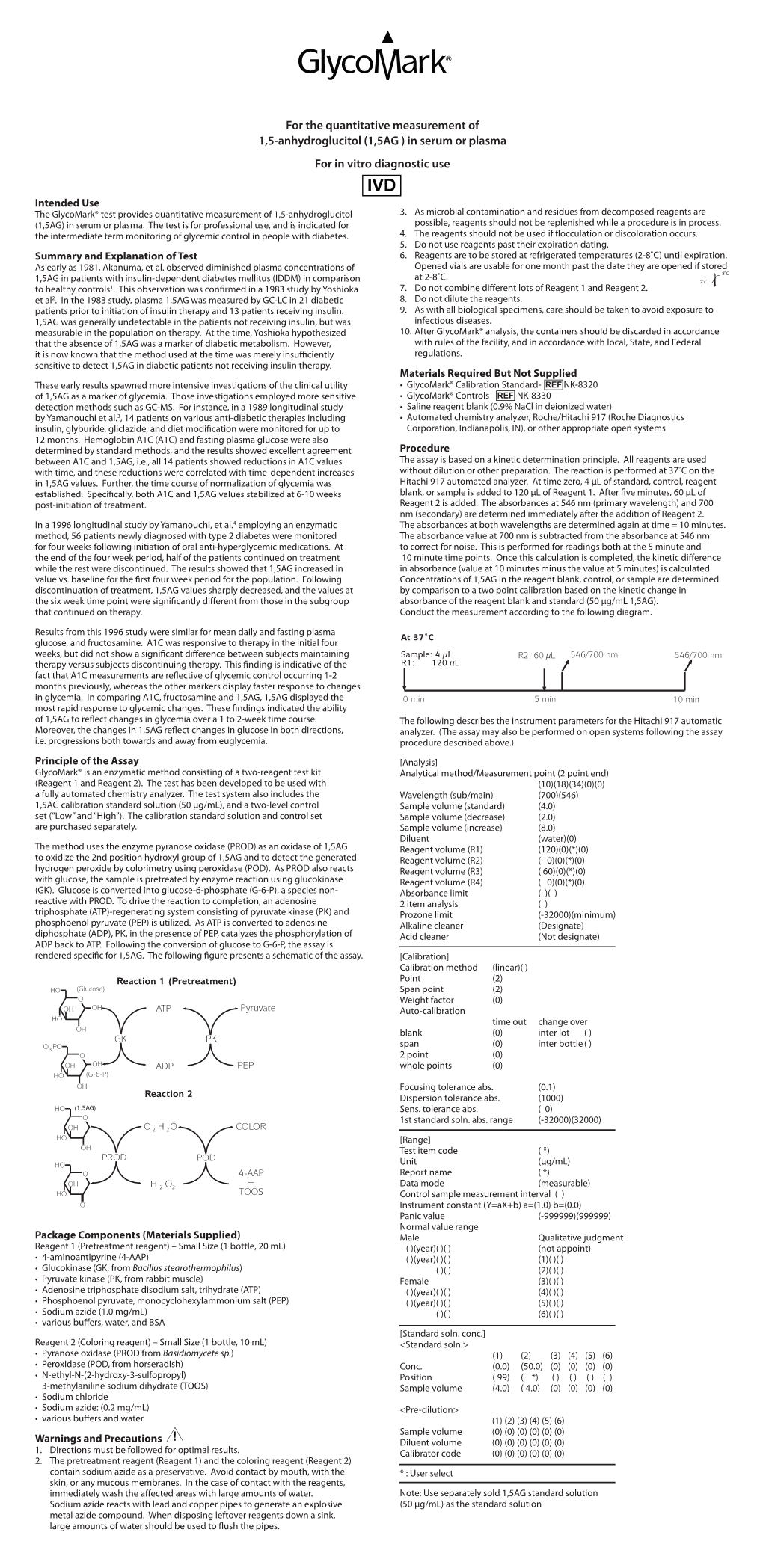
For the Quantitative Measurement of 1,5-Anhydroglucitol (1,5AG ) in Serum Or Plasma for in Vitro Diagnostic Use
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Yangxin Tongmai Formula Ameliorates Impaired Glucose Tolerance in Children with Graves’ Disease Through Upregulation of the Insulin Receptor Levels
Acta Pharmacologica Sinica (2018) 39: 923–929 © 2018 CPS and SIMM All rights reserved 1671-4083/18 www.nature.com/aps Article Yangxin Tongmai Formula ameliorates impaired glucose tolerance in children with Graves’ disease through upregulation of the insulin receptor levels Yan-hong LUO1, Min ZHU1, Dong-gang WANG1, Yu-sheng YANG1, Tao TAN2, Hua ZHU2, Jian-feng HE1, * 1Children’s Hospital Chongqing Medical University, Chongqing 400000, China; 2Department of Surgery, Davis Heart and Lung Research Institute, the Ohio State University Wexner Medical Center, Columbus, OH 43210, USA Abstract Graves’ disease (GD) is the leading cause of hyperthyroidism, and the majority of GD patients eventually develop disorders of glucose handling, which further affects their quality of life. Yangxin Tongmai formula (YTF) is modified from a famous formula of traditional Chinese medicine for the treatment of cardiovascular diseases. In this study we investigated the potential effects of YTF in the treatment of pediatric GD patients with impaired glucose tolerance. Forty pediatric GD patients and 20 healthy children were recruited for this clinical study. Based on the glucose tolerance, the GD patients were divided into two groups: 20 patients displayed impaired glucose tolerance, while the other 20 patients displayed normal glucose tolerance. YTF was orally administered for 60 days. YTF administration significantly ameliorated the abnormal glucose tolerance and insulin sensitivity in the GD patients with impaired glucose tolerance. To determine the molecular mechanisms of this observation, the number of plasma insulin receptors was determined by ELISA. Before treatment, the fasting and postprandial levels of the insulin receptor were significantly lower in patients with impaired glucose tolerance compared with those in patients with normal glucose tolerance and healthy children. -
Various Method of Glucose Estimation , Gtt and Principal of Carbohydrates Chemistry Test
VARIOUS METHOD OF GLUCOSE ESTIMATION , GTT AND PRINCIPAL OF CARBOHYDRATES CHEMISTRY TEST Subject : Biochemistry Student name : 1)Jignasha Surti. 2)Mitali Rana. 3)Arpita Kataria. 4)Priya Patel. 5)Vipra Patel. Content : • Introduction • Entry of glucose into cell • Blood collection • Method for glucose estimation 1) Enzymatic method 2) Chemical method • Estimation of glucose in urine sample • Estimation of glucose in CSF sample • Normal values • GTT • Principle of carbohydrate chemistry INTRODUCTION •Glucose is a monosaccharide. • It is central molecule in carbohydrate metabolism. • Stored as glycogen in liver and skeletal muscle. Entry of glucose into the cell Two specific transport system are used : • Insulin –independent transport system: •Carrier mediated