Coexistence of Lymphangioma Circumscriptum and Angiokeratoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recurrent Targetoid Hemosiderotic Hemangioma in a 26-Year-Old Man
CASE REPORT Recurrent Targetoid Hemosiderotic Hemangioma in a 26-Year-Old Man LT Sarah Broski Gendernalik, DO, MC (FS), USN LT James D. Gendernalik, DO, MC (FS), USN A 26-year-old previously healthy man presented with a 6-mm violaceous papule that had a surrounding 1.5-cm annular, nonblanching, erythematous halo on the right-sided flank. The man reported the lesion had been recurring for 4 to 5 years, flaring every 4 to 5 months and then slowly disap - pearing until the cycle recurred. Targetoid hemosiderotic hemangioma was clinically diagnosed. The lesion was removed by means of elliptical excision and the condition resolved. The authors discuss the clinical appearance, his - tology, and etiology of targetoid hemosiderotic heman - giomas. J Am Osteopath Assoc . 2011;111(2);117-118 argetoid hemosiderotic hemangiomas (THHs) are a com - Tmonly misdiagnosed presentation encountered in the primary care setting. In the present case report, we aim to pro - Figure. A 6-mm violaceous papule with a surrounding 1.5-cm annular, nonblanching, erythematous halo in a 26-year-old man. vide general practitioners with an understanding of the clin - ical appearance, pathology, and prognosis of THH. Report of Case A 26-year-old previously healthy man presented to our primary around it and itched and burned each time it developed. The care clinic with a 6-mm violaceous papule with a surrounding lesion faded completely to normal-appearing skin between 1.5-cm annular, nonblanching, erythematous halo on the right- episodes, without evidence of a papule or postinflammatory sided flank ( Figure ). The patient stated that the lesion had hyperpigmentation. -

Angiokeratoma of the Scrotum (Fordyce Type) Associated with Angiokeratoma of the Oral Cavity
208 Letters to the Editor anti-thyroperoxidas e antibody in addition to, or, less Yamada A. Antineutrophil cytoplasmic autoantibody- likely, instead of MPO-ANCA cannot be excluded. positive crescentric glomerulonephritis associated with thi- amazole therapy. Nephron 1996; 74: 734–735. Vesiculo-bullous SLE has been reported to respond 6. Cooper D. Antithyroid drugs. N Engl J Med 1984; 311: to dapsone (15). However, in our patient, an early 1353–1362. aggressive treatment with steroid pulse therapy and 7. Yung RL, Richardson BC. Drug-induced lupus. Rheum plasmapheresis was mandatory because of her life- Dis Clin North Am 1994; 20: 61–86. threatening clinical condition. The contributory factors, 8. Hess E. Drug-related lupus. N Engl J Med 1988; 318: 1460–1462. such as an environmental trigger or an immunological 9. Sato-Matsumura KC, Koizumi H, Matsumura T, factor, for the presence of a serious illness in this patient Takahashi T, Adachi K, Ohkawara A. Lupus eryth- remain to be elucidated. The mechanism by which ematosus-like syndrome induced by thiamazole and methimazole induces SLE-like reactions is unclear. propylthiouracil. J Dermatol 1994; 21: 501–507. 10. Wing SS, Fantus IG. Adverse immunologic eVects of antithyroid drugs. Can Med Assoc J 1987; 136: 121–127. 11. Condon C, Phelan M, Lyons JF. Penicillamine-induced REFERENCES type II bullous systemic lupus erythematosus. Br J Dermatol 1997; 136: 474–475. 1. Alarcon-Segovia D. Drug induced lupus syndromes. Mayo 12. Stankus S, Johnson N. Propylthiouracil-induced hyper- Clin Proc 1969; 44: 664–681.2. sensitivity vasculitis presenting as respiratory failure. Chest 2. Cush JJ, Goldings EA. -

