Radiation Treatment and Cisplatin Chemotherapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Induction with Mitomycin C, Doxorubicin, Cisplatin And
British Journal of Cancer (1999) 80(12), 1962–1967 © 1999 Cancer Research Campaign Article no. bjoc.1999.0627 Induction with mitomycin C, doxorubicin, cisplatin and maintenance with weekly 5-fluorouracil, leucovorin for treatment of metastatic nasopharyngeal carcinoma: a phase II study RL Hong1, TS Sheen2, JY Ko2, MM Hsu2, CC Wang1 and LL Ting3 Departments of 1Oncology, 2Otolaryngology and 3Radiation Therapy, National Taiwan University Hospital, National Taiwan University, No. 7, Chung-Shan South Road, Taipei 10016, Taiwan Summary The combination of cisplatin and 5-fluorouracil (5-FU) (PF) is the most popular regimen for treating metastatic nasopharyngeal carcinoma (NPC) but it is limited by severe stomatitis and chronic cisplatin-related toxicity. A novel approach including induction with mitomycin C, doxorubicin and cisplatin (MAP) and subsequent maintenance with weekly 5-FU and leucovorin (FL) were designed with an aim to reduce acute and chronic toxicity of PF. Thirty-two patients of NPC with measurable metastatic lesions in the liver or lung were entered into this phase II trial. Mitomycin C 8 mg m–2, doxorubicin 40 mg m–2 and cisplatin 60 mg m–2 were given on day 1 every 3 weeks as initial induction. After either four courses or remission was achieved, patients received weekly dose of 5-FU 450 mg m–2 and leucovorin 30 mg m–2 for maintenance until disease progression. With 105 courses of MAP given, 5% were accompanied by grade 3 and 0% were accompanied by grade 4 stomatitis. The dose-limiting toxicity of MAP was myelosuppression. Forty per cent of courses had grade 3 and 13% of courses had grade 4 leukopenia. -

Arsenic Trioxide Is Highly Cytotoxic to Small Cell Lung Carcinoma Cells
160 Arsenic trioxide is highly cytotoxic to small cell lung carcinoma cells 1 1 Helen M. Pettersson, Alexander Pietras, effect of As2O3 on SCLC growth, as suggested by an Matilda Munksgaard Persson,1 Jenny Karlsson,1 increase in neuroendocrine markers in cultured cells. [Mol Leif Johansson,2 Maria C. Shoshan,3 Cancer Ther 2009;8(1):160–70] and Sven Pa˚hlman1 1Center for Molecular Pathology, CREATE Health and 2Division of Introduction Pathology, Department of Laboratory Medicine, Lund University, 3 Lung cancer is the most frequent cause of cancer deaths University Hospital MAS, Malmo¨, Sweden; and Department of f Oncology-Pathology, Cancer Center Karolinska, Karolinska worldwide and results in 1 million deaths each year (1). Institute and Hospital, Stockholm, Sweden Despite novel treatment strategies, the 5-year survival rate of lung cancer patients is only f15%. Small cell lung carcinoma (SCLC) accounts for 15% to 20% of all lung Abstract cancers diagnosed and is a very aggressive malignancy Small cell lung carcinoma (SCLC) is an extremely with early metastatic spread (2). Despite an initially high aggressive form of cancer and current treatment protocols rate of response to chemotherapy, which currently com- are insufficient. SCLC have neuroendocrine characteristics bines a platinum-based drug with another cytotoxic drug and show phenotypical similarities to the childhood tumor (3, 4), relapses occur in the absolute majority of SCLC neuroblastoma. As multidrug-resistant neuroblastoma patients. At relapse, the efficacy of further chemotherapy is cells are highly sensitive to arsenic trioxide (As2O3) poor and the need for alternative treatments is obvious. in vitro and in vivo, we here studied the cytotoxic effects Arsenic-containing compounds have been used in tradi- of As2O3 on SCLC cells. -