uptake of glucose •Not dependent on insulin. •Present in hepatocytes, erythrocytes & brain. • Insulin dependent transport system : • Present in Skeletal muscle. ENTRY OF GLUCOSE INTO CELL : Insulin - dependent GLUT 4 –mediated • Insulin/GLUT4 is not only pathway. • cellular uptake of glucose into muscle and adipose tissue (40%). Insulin – independent glucose disposal (60%) - GLUT 1 -3 in the Brain, Placenta, Kidney -SGLT 1 and 2 (sodium glucose symporter) -intestinal epithelium, kidney. Blood collection for glucose estimation : •Fluoride containing vials are used. •Fluoride inhibit glycolysis by inhibiting enolase enzyme. •2-phosphoglycerate is converted into phosphoenol pyruvate by enzyme enolase by removing one water molecule. FLUORIDE •Fluoride irreversibly inhibit enolase there by stop the whole glycolysis. •Therefor, fluoride is added to blood during estimation of blood sugar. Normal ranges : [Reference: American Diabetes Association(ADA) ] Random blood glucose test : • It is a blood sugar test taken from a non-fasting subject. • Normal range is 79-160 mg/dl. -
Glucose Transporter 2 Concentrations in Hyper- and Hypothyroid Rat Livers
285 Glucose transporter 2 concentrations in hyper- and hypothyroid rat livers T Mokuno, K Uchimura, R Hayashi, N Hayakawa, M Makino, M Nagata, H Kakizawa, Y Sawai, M Kotake, N Oda, A Nakai, A Nagasaka and M Itoh Department of Internal Medicine, Fujita Health University School of Medicine, Toyoake, Aichi 470–1192, Japan (Requests for offprints should be addressed to A Nagasaka) Abstract The deterioration of glucose metabolism frequently An oral glucose tolerance test revealed an oxyhyper- observed in hyperthyroidism may be due in part to glycemic curve (impaired glucose tolerance) in hyperthy- increased gluconeogenesis in the liver and glucose efflux roid rats (n=7) and a flattened curve in hypothyroid rats through hepatocyte plasma membranes. Glucose trans- (n=7). GLUT 2 levels in hepatocyte plasma membranes porter 2 (GLUT 2), a facilitative glucose transporter were significantly increased in hyperthyroid rats and were localized to the liver and pancreas, may play a role in this not decreased in hypothyroid rats compared with euthy- distorted glucose metabolism. roid rats. The same results were obtained with a densito- We examined changes in the levels of GLUT 2 in livers metric assay. These findings suggest that changes in the from rats with -thyroxine-induced hyperthyroidism or liver GLUT 2 concentration may contribute to abnormal methimazole-induced hypothyroidism by using Western glucose metabolism in thyroid disorders. blotting to detect GLUT 2. Journal of Endocrinology (1999) 160, 285–289 Introduction by glucose transporter 2 (GLUT 2), a facilitative glucose transporter (Elbrink & Bihler 1975). Thus, GLUT 2, The homeostasis of glucose metabolism is maintained by which is localized to the liver and pancreas (Fukumoto many factors, including intestinal glucose absorption, liver et al. -

Glycomark Compendium of Evidence