Angiokeratoma of the Scrotum (Fordyce)
Keio Journal of Medicine Vol. 1, No. 1, January, 1952 ANGIOKERATOMA OF THE SCROTUM (FORDYCE) MASAKATSU IZAKI Department of Dermatology, School of Medicine, Keio University Since Fordyce, in 1896, first described a case of angiokeratoma of the scrotum, many authors have reported and discussed about this dermatosis. However the classification and the nomenclature of this skin disease still remain in a state of confusion. Recently I had a chance to see the report of Robinson and Tasker (1946)(14), discussing the nomenclature of this condition, which held my attention considerably. In this paper I wish to report statistical observation concerning the incidences of this dermatosis among Japanese males, and histopathological studies made in 5 cases of this condition. STATISTICALOBSERVATION It must be first pointed out that this study was made along with the statistical study on angioma senile and same persons were examined in both dermatosis (ref. Studies on Senile Changes in the Skin I. Statistical Observation; Journal of the Keio Medical Society Vol. 28, No. 2, p. 59, 1951). The statistics was handled by the small sampling method. Totals of persons examined were 1552 males. Their ages varied from 16 to 84 years, divided into seven groups: i.e. the late teen-agers (16-20), persons of the third decade (21-30), of the fourth decade (31-40), of the fifth decade (41-50), of the sixth decade (51-60), of the seventh decade (61-70) and a group of persons over 71 years of age. The number of persons and the incidence of this condition in each group are summarized briefly in Table 1. -

Vascular Tumors and Malformations of the Orbit
14 Vascular Tumors Kaan Gündüz and Zeynel A. Karcioglu ascular tumors and malformations of the orbit VIII related antigen (v,w,f), CV141 (endothelium, comprise an important group of orbital space- mesothelium, and squamous cells), and VEGFR-3 Voccupying lesions. Reviews indicate that vas- (channels, neovascular endothelium). None of the cell cular lesions account for 6.2 to 12.0% of all histopatho- markers is absolutely specific in its application; a com- logically documented orbital space-occupying lesions bination is recommended in difficult cases. CD31 is (Table 14.1).1–5 There is ultrastructural and immuno- the most often used endothelial cell marker, with pos- histochemical evidence that capillary and cavernous itive membrane staining pattern in over 90% of cap- hemangiomas, lymphangioma, and other vascular le- illary hemangiomas, cavernous hemangiomas, and an- sions are of different nosologic origins, yet in many giosarcomas; CD34 is expressed only in about 50% of patients these entities coexist. Hence, some prefer to endothelial cell tumors. Lymphangioma pattern, on use a single umbrella term, “vascular hamartomatous the other hand, is negative with CD31 and CD34, lesions” to identify these masses, with the qualifica- but, it is positive with VEGFR-3. VEGFR-3 expression tion that, in a given case, one tissue element may pre- is also seen in Kaposi sarcoma and in neovascular dominate.6 For example, an “infantile hemangioma” endothelium. In hemangiopericytomas, the tumor may contain a few caverns or intertwined abnormal cells are typically positive for vimentin and CD34 and blood vessels, but its predominating component is negative for markers of endothelia (factor VIII, CD31, usually capillary hemangioma. -

Benign Hemangiomas
TUMORS OF BLOOD VESSELS CHARLES F. GESCHICKTER, M.D. (From tke Surgical Palkological Laboratory, Department of Surgery, Johns Hopkins Hospital and University) AND LOUISA E. KEASBEY, M.D. (Lancaster Gcaeral Hospital, Lancuster, Pennsylvania) Tumors of the blood vessels are perhaps as common as any form of neoplasm occurring in the human body. The greatest number of these lesions are benign angiomas of the body surfaces, small elevated red areas which remain without symptoms throughout life and are not subjected to treatment. Larger tumors of this type which undergb active growth after birth or which are situated about the face or oral cavity, where they constitute cosmetic defects, are more often the object of surgical removal. The majority of the vascular tumors clinically or pathologically studied fall into this latter group. Benign angiomas of similar pathologic nature occur in all of the internal viscera but are most common in the liver, where they are disclosed usually at autopsy. Angiomas of the bone, muscle, and the central nervous system are of less common occurrence, but, because of the symptoms produced, a higher percentage are available for study. Malignant lesions of the blood vessels are far more rare than was formerly supposed. An occasional angioma may metastasize following trauma or after repeated recurrences, but less than 1per cent of benign angiomas subjected to treatment fall into this group. I Primarily ma- lignant tumors of the vascular system-angiosarcomas-are equally rare. The pathological criteria for these growths have never been ade- quately established, and there is no general agreement as to this par- ticular form of tumor. -

