Lymphangioma in Patients with Pulmonary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recurrent Targetoid Hemosiderotic Hemangioma in a 26-Year-Old Man
CASE REPORT Recurrent Targetoid Hemosiderotic Hemangioma in a 26-Year-Old Man LT Sarah Broski Gendernalik, DO, MC (FS), USN LT James D. Gendernalik, DO, MC (FS), USN A 26-year-old previously healthy man presented with a 6-mm violaceous papule that had a surrounding 1.5-cm annular, nonblanching, erythematous halo on the right-sided flank. The man reported the lesion had been recurring for 4 to 5 years, flaring every 4 to 5 months and then slowly disap - pearing until the cycle recurred. Targetoid hemosiderotic hemangioma was clinically diagnosed. The lesion was removed by means of elliptical excision and the condition resolved. The authors discuss the clinical appearance, his - tology, and etiology of targetoid hemosiderotic heman - giomas. J Am Osteopath Assoc . 2011;111(2);117-118 argetoid hemosiderotic hemangiomas (THHs) are a com - Tmonly misdiagnosed presentation encountered in the primary care setting. In the present case report, we aim to pro - Figure. A 6-mm violaceous papule with a surrounding 1.5-cm annular, nonblanching, erythematous halo in a 26-year-old man. vide general practitioners with an understanding of the clin - ical appearance, pathology, and prognosis of THH. Report of Case A 26-year-old previously healthy man presented to our primary around it and itched and burned each time it developed. The care clinic with a 6-mm violaceous papule with a surrounding lesion faded completely to normal-appearing skin between 1.5-cm annular, nonblanching, erythematous halo on the right- episodes, without evidence of a papule or postinflammatory sided flank ( Figure ). The patient stated that the lesion had hyperpigmentation. -

The Health-Related Quality of Life of Sarcoma Patients and Survivors In
Cancers 2020, 12 S1 of S7 Supplementary Materials The Health-Related Quality of Life of Sarcoma Patients and Survivors in Germany—Cross-Sectional Results of A Nationwide Observational Study (PROSa) Martin Eichler, Leopold Hentschel, Stephan Richter, Peter Hohenberger, Bernd Kasper, Dimosthenis Andreou, Daniel Pink, Jens Jakob, Susanne Singer, Robert Grützmann, Stephen Fung, Eva Wardelmann, Karin Arndt, Vitali Heidt, Christine Hofbauer, Marius Fried, Verena I. Gaidzik, Karl Verpoort, Marit Ahrens, Jürgen Weitz, Klaus-Dieter Schaser, Martin Bornhäuser, Jochen Schmitt, Markus K. Schuler and the PROSa study group Includes Entities We included sarcomas according to the following WHO classification. - Fletcher CDM, World Health Organization, International Agency for Research on Cancer, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. 468 p. (World Health Organization classification of tumours). - Kurman RJ, International Agency for Research on Cancer, World Health Organization, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: International Agency for Research on Cancer; 2014. 307 p. (World Health Organization classification of tumours). - Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. - World Health Organization, Swerdlow SH, International Agency for Research on Cancer, editors. WHO classification of tumours of haematopoietic and lymphoid tissues: [... reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25 - 27, 2007]. 4. ed. -

The Nutrition and Food Web Archive Medical Terminology Book
The Nutrition and Food Web Archive Medical Terminology Book www.nafwa. -

Vascular Tumors and Malformations of the Orbit
14 Vascular Tumors Kaan Gündüz and Zeynel A. Karcioglu ascular tumors and malformations of the orbit VIII related antigen (v,w,f), CV141 (endothelium, comprise an important group of orbital space- mesothelium, and squamous cells), and VEGFR-3 Voccupying lesions. Reviews indicate that vas- (channels, neovascular endothelium). None of the cell cular lesions account for 6.2 to 12.0% of all histopatho- markers is absolutely specific in its application; a com- logically documented orbital space-occupying lesions bination is recommended in difficult cases. CD31 is (Table 14.1).1–5 There is ultrastructural and immuno- the most often used endothelial cell marker, with pos- histochemical evidence that capillary and cavernous itive membrane staining pattern in over 90% of cap- hemangiomas, lymphangioma, and other vascular le- illary hemangiomas, cavernous hemangiomas, and an- sions are of different nosologic origins, yet in many giosarcomas; CD34 is expressed only in about 50% of patients these entities coexist. Hence, some prefer to endothelial cell tumors. Lymphangioma pattern, on use a single umbrella term, “vascular hamartomatous the other hand, is negative with CD31 and CD34, lesions” to identify these masses, with the qualifica- but, it is positive with VEGFR-3. VEGFR-3 expression tion that, in a given case, one tissue element may pre- is also seen in Kaposi sarcoma and in neovascular dominate.6 For example, an “infantile hemangioma” endothelium. In hemangiopericytomas, the tumor may contain a few caverns or intertwined abnormal cells are typically positive for vimentin and CD34 and blood vessels, but its predominating component is negative for markers of endothelia (factor VIII, CD31, usually capillary hemangioma. -