GlycoMark Compendium of Evidence Glycemic Control No. Title Institute Department First Author Citation 1 Variations of 1-Deoxyglucose (1,5-Anhydroglucitol) National Defense Pediatrics Yoshioka S Clin.Chem 1983; 29(7): 1396-1398 content in patients with insulin-dependent diabetes Medical College mellitus 2 Reduction and recovery of plasma 1,5-anhydro-D-glucitol University of Teikyo Internal Medicine Yamanouchi T Diabetes 1987; 36(6): 709-715 level in diabetes mellitus 3 Reduction of plasma 1,5-AG(1,5-Anhydroglucitol) levels in Saitama Medical Internal Medicine Kawazu S J. Japan Diab. Soc. 1988; 31(8): diabetes mellitus and renal glycosuria School 715-718 4 Urinary excretion of 1,5-Anhydro-D-glucitol Institute for Diabetes Akanuma Y Diabetologia 1988; 31: 831-835 accompanying glucose excretion in diabetic patients Care and Research, Asahi Life Foundation 5 Reduction of plasma 1,5-anhydroglucitol concentration in University of Teikyo Internal Medicine Yamanouchi T Diabetologia 1988; 31:41-45 diabetic patients 6 Plasma 1,5-anhydro-D-glucitol as new clinical marker of University of Teikyo Internal Medicine Yamanouchi T Diabetes 1989; 38(6): 723-729 glycemic control in NIDDM patients 7 Clinical significance of serum 1,5-anhydroglucitol University of Teikyo Internal Medicine Yamanouchi T J. Japan Diab. Soc. 1990; 33(1): measurements in diabetes mellitus 41-48 8 Serum 1,5-Anhydroglucitol level in patients with non- Jichi Medical School Endocrinology and Iwamoto Y Korea Japan Symp.D.M. 1991; insulin-dependent diabetes Mellitus Metabolism 117-120 9 1,5-anhydroglucitol as a marker of glycemic control in Jichi Medical School Endocrinology and Ohwada N Clinical Endocrinology 1991; diabetes mellitus. -

Glucose Variability Before and After Treatment of a Patient with Graves’ Disease Complicated by Diabetes Mellitus: Assessment by Continuous Glucose Monitoring
Endocrine Journal 2014 ORIGINAL Advance Publication doi: 10.1507/endocrj. EJ13-0410 Glucose variability before and after treatment of a patient with Graves’ disease complicated by diabetes mellitus: Assessment by continuous glucose monitoring Keiichi Torimoto, Yosuke Okada, Tadashi Arao, Hiroko Mori, Sunao Yamamoto, Manabu Narisawa, Akira Kurozumi and Yoshiya Tanaka First Department of Internal Medicine, School of Medicine, University of Occupational and Environmental Health, Kitakyushyu 807-8555, Japan Abstract. A 48-year-old woman was diagnosed and treated for Graves’ disease (GD) in 1999 but she discontinued treatment at her own discretion. In 2011, she was admitted to a local hospital for management of thyrotoxic crisis. Treatment with propylthiouracil, iodide potassium (KI), and prednisolone (PSL) was started, which resulted in improvement of the general condition. PSL and KI were discontinued before she was transferred to our hospital. At the local hospital, fasting plasma glucose (FPG) was 212 mg/dL and hemoglobin A1c concentration was 11.2%; intensive insulin therapy had been instituted. Upon admission to our hospital, FPG level was 122 mg/dL, but insulin secretion was compromised, suggesting aggravation of thyroid function and deterioration of glycemic control. The FPG level increased to 173 