Vascular Malformations, Skeletal Deformities Including Macrodactyly, Embryonic Veins
1.) Give a general classification and nomenclature to think about when evaluating these patients 2.) Share some helpful tips to narrow the differential in a minute or less of interaction 3.) Discuss some helpful imaging recommendations focusing on ultrasound Vascular Anomalies Tumors: Malformations: Hemangiomas: Low flow: Infantile Hemangioma (IH) Capillary malformation (CM) Rapidly involuting congenital hemangioma (RICH) Non-involuting congenital hemangioma (NICH) Venous malformation (VM) Kaposiform Hemangioendothelioma Lymphatic malformation (LM) (KHE) High flow: Arteriovenous malformation (AVM) Tufted Angioma (TA) Combined including syndromic VA. Other rare tumors www.issva.org • 2014 ISSVA classification is now 20 pages long • The key is that the imaging characteristics have not changed • Rapidly growing field • Traditionally, options were always the same – Surgery – Do nothing • With the increase in awareness and research as well as the development of the specialty of vascular anomalies: New Treatment Options Available – Treatment directly linked to diagnosis • Today, we have: – Interventional catheter based therapies – Laser surgery – Ablation technologies: Cryo, RFA, Microwave, etc. – Direct image-guided medications to administer – Infusion medicines – Oral medicines – Surgery- although much less common – Do Nothing- a VERY important alternative • Survey sample of 100 Referred patients – 47% wrong Dx – 35% wrong Tx • 14% wrong Tx with correct Dx • VAC – 14% indeterminate or wrong Dx – only 4% leave with no Tx plan • Important because -
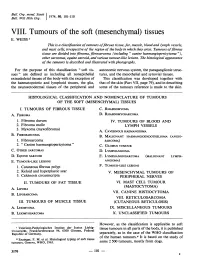
Mesenchymal) Tissues E
Bull. Org. mond. San 11974,) 50, 101-110 Bull. Wid Hith Org.j VIII. Tumours of the soft (mesenchymal) tissues E. WEISS 1 This is a classification oftumours offibrous tissue, fat, muscle, blood and lymph vessels, and mast cells, irrespective of the region of the body in which they arise. Tumours offibrous tissue are divided into fibroma, fibrosarcoma (including " canine haemangiopericytoma "), other sarcomas, equine sarcoid, and various tumour-like lesions. The histological appearance of the tamours is described and illustrated with photographs. For the purpose of this classification " soft tis- autonomic nervous system, the paraganglionic struc- sues" are defined as including all nonepithelial tures, and the mesothelial and synovial tissues. extraskeletal tissues of the body with the exception of This classification was developed together with the haematopoietic and lymphoid tissues, the glia, that of the skin (Part VII, page 79), and in describing the neuroectodermal tissues of the peripheral and some of the tumours reference is made to the skin. HISTOLOGICAL CLASSIFICATION AND NOMENCLATURE OF TUMOURS OF THE SOFT (MESENCHYMAL) TISSUES I. TUMOURS OF FIBROUS TISSUE C. RHABDOMYOMA A. FIBROMA D. RHABDOMYOSARCOMA 1. Fibroma durum IV. TUMOURS OF BLOOD AND 2. Fibroma molle LYMPH VESSELS 3. Myxoma (myxofibroma) A. CAVERNOUS HAEMANGIOMA B. FIBROSARCOMA B. MALIGNANT HAEMANGIOENDOTHELIOMA (ANGIO- 1. Fibrosarcoma SARCOMA) 2. " Canine haemangiopericytoma" C. GLOMUS TUMOUR C. OTHER SARCOMAS D. LYMPHANGIOMA D. EQUINE SARCOID E. LYMPHANGIOSARCOMA (MALIGNANT LYMPH- E. TUMOUR-LIKE LESIONS ANGIOMA) 1. Cutaneous fibrous polyp F. TUMOUR-LIKE LESIONS 2. Keloid and hyperplastic scar V. MESENCHYMAL TUMOURS OF 3. Calcinosis circumscripta PERIPHERAL NERVES II. TUMOURS OF FAT TISSUE VI. -