Combination of Oxoplatin with Other FDA-Approved Oncology Drugs
International Journal of Molecular Sciences Article Theoretical Prediction of Dual-Potency Anti-Tumor Agents: Combination of Oxoplatin with Other FDA-Approved Oncology Drugs José Pedro Cerón-Carrasco Reconocimiento y Encapsulación Molecular, Universidad Católica San Antonio de Murcia Campus los Jerónimos, 30107 Murcia, Spain; [email protected] Received: 16 April 2020; Accepted: 2 July 2020; Published: 3 July 2020 Abstract: Although Pt(II)-based drugs are widely used to treat cancer, very few molecules have been approved for routine use in chemotherapy due to their side-effects on healthy tissues. A new approach to reducing the toxicity of these drugs is generating a prodrug by increasing the oxidation state of the metallic center to Pt(IV), a less reactive form that is only activated once it enters a cell. We used theoretical tools to combine the parent Pt(IV) prodrug, oxoplatin, with the most recent FDA-approved anti-cancer drug set published by the National Institute of Health (NIH). The only prerequisite imposed for the latter was the presence of one carboxylic group in the structure, a chemical feature that ensures a link to the coordination sphere via a simple esterification procedure. Our calculations led to a series of bifunctional prodrugs ranked according to their relative stabilities and activation profiles. Of all the designed molecules, the combination of oxoplatin with aminolevulinic acid as the bioactive ligand emerged as the most promising strategy by which to design enhanced dual-potency oncology drugs. Keywords: cancer; drug design; organometallics; platinum-based drugs; bifunctional compounds; theoretical tools 1. Introduction The unexpected discovery of the bioactivity of Pt salts by Rosenberg about 60 years ago opened the door to a new type of cancer treatment: chemotherapy with transition metals [1]. -
Small Cell Lung Cancer (SCLC) Algorithm
Small Cell Lung Cancer (SCLC) Page 1 of 8 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. Note: Consider Clinical Trials as treatment options for eligible patients. INITIAL EVALUATION STAGE ● Pathology consistent with SCLC Limited Stage ● History and physical AJCC Stage I-III2, see Page 2 ● Laboratory studies to include hematological and full chemistry panels ● FDG PET/CT and CT chest with IV contrast ○ If FDG PET/CT not available: nuclear medicine bone scan and CT chest, abdomen, and pelvis with IV contrast ● MRI brain with IV contrast (preferred) or CT head with IV contrast ● MRI spine, lumbar puncture and bone marrow aspirate/biopsy as indicated ● Pulmonary function tests 1 Extensive Stage ● Lifestyle risk assessment AJCC Stage IV3, see Page 3 ● Molecular profiling (for never smokers) AJCC = American Joint Committee on Cancer 1 See Physical Activity, Nutrition, and Tobacco Cessation algorithms; ongoing reassessment of lifestyle risks should be a part of routine clinical practice 2 Limited stage: Stage I-III (T any, N any, M0) per AJCC 8th edition or disease confined to the ipsilateral hemithorax -

Cisplatin and Etoposide (Lung)
Cisplatin and Etoposide (lung) _____________________________________________________________________________________________ Indication First line chemotherapy for patients with small cell lung cancer (SCLC), who have a good performance status (WHO PS 0-2). Concomitant radiotherapy may start with cycle 2. ICD-10 codes Codes pre-fixed with C34 Regimen details Day Drug Dose Route 1 Cisplatin 75-80mg/m² IV infusion 1 Etoposide 100mg/m² IV infusion 2 and 3 or Etoposide 100mg/m² IV infusion 2 and 3 Etoposide 200mg/m2 PO Cycle frequency 21 days Number of cycles 4 - 6 cycles (usually 4) Administration Cisplatin is administered in 500mL sodium chloride 0.9% over 60 minutes following the pre and post hydration protocol below. Infusion Fluid & Additives Volume Infusion Time Sodium Chloride 0.9% 1000mL 1 hour Mannitol 20% 200mL 30 minutes OR Mannitol 10% 400mL 30 minutes Ensure urine output > 100mL / hour prior to giving cisplatin. Give a single dose of furosemide 20mg iv if necessary. Cisplatin 500mL 1 hour Sodium Chloride 0.9% + 2g MgSO4 + 1000mL 2 hours 20mmol KCl TOTAL 2700mL or 2900mL 4 hours 30 minutes Note: Patients with magnesium or potassium below the normal range should have 2g MgSO4 and 20mmol KCl added to the pre-hydration bag and the duration of the infusion increased to 2 hours. All patients must be advised to drink at least 2 litres of fluid over the following 24 hours. IV etoposide is administered in 1000mL sodium chloride 0.9% and infused over a minimum of 1 hour. Version 1 Review date June 2018 Page 1 of 4 Oral etoposide is available as 50mg and 100mg capsules. -