mg/dL; continuous glucose monitoring (CGM) identified dawn phenomenon at approximately 0400 h. Resumption of KI resulted in improvement of FPG and disappearance of the dawn phenomenon, as assessed by CGM. These results indicate that in patients with compromised insulin secretion, hyperthyroidism can induce elevation of not only postprandial blood glucose, but also FPG level due to the dawn phenomenon and that the dawn phenomenon can be alleviated with improvement in thyroid function. -

Us 2018 / 0305689 A1
US 20180305689A1 ( 19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2018 /0305689 A1 Sætrom et al. ( 43 ) Pub . Date: Oct. 25 , 2018 ( 54 ) SARNA COMPOSITIONS AND METHODS OF plication No . 62 /150 , 895 , filed on Apr. 22 , 2015 , USE provisional application No . 62/ 150 ,904 , filed on Apr. 22 , 2015 , provisional application No. 62 / 150 , 908 , (71 ) Applicant: MINA THERAPEUTICS LIMITED , filed on Apr. 22 , 2015 , provisional application No. LONDON (GB ) 62 / 150 , 900 , filed on Apr. 22 , 2015 . (72 ) Inventors : Pål Sætrom , Trondheim (NO ) ; Endre Publication Classification Bakken Stovner , Trondheim (NO ) (51 ) Int . CI. C12N 15 / 113 (2006 .01 ) (21 ) Appl. No. : 15 /568 , 046 (52 ) U . S . CI. (22 ) PCT Filed : Apr. 21 , 2016 CPC .. .. .. C12N 15 / 113 ( 2013 .01 ) ; C12N 2310 / 34 ( 2013. 01 ) ; C12N 2310 /14 (2013 . 01 ) ; C12N ( 86 ) PCT No .: PCT/ GB2016 /051116 2310 / 11 (2013 .01 ) $ 371 ( c ) ( 1 ) , ( 2 ) Date : Oct . 20 , 2017 (57 ) ABSTRACT The invention relates to oligonucleotides , e . g . , saRNAS Related U . S . Application Data useful in upregulating the expression of a target gene and (60 ) Provisional application No . 62 / 150 ,892 , filed on Apr. therapeutic compositions comprising such oligonucleotides . 22 , 2015 , provisional application No . 62 / 150 ,893 , Methods of using the oligonucleotides and the therapeutic filed on Apr. 22 , 2015 , provisional application No . compositions are also provided . 62 / 150 ,897 , filed on Apr. 22 , 2015 , provisional ap Specification includes a Sequence Listing . SARNA sense strand (Fessenger 3 ' SARNA antisense strand (Guide ) Mathew, Si Target antisense RNA transcript, e . g . NAT Target Coding strand Gene Transcription start site ( T55 ) TY{ { ? ? Targeted Target transcript , e . -

Glucose and Insulin Metabolism in Patients with Hyperthyroidism Due to Graves' Disease
Nagoya J. Med. Sci. 57. 61 - 68, 1994 GLUCOSE AND INSULIN METABOLISM IN PATIENTS WITH HYPERTHYROIDISM DUE TO GRAVES' DISEASE TOSHIKI MANO, AKITOSHI KAwAKUBO, and MASAHIRO YAMAMOTO Department of Internal Medicine, Anjo Kosei Hospital, Anjo, Aichi 446, Japan ABSTRACT To clarify the impairment of carbohydrate metabolism in hyperthyroidism, we performed the oral glucose tolerance test (OGTT) and glucagon tolerance test in ten patients with hyperthyroidism due to Graves' dis ease (GD) and in ten normal subjects. During OGTT, glucose and insulin values in the GD patients were twice as high as those in the normals. The ratio of cumulative net plasma glucose [:LPG (0-120 minutes)] and insulin [:LIRI (0-120 