Head and Neck Kaposi Sarcoma: Clinicopathological Analysis of 11 Cases
Head and Neck Pathology https://doi.org/10.1007/s12105-018-0902-x ORIGINAL PAPER Head and Neck Kaposi Sarcoma: Clinicopathological Analysis of 11 Cases Abbas Agaimy1 · Sarina K. Mueller2 · Thomas Harrer3 · Sebastian Bauer4 · Lester D. R. Thompson5 Received: 24 January 2018 / Accepted: 26 February 2018 © Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract Kaposi sarcoma (KS) of the head and neck area is uncommon with limited published case series. Our routine and consulta- tion files were reviewed for histologically and immunohistochemically proven KS affecting any cutaneous or mucosal head and neck site. Ten males and one female aged 42–78 years (median, 51 years; mean, 52 years) were retrieved. Eight patients were HIV-positive and three were HIV-negative. The affected sites were skin (n = 5), oral/oropharyngeal mucosa (n = 5), and lymph nodes (n = 3) in variable combination. The ear (pinna and external auditory canal) was affected in two cases; both were HIV-negative. Multifocal non-head and neck KS was reported in 50% of patients. At last follow-up (12–94 months; median, 46 months), most of patients were either KS-free (n = 8) or had ongoing remission under systemic maintenance therapy (n = 2). One patient was alive with KS (poor compliance). Histopathological evaluation showed classical features of KS. One case was predominantly sarcomatoid with prominent inflammation mimicking undifferentiated sarcoma. Immunohisto- chemistry showed consistent expression of CD31, CD34, ERG, D2-40 and HHV8 in all cases. This is one of the few series devoted to head and neck KS showing high prevalence of HIV-positivity, but also unusual presentations in HIV-negative patients with primary origin in the skin of the ear and the auditory canal. -

Early Lesions of Kaposi's Sarcoma in Homosexual Men an Ultrastructural Comparison with Other Vascular Proliferations in Skin
Early Lesions of Kaposi's Sarcoma in Homosexual Men An Ultrastructural Comparison With Other Vascular Proliferations in Skin N. SCOTT McNUTT, MD, VAN FLETCHER, MD and From the Departments of Pathology and Dermatology and the Kaposi MARCUS A. CONANT, MD Sarcoma Study Group, Veterans Administration Medical Center, and the University of California, San Francisco, California An aggressive variant of Kaposi's sarcoma (KS) has ap- thelial lining, and had only a few small junctional peared in young homosexual men with evidence of sys- densities between endothelial cells. Some clinically temic immunosuppression. The ultrastructure in biop- aggressive cases of KS also had necrosis of individual sy specimens from 8 KS cases in young homosexual endothelial cells and had prominent cytoplasmic pro- men has been compared with that in biopsy specimens cesses entrapping individual collagen fibers. The be- from 4 KS cases in elderly heterosexuals and with that nign disorders lacked these features. These differences in biopsy specimens from 23 cases of benign vascular in the structure of the small vessels may be of diagnos- disorders of skin. In all cases of KS the small blood ves- tic value in some early cases ofKS. The loss ofdendritic sels lacked a prominent investment of pericytes and pericytes in blood capillaries in KS might relate to the their processes, had a fragmented and often absent telangiectasia which is a prominent feature of the early basal lamina, had frequent discontinuities in the endo- lesions of KS. (Am J Pathol 1983, 111:62-77) A DRAMATIC CHANGE in the epidemiology and patients the disease progresses rapidly, and they die clinical course of the vascular neoplasm called of KS within 1 year, despite standard combination Kaposi's sarcoma (KS) has occurred in the United drug chemotherapy regimens.4 States since 1981. -

Kaposiform Hemangioendothelioma in Tonsil of a Child
Rekhi et al. World Journal of Surgical Oncology 2011, 9:57 http://www.wjso.com/content/9/1/57 WORLD JOURNAL OF SURGICAL ONCOLOGY CASEREPORT Open Access Kaposiform hemangioendothelioma in tonsil of a child associated with cervical lymphangioma: a rare case report Bharat Rekhi1*, Shweta Sethi1, Suyash S Kulkarni2 and Nirmala A Jambhekar1 Abstract Kaposiform hemangioendothelioma (KHE) is an uncommon vascular tumor of intermediate malignant potential, usually occurs in the extremities and retroperitoneum of infants and is characterized by its association with lymphangiomatosis and Kasabach-Merritt phenomenenon (KMP) in certain cases. It has rarely been observed in the head and neck region and at times, can present without KMP. Herein, we present an extremely uncommon case of KHE occurring in tonsil of a child, associated with a neck swelling, but unassociated with KMP. A 2-year-old male child referred to us with history of sore throat, dyspnoea and right-sided neck swelling off and on, since birth, was clinicoradiologically diagnosed with recurrent tonsillitis, including right sided peritonsillar abscess, for which he underwent right-sided tonsillectomy, elsewhere. Histopathological sections from the excised tonsillar mass were reviewed and showed a tumor composed of irregular, infiltrating lobules of spindle cells arranged in kaposiform architecture with slit-like, crescentic vessels. The cells displayed focal lumen formation containing red blood cells (RBCs), along with platelet thrombi and eosinophilic hyaline bodies. In addition, there were discrete foci of several dilated lymphatic vessels containing lymph and lymphocytes. On immunohistochemistry (IHC), spindle cells were diffusely positive for CD34, focally for CD31 and smooth muscle actin (SMA), the latter marker was mostly expressed around the blood vessels. -