Benign Hemangiomas
TUMORS OF BLOOD VESSELS CHARLES F. GESCHICKTER, M.D. (From tke Surgical Palkological Laboratory, Department of Surgery, Johns Hopkins Hospital and University) AND LOUISA E. KEASBEY, M.D. (Lancaster Gcaeral Hospital, Lancuster, Pennsylvania) Tumors of the blood vessels are perhaps as common as any form of neoplasm occurring in the human body. The greatest number of these lesions are benign angiomas of the body surfaces, small elevated red areas which remain without symptoms throughout life and are not subjected to treatment. Larger tumors of this type which undergb active growth after birth or which are situated about the face or oral cavity, where they constitute cosmetic defects, are more often the object of surgical removal. The majority of the vascular tumors clinically or pathologically studied fall into this latter group. Benign angiomas of similar pathologic nature occur in all of the internal viscera but are most common in the liver, where they are disclosed usually at autopsy. Angiomas of the bone, muscle, and the central nervous system are of less common occurrence, but, because of the symptoms produced, a higher percentage are available for study. Malignant lesions of the blood vessels are far more rare than was formerly supposed. An occasional angioma may metastasize following trauma or after repeated recurrences, but less than 1per cent of benign angiomas subjected to treatment fall into this group. I Primarily ma- lignant tumors of the vascular system-angiosarcomas-are equally rare. The pathological criteria for these growths have never been ade- quately established, and there is no general agreement as to this par- ticular form of tumor. -

About Soft Tissue Sarcoma Overview and Types
cancer.org | 1.800.227.2345 About Soft Tissue Sarcoma Overview and Types If you've been diagnosed with soft tissue sarcoma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Soft Tissue Sarcoma? Research and Statistics See the latest estimates for new cases of soft tissue sarcoma and deaths in the US and what research is currently being done. ● Key Statistics for Soft Tissue Sarcomas ● What's New in Soft Tissue Sarcoma Research? What Is a Soft Tissue Sarcoma? Cancer starts when cells start to grow out of control. Cells in nearly any part of the body can become cancer and can spread to other areas. To learn more about how cancers start and spread, see What Is Cancer?1 There are many types of soft tissue tumors, and not all of them are cancerous. Many benign tumors are found in soft tissues. The word benign means they're not cancer. These tumors can't spread to other parts of the body. Some soft tissue tumors behave 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 in ways between a cancer and a non-cancer. These are called intermediate soft tissue tumors. When the word sarcoma is part of the name of a disease, it means the tumor is malignant (cancer).A sarcoma is a type of cancer that starts in tissues like bone or muscle. Bone and soft tissue sarcomas are the main types of sarcoma. Soft tissue sarcomas can develop in soft tissues like fat, muscle, nerves, fibrous tissues, blood vessels, or deep skin tissues. -
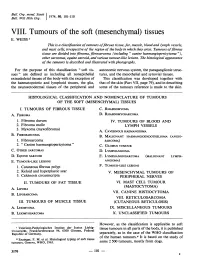
Mesenchymal) Tissues E
Bull. Org. mond. San 11974,) 50, 101-110 Bull. Wid Hith Org.j VIII. Tumours of the soft (mesenchymal) tissues E. WEISS 1 This is a classification oftumours offibrous tissue, fat, muscle, blood and lymph vessels, and mast cells, irrespective of the region of the body in which they arise. Tumours offibrous tissue are divided into fibroma, fibrosarcoma (including " canine haemangiopericytoma "), other sarcomas, equine sarcoid, and various tumour-like lesions. The histological appearance of the tamours is described and illustrated with photographs. For the purpose of this classification " soft tis- autonomic nervous system, the paraganglionic struc- sues" are defined as including all nonepithelial tures, and the mesothelial and synovial tissues. extraskeletal tissues of the body with the exception of This classification was developed together with the haematopoietic and lymphoid tissues, the glia, that of the skin (Part VII, page 79), and in describing the neuroectodermal tissues of the peripheral and some of the tumours reference is made to the skin. HISTOLOGICAL CLASSIFICATION AND NOMENCLATURE OF TUMOURS OF THE SOFT (MESENCHYMAL) TISSUES I. TUMOURS OF FIBROUS TISSUE C. RHABDOMYOMA A. FIBROMA D. RHABDOMYOSARCOMA 1. Fibroma durum IV. TUMOURS OF BLOOD AND 2. Fibroma molle LYMPH VESSELS 3. Myxoma (myxofibroma) A. CAVERNOUS HAEMANGIOMA B. FIBROSARCOMA B. MALIGNANT HAEMANGIOENDOTHELIOMA (ANGIO- 1. Fibrosarcoma SARCOMA) 2. " Canine haemangiopericytoma" C. GLOMUS TUMOUR C. OTHER SARCOMAS D. LYMPHANGIOMA D. EQUINE SARCOID E. LYMPHANGIOSARCOMA (MALIGNANT LYMPH- E. TUMOUR-LIKE LESIONS ANGIOMA) 1. Cutaneous fibrous polyp F. TUMOUR-LIKE LESIONS 2. Keloid and hyperplastic scar V. MESENCHYMAL TUMOURS OF 3. Calcinosis circumscripta PERIPHERAL NERVES II. TUMOURS OF FAT TISSUE VI. -