minutes)] was 0.83±0.14 and 1.14±0.25 in the GD patients and normals, respec tively. During the glucagon tolerance test, plasma glucose showed lower peaks in the GD patients than in the normals. C-peptide reached a peak value at 6 min in the GD patients and at 10 min in the normals. Cyclic AMP response in the GD patients was three times greater than that in the normals. A smaller insulinogenic index and a smaller :LPGI:LIRI ratio in the GD patients suggest that the secre tion of insulin in GD patients does not meet the demand despite the higher insulin values observed during OGTT. Greater response of cAMP, smaller and earlier peaks of C-peptide and smaller response of glucose to glucagon in the GD patients may suggest a rapid insulin turnover and a reduction of glycogen storage in the liver with hyperthyroidism. -

Glucose Variability Before and After Treatment of a Patient with Graves’ Disease Complicated by Diabetes Mellitus: Assessment by Continuous Glucose Monitoring
Endocrine Journal 2014, 61 (4), 321-328 ORIGINAL Glucose variability before and after treatment of a patient with Graves’ disease complicated by diabetes mellitus: Assessment by continuous glucose monitoring Keiichi Torimoto, Yosuke Okada, Tadashi Arao, Hiroko Mori, Sunao Yamamoto, Manabu Narisawa, Akira Kurozumi and Yoshiya Tanaka First Department of Internal Medicine, School of Medicine, University of Occupational and Environmental Health, Kitakyushyu 807-8555, Japan Abstract. A 48-year-old woman was diagnosed and treated for Graves’ disease (GD) in 1999 but she discontinued treatment at her own discretion. In 2011, she was admitted to a local hospital for management of thyrotoxic crisis. Treatment with propylthiouracil, iodide potassium (KI), and prednisolone (PSL) was started, which resulted in improvement of the general condition. PSL and KI were discontinued before she was transferred to our hospital. At the local hospital, fasting plasma glucose (FPG) was 212 mg/dL and hemoglobin A1c concentration was 11.2%; intensive insulin therapy had been instituted. Upon admission to our hospital, FPG level was 122 mg/dL, but insulin secretion was compromised, suggesting aggravation of thyroid function and deterioration of glycemic control. The FPG level increased to 173 mg/dL; continuous glucose monitoring (CGM) identified dawn phenomenon at approximately 0400 h. Resumption of KI resulted in improvement of FPG and disappearance of the dawn phenomenon, as assessed by CGM. These results indicate that in patients with compromised insulin secretion, hyperthyroidism can induce elevation of not only postprandial blood glucose, but also FPG level due to the dawn phenomenon and that the dawn phenomenon can be alleviated with improvement in thyroid function. -

Oxyhyperglycemiaと 糖尿 病 との関 係 に つ い て 第1報 胃切除者における
