doctor of Philosophy Temple University, 2012 Doctoral Advisory Committee Chair: Nae J Dun, Ph.D. Amylin, or islet amyloid polypeptide is a 37-amino acid member of the calcitonin peptide family. Amylin role in the brainstem and its function in regulating heart rates is unknown. The diving reflex is a powerful autonomic reflex, however no neuropeptides have been described to modulate its function. In this thesis study, amylin expression in the brainstem involving pathways between the trigeminal ganglion and the nucleus ambiguus was visualized and characterized using immunohistochemistry. Its functional role in slowing heart rate and also its involvement in the diving reflex were elucidated using stereotaxic microinjection, whole-cel patch-clamp, and a rat diving model. Immunohistochemical and tract tracing studies in rats revealed amylin expression in trigeminal ganglion cells, which also contained vesicular glutamate transporter 2 positive. -

A G-Protein-Coupled Receptor Mediates Neuropeptide-Induced
bioRxiv preprint doi: https://doi.org/10.1101/801225; this version posted October 10, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. A G-protein-coupled receptor mediates neuropeptide-induced oocyte maturation in the jellyfish Clytia Gonzalo Quiroga Artigas1#, Pascal Lapébie1, Lucas Leclère1, Philip Bauknecht 2, Julie Uveira1, Sandra Chevalier1, Gáspár Jékely2,3, Tsuyoshi Momose1 and Evelyn Houliston1* 1. Sorbonne University, CNRS, Villefranche-sur-mer Developmental Biology Laboratory (LBDV), 06230 Villefranche-sur-mer, France 2. Max Planck Institute for Developmental Biology, Spemannstraße 35, 72076 Tübingen, Germany. 3. Living Systems Institute, University of Exeter, Stocker Road, EX4 4QD, Exeter, UK # current address: GQA: The Whitney Laboratory for Marine Bioscience, University of Florida, St. Augustine, FL, USA *Corresponding author: E. Houliston [email protected] Short title: The Clytia oocyte maturation hormone receptor 1 bioRxiv preprint doi: https://doi.org/10.1101/801225; this version posted October 10, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Abstract The reproductive hormones that trigger oocyte meiotic maturation and release from the ovary vary greatly between animal species. Identification of receptors for these Maturation Inducing Hormones (MIHs), and understanding how they initiate the largely conserved maturation process, remain important challenges.