A Case of Lymphangioleiomyomatosis Originated in the Pelvic Cavity
J Gynecol Oncol Vol. 19, No. 3:195-198, September 2008 DOI:10.3802/jgo.2008.19.3.195 Case Report A case of lymphangioleiomyomatosis originated in the pelvic cavity Jung-Mi Han, Kyung-Hee Lee, Sung-Joo Kim, Chae-Chun Rhim, Young-Han Park, Jung-Bae Kang, Sun-Young Jeon1 Departments of Obstetrics and Gynecology, 1Pathology, Hallym University Medical College, Anyang, Korea Lymphangioleiomyomatosis is a rare disease that is characterized by proliferation of abnormal smooth muscle-like cells, especially that which occurs in the pulmonary parenchyme. It primarily affects women of child-bearing age. The majority of primary lymphangioleiomyomatosis occurs in the lung, but there are a few reports of extrapulmonary cases. We experienced a rare case of lymphangioleiomyomatosis which originated in the pelvic cavity (in the posterior portion of the uterus), and report with brief review of literatures. Key Words: Lymphangioleiomyomatosis, Pelvis, Uterus INTRODUCTION hypervascular tumor between the uterus and the right ovary, and two small myomas about 2 cm in size (Fig. 1). Under the Lymphangioleiomyomatosis is a very rare disease which impression of ovarian malignancy she had admitted for shows typical features of abnormal smooth muscle cell further evaluation including MRI. Her initial serum CA-125 proliferation and which develops in females during the level was 26.7 U/ml and CA 19-9 level was below 2 U/ml, and reproductive period.1,2 The majority cases of this disease other hematologic findings were all within the normal range. primarily occur in the lungs, but extrapulmonary regions such Magnetic resonance imaging study of the abdomen-pelvis as the pelvis and retroperitoneal spaces are occasionally demonstrated an approximately 4.0×5.0×4.0 cm sized tumor primary sites. -

Lymphangioleiomyomatosis and Tuberous Sclerosis: Where Is the Border?
Eur Respir J, 1996, 9, 399–401 Copyright ERS Journals Ltd 1996 DOI: 10.1183/09031936.96.09030399 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 EDITORIAL Lymphangioleiomyomatosis and tuberous sclerosis: Where is the border? F. Bonetti*, P. Chiodera** Pulmonary lymphangioleiomyomatosis (PLAM) is a The key to addressing this unresolved question seems rare disease, characterized by an abnormal proliferation to be the definition of the diagnostic criteria of TS. The of smooth muscle throughout the lung; it occurs exclu- classical Vogt triad (seizures, mental retardation and facial sively in women, generally of reproductive age [1]. The angiofibroma) was the first important attempt to clini- muscle cells proliferating in PLAM show little or no cally define the syndrome. This diagnostic triad was atypia at histological level. Therefore, PLAM has been universally accepted and was, for a long time, consi- considered to be a hamartomatous lesion rather than a dered the hallmark of the disease. Whilst useful for clini- true neoplastic process. However, in spite of the bland cians, this approach led to a delay in the recognition of cytological features, the disease causes a progressive other diagnostic signs of TS, particularly the presence structural remodelling of the lung, leading to serious and classification of visceral lesions, such as angio- impairment of pulmonary function. Whilst survival curves myolipoma, so characteristic in this hereditary disease of now seem better than previously believed and hormonal autosomal dominant transmission. With the accumula- treatment has been introduced with encouraging results tion of knowledge on TS and the introduction of new [2], some patients progress to a condition necessitating diagnostic techniques, the Vogt triad has lost much of lung transplantation. -