Combination Chemotherapy with Estramustine Phosphate, Ifosfamide and Cisplatin for Hormone-Refractory Prostate Cancer
Acta Med. Okayama, 2006 Vol. 60, No. 1, pp. 43ン49 CopyrightⒸ 2006 by Okayama University Medical School. Original Article http ://www.lib.okayama-u.ac.jp/www/acta/ Combination Chemotherapy with Estramustine Phosphate, Ifosfamide and Cisplatin for Hormone-refractory Prostate Cancer Haruki Kakua, Takashi Saikaa*, Tomoyasu Tsushimab, Atsushi Nagaia, Teruhiko Yokoyamaa, Fernando Abarzuaa, Shin Ebaraa, Daisuke Manabea, Yasutomo Nasua, and Hiromi Kumona aDepartment of Urology, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama 700ン8558, Japan, and bDepartment of Urology, Medival center of Okayama, Okayama 701-1192, Japan We evaluated the effi ciency and toxicity of estramustine phosphate (ECT), ifosfamide (IFM) and cis- platin (CDDP) combination chemotherapy in twenty-one patients with hormone-refractory prostate cancer (HRPC), for which there is currently no eff ective treatment. Patients received a daily dose of 560 mg ECT in combination with 1.2 g/m2 IFM on days 1 to 5 and 70 mg/m2 CDDP on day 1. This combination therapy was given every 3 to 4 weeks. An objective response of more than 50オ reduc- tion in prostate-specifi c antigen was observed in 9 of 18 patients (50オ), and a more than 50オ reduc- tion in bi-dimensionally measurable soft-tissue lesions was observed in 2 of 7 patients (29オ). The median duration of response among the cases showing partial response was 40 weeks, while the median duration of response of overall partial-response plus stable cases was 30 weeks. The median survival duration of all cases was 47 weeks. Toxicity was modest and acceptable. In conclusion, the ECT, IFM and CDDP combination chemotherapy regimen is a viable treatment option for HRPC. -

Utilization of Arsenic Trioxide As a Treatment of Cisplatin-Resistant Non-Small Cell Lung Cancer PC-9/CDDP and PC-14/CDDP Cells
ONCOLOGY LETTERS 10: 805-809, 2015 Utilization of arsenic trioxide as a treatment of cisplatin-resistant non-small cell lung cancer PC-9/CDDP and PC-14/CDDP cells TOSHIHIRO SUZUKI1, KENICHI ISHIBASHI1, ATSUSHI YUMOTO1, KAZUTO NISHIO2 and YUKI OGASAWARA1 1Department of Analytical Biochemistry, Meiji Pharmaceutical University, Kiyose, Tokyo 204‑8588; 2Department of Genome Biology, Kinki University School of Medicine, Osaka-sayama, Osaka 589-8511, Japan Received August 26, 2014; Accepted May 20, 2015 DOI: 10.3892/ol.2015.3352 Abstract. Cisplatin is a commonly used drug in combination treatment of various cancers, including lung cancer. Cisplatin chemotherapy. However, various malignant tumors frequently is a commonly used drug for combination chemotherapy (1). acquire resistance to cisplatin. Arsenic trioxide (ATO) has Although cisplatin is a potent anticancer drug, various been approved as a chemotherapeutic drug for the treatment malignant tumors frequently acquire resistance to cisplatin, of acute promyelocytic leukemia, and the combination of limiting the clinical application of this agent (2,3). ATO and cisplatin has been revealed to demonstrate syner- Arsenite is a toxic metalloid that is widely distributed in gistic effects in ovarian and small cell lung cancer cells. Thus, the environment (4). Despite the toxicity, arsenic-containing it was hypothesized that ATO may also be active against compounds have been used in traditional Chinese medicine cisplatin-resistant non-small cell lung cancer (NSCLC) for >2,000 years (5). In addition, arsenic trioxide (ATO) has PC-9/CDDP and PC-14/CDDP cells. The present study been approved in numerous countries for the treatment of also evaluated the effects of ATO on the cisplatin-sensitive acute promyelocytic leukemia (APL) (6). -

Enhancement of the Activity of Phenoxodiol by Cisplatin in Prostate Cancer Cells
British Journal of Cancer (2009) 100, 649 – 655 & 2009 Cancer Research UK All rights reserved 0007 – 0920/09 $32.00 www.bjcancer.com Enhancement of the activity of phenoxodiol by cisplatin in prostate cancer cells 1 1,2 *,1,2 RAC McPherson , PT Galettis and PL de Souza 1 2 Cancer Pharmacology and Therapeutics Laboratory, Department of Medical Oncology, St George Hospital, Sydney, New South Wales, Australia; Faculty of Medicine, University of NSW, Sydney, New South Wales, Australia Phenoxodiol is a novel isoflav-3-ene, currently undergoing clinical trials, that has a broad in vitro activity against a number of human cancer cell lines. Phenoxodiol alone inhibited DU145 and PC3 in a dose- and time-dependent manner with IC50 values of 8±1 and 38±9 mM, respectively. The combination of phenoxodiol and cisplatin was synergistic in DU145, and additive in PC3, as assessed by the Chou–Talalay method. Carboplatin was also synergistic in combination with phenoxodiol in DU145 cells. The activity of the phenoxodiol and cisplatin combination was confirmed in vivo using a DU145 xenograft model in nude mice. Pharmacokinetic data from these mice suggest that the mechanism of synergy may occur through a pharmacodynamic mechanism. An intracellular cisplatin accumulation assay showed a 35% (Po0.05) increase in the uptake of cisplatin when it was combined in a ratio of 1 mM:5mM phenoxodiol, resulting in a 300% (P 0.05) increase in DNA adducts. Taken together, our results suggest that phenoxodiol has o interesting properties that make combination therapy with cisplatin or carboplatin appealing. British Journal of Cancer (2009) 100, 649–655. -