Oxyhyperglycemiaと 糖 尿 病 と の 関 係 に つ い て 第1報 胃切 除 者 にお け る検討* 大 西 泰 憲** 著 者 は 胃切 除 者 に お け る ブ ドウ糖 お よびtolbutamide I. 緒 言 負 荷 時 の 血 糖 な らび に そ の さい の血 中 イ ン ス リン の動 態 胃切 除 者 で は,糖 の経 口負 荷 後血 糖 が 初 期 著 明 に上 昇, に つ い て,胃 切 除 前 後 に お け る変 化 お よび術 後 の 経 過 年 つ づ い て急 速 に下 降 し,Lawrence1)(1936)の い うoxy- 数 との 関 係 を検 討 し,胃 切 除 者 に み ら れ るoxyhyper- hyperglycemia型 の 耐 糖 曲 線 を 示 す こ とが 特 徴 と され て glycemiaと 糖 尿 病 との 関 係 につ い て2,3の 考 察 を試 み い る.胃 切 除 者 に お い て この よ うな耐糖 曲 線 の み られ る た. 理 由 と して,Lawrence以 来 一 般 に,負 荷 した 糖 が 急 速 に腸 管 に移 行 し,そ の 吸 収 が 促 進 され る こ とに よ る もの II. 研 究 対 象 な ら び に 方 法 で,糖 代 謝 の 異常 で は な い と理 解 さ れ て お り2~4) ,従 来 1. 研 究 対 象 胃切 除 者 に お け る糖 負荷 後 の血 糖 の変 動 につ い て の研 究 対 象 は,1964年 よ り1967年 の間 に,岡 山大 学 医 学 部 第 は,主 と して 胃切 除 後 の ダ ン ピ ン グ症 候 群 に 関 係 す る も 一 内 科 に お い て ,ブ ドウ糖 負 荷 試 験(以 下GTTと 略 す) の で5~7),糖尿 病 との 関連 を検 討 した もの は ほ とん ど み を行 な った 胃切 除 者(原 疾 患 は 全 例 胃 ま た は十 二 指 腸 潰 あ た ら ない. -

Hba1c and Glycated Albumin Levels Are High in Gastrectomized Subjects with Iron-Deficiency Anemia
Available online at www.annclinlabsci.org 52 Annals of Clinical & Laboratory Science, vol. 47, no. 1, 2017 HbA1c and Glycated Albumin Levels Are High in Gastrectomized Subjects with Iron-Deficiency Anemia Shinya Inada1 and Masafumi Koga2 1Department of Internal Medicine, Kawanishi City Hospital and 2Department of Internal Medicine, Hakuhokai Central Hospital, Hyogo, Japan Abstract. We report that glycated albumin (GA) is higher relative to HbA1c in non-diabetic, gastrecto- mized subjects without anemia, and thus is a sign of oxyhyperglycemia. It is known that gastrectomized subjects are prone to iron-deficiency anemia (IDA), and that the HbA1c levels of subjects with IDAare falsely high. In the present study, the HbA1c and GA levels of gastrectomized subjects with IDA were compared with gastrectomized subjects without anemia. Seven non-diabetic gastrectomized subjects with IDA were enrolled in the present study. Twenty-eight non-diabetic gastrectomized subjects without anemia matched with the subjects with IDA in terms of age, gender, and body mass index were used as the con- trols. Although there were no significant differences in fasting plasma glucose and OGTT 2-hour plasma glucose (2-h PG) between the two groups, the HbA1c and GA levels in gastrectomized subjects with IDA were significantly higher than the controls. For all of the gastrectomized subjects (n=35), ferritin exhibited a significant negative correlation with HbA1c and GA, and a significant positive correlation with2-hPG. In addition, the HbA1c and GA levels exhibited a significant negative correlation with the mean corpuscular hemoglobin and hemoglobin. The HbA1c and GA levels in gastrectomized subjects withIDA were sig- nificantly higher than those in controls. -

Treatment with Hypoglycemia: A-Glucosidase Inhibitor for Severe
Endocrine Journal 2000, 47 (4), 437-442 Treatment with a-Glucosidase Inhibitor for Severe Reactive Hypoglycemia: A Case Report ** SHINICHI TENO *, , YUKO NAKAJIMA-UTO*, **, KAZUTAKA NAGAI*, MADOKA SHIMIZU-SAITOH*, HIROYUKI OZU *, YASUE OMORI* AND TAKAO TAKIZAWA* * Saitamaken Saiseikai Kurihashi Hospital , Kouemon Gotanda 714-6, Kurihashi-cho, Kita-katsushika-gun, Saitama 349-1105, Japan **Diabetes Center , Tokyo Women's Medical University School of Medicine, Kawada-cho 8-1, Shinjuku-ku, Tokyo 162-8666, Japan Abstract. Gastrectomy or vagotomy may result in reactive