Differential Diagnostic Considerations
Radiology Case Reports Volume 10, Issue 2, 2015 Chylothorax in a patient with metastatic Kaposi sarcoma: Differential diagnostic considerations Ryan Alexander, DO; Magda Rizer, DO; William Burke, MD; and Lawrence Ciment, MD Kaposi sarcoma (KS) is a low-grade mesenchymal tumor involving blood and lymphatic vessels. There are four types, based on clinical presentation: classic, endemic (Africana), iatrogenic (typically, involving renal allograft recipients), and AIDS-associated (epidemic). Kaposi’s sarcoma-associated herpes virus in- fection has been linked along with other factors to the development of KS. The Kaposi’s sarcoma- associated herpes virus interacts and encodes for numerous molecular proteins that play a role in the pathogenesis of KS, including latency-associated nuclear antigen, viral G protein-coupled receptor, viral FLICE inhibitory protein, and viral IL-6. KS primarily affects the skin and causes disseminated disease in a variety of organs. Involvement of visceral organs other than the lining of the alimentary tract is ex- tremely rare. While the chylous pleural effusions of KS may resemble other pulmonary diseases (includ- ing lymphangioma, lymphangectasis, and lymphangioleiomyomatosis) with chylous effusions at thoracic CT, differentiating features may allow for more prompt diagnosis and treatment. The presumptive diag- nosis of AIDS-related pulmonary KS is often clinical. A tissue diagnosis is not required to establish the diagnosis of pulmonary KS. There are a variety of causes of chylothorax. The primary finding is a near- water-attenuating pleural effusion. The secondary findings of chylothorax can help differentiate the etiology. Introduction be diagnosed on CT or MRI. The CT finding of chylous Chylothorax is a relatively uncommon cause of pleural effusions is typically a large unilateral effusion of water effusion (1). -

Head and Neck Kaposi Sarcoma: Clinicopathological Analysis of 11 Cases
Head and Neck Pathology https://doi.org/10.1007/s12105-018-0902-x ORIGINAL PAPER Head and Neck Kaposi Sarcoma: Clinicopathological Analysis of 11 Cases Abbas Agaimy1 · Sarina K. Mueller2 · Thomas Harrer3 · Sebastian Bauer4 · Lester D. R. Thompson5 Received: 24 January 2018 / Accepted: 26 February 2018 © Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract Kaposi sarcoma (KS) of the head and neck area is uncommon with limited published case series. Our routine and consulta- tion files were reviewed for histologically and immunohistochemically proven KS affecting any cutaneous or mucosal head and neck site. Ten males and one female aged 42–78 years (median, 51 years; mean, 52 years) were retrieved. Eight patients were HIV-positive and three were HIV-negative. The affected sites were skin (n = 5), oral/oropharyngeal mucosa (n = 5), and lymph nodes (n = 3) in variable combination. The ear (pinna and external auditory canal) was affected in two cases; both were HIV-negative. Multifocal non-head and neck KS was reported in 50% of patients. At last follow-up (12–94 months; median, 46 months), most of patients were either KS-free (n = 8) or had ongoing remission under systemic maintenance therapy (n = 2). One patient was alive with KS (poor compliance). Histopathological evaluation showed classical features of KS. One case was predominantly sarcomatoid with prominent inflammation mimicking undifferentiated sarcoma. Immunohisto- chemistry showed consistent expression of CD31, CD34, ERG, D2-40 and HHV8 in all cases. This is one of the few series devoted to head and neck KS showing high prevalence of HIV-positivity, but also unusual presentations in HIV-negative patients with primary origin in the skin of the ear and the auditory canal. -

2016 Essentials of Dermatopathology Slide Library Handout Book
2016 Essentials of Dermatopathology Slide Library Handout Book April 8-10, 2016 JW Marriott Houston Downtown Houston, TX USA CASE #01 -- SLIDE #01 Diagnosis: Nodular fasciitis Case Summary: 12 year old male with a rapidly growing temple mass. Present for 4 weeks. Nodular fasciitis is a self-limited pseudosarcomatous proliferation that may cause clinical alarm due to its rapid growth. It is most common in young adults but occurs across a wide age range. This lesion is typically 3-5 cm and composed of bland fibroblasts and myofibroblasts without significant cytologic atypia arranged in a loose storiform pattern with areas of extravasated red blood cells. Mitoses may be numerous, but atypical mitotic figures are absent. Nodular fasciitis is a benign process, and recurrence is very rare (1%). Recent work has shown that the MYH9-USP6 gene fusion is present in approximately 90% of cases, and molecular techniques to show USP6 gene rearrangement may be a helpful ancillary tool in difficult cases or on small biopsy samples. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors, 5th edition. Mosby Elsevier. 2008. Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011 Oct;91(10):1427-33. Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013 Jul;463(1):97-8. CONTRIBUTED BY KAREN FRITCHIE, MD 1 CASE #02 -- SLIDE #02 Diagnosis: Cellular fibrous histiocytoma Case Summary: 12 year old female with wrist mass.