A Phase I Study of Estramustine, Weekly Docetaxel, and Carboplatin Chemotherapy in Patients with Hormone-Refractory Prostate Cancer
284 Vol. 11, 284–289, January 1, 2005 Clinical Cancer Research A Phase I Study of Estramustine, Weekly Docetaxel, and Carboplatin Chemotherapy in Patients with Hormone-Refractory Prostate Cancer William K. Oh,1 Elizabeth Hagmann,1 docetaxel is 43 mg/m2 combined with estramustine and Judith Manola,2 Daniel J. George,1 carboplatin. PSA declines were seen at every dose level. Timothy D. Gilligan,1 Joseph O. Jacobson,4 Matthew R. Smith,3 Donald S. Kaufman,3 and INTRODUCTION Philip W. Kantoff 1 Prostate cancer remains the second leading cause of cancer 1Lank Center for Genitourinary Oncology, Department of Medical death in men in the United States (1). Although initially Oncology and 2Department of Biostatistical Science, Dana-Farber responsive to androgen deprivation therapy, prostate cancer Cancer Institute; 3Department of Medical Oncology, Massachusetts almost always becomes refractory to hormonal manipulation (2) 4 General Hospital Cancer Center, Boston, Massachusetts; and North Mitoxantrone chemotherapy combined with corticosteroids Shore Cancer Center, Peabody, Massachusetts provides palliative benefit in the management of symptomatic disease, but no improvement in survival (3, 4). Phase I and II ABSTRACT trials have shown that the combination of docetaxel and Purpose: To define the maximal tolerated dose, safety, estramustine is effective and well tolerated in patients with and efficacy of docetaxel, carboplatin, and estramustine in hormone refractory prostate cancer (HRPC; refs. 5–9). Two patients with hormone-refractory prostate cancer (HRPC). recently reported large phase III trials showed that docetaxel Methods: Patients with HRPC received docetaxel for 3 combined with either prednisone or estramustine was associated weeks, followed by a rest week. -

Head and Neck Cancer
Chemotherapy Protocol HEAD AND NECK CANCER CISPLATIN-FLUOROURACIL Regimen • Head and Neck Cancer – Cisplatin-Fluorouracil Indication • Neoadjuvant and palliative treatment of squamous cell carcinoma of the head and neck Toxicity Drug Adverse Effect Cisplatin Neuropathy, nephrotoxicity, ototoxicity Fluorouracil Diarrhoea, stomatitis The adverse effects listed are not exhaustive. Please refer to the relevant Summary of Product Characteristics for full details. Monitoring Drugs • FBC, LFTs and U&Es prior to each cycle • Patients with complete or partial dihydropyrimidine dehydrogenase (DPD) deficiency are at increased risk of severe and fatal toxicity during treatment with fluorouracil. All patients should be tested for DPD deficiency before initiation (cycle 1) to minimise the risk of these reactions Dose Modifications The dose modifications listed are for haematological, liver and renal function and drug specific toxicities only. Dose adjustments may be necessary for other toxicities as well. In principle all dose reductions due to adverse drug reactions should not be re-escalated in subsequent cycles without consultant approval. It is also a general rule for chemotherapy that if a third dose reduction is necessary treatment should be stopped. Please discuss all dose reductions / delays with the relevant consultant before prescribing, if appropriate. The approach may be different depending on the clinical circumstances. Version 1.1 (November 2020) Page 1 of 6 Head and Neck – Cisplatin-Fluorouracil Haematological Consider blood transfusion if patient symptomatic of anaemia or has a haemoglobin of less than 8g/dL. Criteria Eligible Level Neutrophils 1.5x10 9/L or greater Platelets 100x10 9/L or greater Defer treatment for 7 days if the neutrophil count is less than 1.5x10 9/L and / or the platelet count is less than 100x10 9/L. -