hypoglycemia, which, in some cases, can reduce the plasma glucose levels to 30-40 mg/dl due to rapid digestion and absorption of food, especially carbohydrates. It also occurs sometimes in patients on hemodialysis, where it is a potentially lethal complication. Because insulin has a longer half-life due to lack of renal degradation, hypoglycemia can be induced by insulin in patients with renal failure. We treated a patient with frequent episodes of severe hypoglycemia, that were sometimes accompanied by con- vulsions. He had undergone total gastrectomy 8 years before and had been maintained on hemodialysis for 3 years. Hyperinsulinemia caused by oxyhyperglycemia associated with post-gastrectomy led to severe hypoglycemia in this patient because of the lack of renal insulin degradation. Since nutritional treatment did not successfully manage his reactive hypoglycemia, an a-glucosidase inhibitor, acarbose, was administered to treat his oxyhyperglycemia. This therapy was very effective and he has not had any recurrence of reactive hypoglycemia since the initiation of the therapy. Key words: Alimentary hypoglycemia, Post-gastrectomy, Chronic renal failure, a-Glucosidase inhibitor, Counter- regulatory hormone (Endocrine Journal 47: 437-442, 2000) SYMPTOMS of hypoglycemia, such as weakness, lized in the kidneys and liver. -

(12) Patent Application Publication (10) Pub. No.: US 2009/0042279 A1 YAMAKOSH Et Al
US 20090042279A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2009/0042279 A1 YAMAKOSH et al. (43) Pub. Date: Feb. 12, 2009 (54) METHOD OF DETECTING MILD IMPAIRED Related U.S. Application Data St.RE.N E OR INSULIN (62) Division of application No. 10/509,120, filed on Nov. 29, 2004, now Pat. No. 7,452,687, filed as application No. PCT/JP03/03771 on Mar 27, 2003. (75) Inventors: Masaru YAMAKOSHI, (30) Foreign Application Priority Data Mishima-shi (JP); Takuji Kouzuma, Mishima-shi (JP) Mar. 22, 2002 (JP) ................................... 2002-97.121 Publication Classification (51) Int. Cl. Correspondence Address: CI2P I/00 (2006.01) BRCH STEWARTKOLASCH & BRCH (52) U.S. Cl. ........................................................ 435/262 PO BOX 747 FALLS CHURCH, VA 22040-0747 (US) (57) ABSTRACT It is intended to provide a noninvasive method of conve niently detecting mild impaired glucose tolerance and/or (73) Assignee: Asahi Kasei Pharma Corporation, insulin hyposecretion at the early stage with the use of an Tokyo (JP) enzyme. Namely, mild impaired glucose tolerance and/or insulin hyposecretion at the early stage are detected by quan tifying myoinositol Secreted into the urine before loading glucose and after loading glucose for a definite period of time (21) Appl. No.: 12/248,876 with the use of a reagent and comparing the increase (or the increase ratio) in the myoinositol content thus measured with a characteristic level which has been preliminarily deter (22) Filed: Oct. 9, 2008 mined in normal Subjects. 200 y = 3.4753x + 477.1 1000 g 3. 2 600 2. 400 A 200 -50 O 50 OO 50 200 A myo-inositol (ug/mg Cre) Patent Application Publication Feb.