Multiple Myeloma
MULTIPLE MYELOMA ARSENIC TRIOXIDE Arsenic trioxide 0.25 mg/kg/day IV* Monday - Friday of Weeks 1 and 2** *Administer over 1 hour; **Administer Monday - Friday (5 days per week) during the first 2 weeks of each 4 week cycle. Repeat cycles every 28 days. NOTE: Ensure that serum electrolytes are assessed and corrected, particularly potassium and magnesium, prior to start of treatment, and maintain these values throughout the cycle. Avoid medication known to prolong the QTc interval. Obtain a 12-lead ECG prior to the first dose and ensure that the QTc interval is not greater than 460 msec. Reference: Hussein MA, et al. Br J Haematol 2004;125:470 - 6. BORTEZOMIB Bortezomib 1.3 mg/m2 IVB Days 1, 4, 8 and 11 Repeat cycle every 21 days to a maximum of 8 cycles. NOTE: Patients with progressive disease after 2 cycles or stable diseases after 4 cycles were able to receive dexamethasone 20 mg on the day of and the day after bortezomib. Reference: Richardson PG, et al. N Engl J Med 2003;348:2609 – 17. BORTEZOMIB – DOXORUBICIN - DEXAMETHASONE Bortezomib 1.3 mg/m2 IVB Days 1, 4, 8 and 11 Dexamethasone 40 mg /day PO See below (cycle dependent) Doxorubicin 9 mg/m2/day IV Days 1 - 4 Repeat cycle every 21 days for 4 cycles. NOTE: Dexamethasone dosing: 40 mg PO/day was administered on days 1 – 4, 8 – 11, and 15 – 18 of cycle 1 and on days 1 – 4 of cycles 2 – 4. Concurrent bisphosphonate therapy, gastric protection, erythropoietin and Pneumocystis carinii prophylaxis were given. -
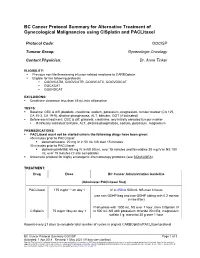
GOCISP Protocol
BC Cancer Protocol Summary for Alternative Treatment of Gynecological Malignancies using CISplatin and PACLitaxel Protocol Code: GOCISP Tumour Group: Gynecologic Oncology Contact Physician: Dr. Anna Tinker ELIGIBILITY: . Previous non-life threatening infusion-related reactions to CARBOplatin . Eligible for the following protocols . GOOVCATM, GOOVCATR, GOOVCATX, GOOVDDCAT . GOCXCAT . GOENDCAT EXCLUSIONS: . Creatinine clearance less than 45 mL/min at baseline TESTS: . Baseline: CBC & diff, platelets, creatinine, sodium, potassium, magnesium, tumour marker (CA 125, CA 15-3, CA 19-9), alkaline phosphatase, ALT, bilirubin, GGT (if indicated) . Before each treatment: CBC & diff, platelets, creatinine, any initially elevated tumour marker . If clinically indicated: bilirubin, ALT, alkaline phosphatase, sodium, potassium, magnesium PREMEDICATIONS: . PACLitaxel must not be started unless the following drugs have been given: 45 minutes prior to PACLItaxel: . dexamethasone 20 mg IV in 50 mL NS over 15 minutes 30 minutes prior to PACLItaxel: . diphenhydrAMINE 50 mg IV in NS 50 mL over 15 minutes and famotidine 20 mg IV in NS 100 mL over 15 minutes (Y-site compatible) . Antiemetic protocol for highly emetogenic chemotherapy protocols (see SCNAUSEA) TREATMENT: Drug Dose BC Cancer Administration Guideline (Administer PACLitaxel first) PACLitaxel 175 mg/m2 * on day 1 IV in 250 to 500 mL NS over 3 hours (use non-DEHP bag and non-DEHP tubing with 0.2 micron in-line filter) Prehydrate with 1000 mL NS over 1 hour, then CISplatin IV CISplatin 75 mg/m2/day on day 1 in 500 mL NS with potassium chloride 20 mEq, magnesium sulfate 1 g, mannitol 30 g over 1 hour Repeat every 21 days to complete total number of cycles in original CARBOplatin/PACLitaxel protocol BC Cancer Protocol Summary GOCISP Page 1 of 3 Activated: 1 Apr 2018 Revised: 1 May 2021 (IV bag size clarified) Warning: The information contained in these documents are a statement of consensus of BC Cancer professionals regarding their views of currently accepted approaches to treatment.