Angiokeratoma.Pdf
Classification of vascular tumors/nevi Vascular tumors mainly of infancy and childhood • Hemangioma of infancy. • Congenital hemangioma. • Miliary hemangiomatosis of infancy. • Spindle cell hemangioma. • Kaposiform hemangioendothelioma. • Tufted angioma. • Sinusoidal hemagioma. Vascular malformation - Capillary: • Salmon patch. • Potr-wine stain. • Nevus anemicus. - Mixed vascular malformation: • Reticulate vascular nevus. • Klipple ternaunay syndrome. • Venous malformation. • Blue rubber bleb nevus syndrome. • Maffucci syndrome. • Zosteriform venous malformation. • Other multiple vascular malformation syndrome. - Lymphatic malformations: • Microcystic/Macrocystic. • Rapid flow (arteriovenous malformation). Angiokeratoma: • Angiokeratoma circumscriptum naeviforme. • Angiokeratoma of Mibelli (or angiokeratoma acroasphyticum digitorum) . • Solitary papular angiokeratoma. • Angiokeratoma of fordyce (or angiokeratoma scroti). • Angiokeratoma corporis diffusum. Cutanous vascular hyperplasia: • Lobular capillary hemangioma. • Epithelioid hemangioma. • Crisoid aneurysm. • Reactive angioendotheliomatosis. • Gromeruloid hemangioma. • Hobnail hemangioma. • Microvascular hemangioma. Benign neoplasm: • Glomus tumors. Malignancy: • Kaposi sarcoma. • Angiosarcoma. • Retiform hemangioendothelioma. Modified classification of the International Society for the Study of Vascular Anomalies (Rome, Italy, 1996) : Tumors: -Hemangiomas: • Superficial (capillary or strawberry haemangioma). • Deep (cavernous haemangioma). • Combined. - Others: • Kaposiform -

Angiokeratoma Corporis Diffusum - a Case Report
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 1 Ver. IV (Jan. 2015), PP 11-13 www.iosrjournals.org Angiokeratoma Corporis Diffusum - A Case Report Dr.S.Nageswaramma1 , Dr. G. Swarna Kumari2, Dr. P. Rajashekar3, Dr. S. Sowmya4, Dr. G. Sirisha5. Department of DVL, Guntur Medical College, DRNTRUHS, Andhra pradesh , India Abstract: Angiokeratoma corporis diffusum, a rare clinical type of angiokeratoma, reported in association with various diseases of which Fabry disease is most common. Fabry disease, an X-linked recessive inborn error of glycosphingolipid metabolism due to deficiency of lysosomal enzyme α- galactosidase A . Clinically the disease is characterized by acroparesthesias, multiple cherry red coloured raised angiomatous hyperkeratotic lesions over trunk, abdomen, sides of buttocks and genitilia. A 27-year-old male born to a consanguineous marriage presents with acroparaesthesias and multiple cherry red and hyperkeratotic lesions over trunk, abdomen, sides of buttocks and genitilia. Histopathological examination is consistent with angiokeratoma and our case was diagnosed as angiokeratoma corporis diffusum. This case is being reported because of its rarity. Keywords: Angiokeratoma corporis difffusum, fabry disease, X-linked recessive disease, α- galactosidase A, acroparaesthesias I. Introduction Fabry disease is an X – linked inborn error of glycosphingolipid metabolism resulting from deficient or absent activity of lysosomal enzyme α-galactosidase A. The enzyme defect leads to accumulation of globotriaosyl ceramide(GL-3) and related glycosphingolipids in plasma and tissue lysosomes. Males are primarily affected, females are carrriers. In classically affected males symptoms begin in childhood with acroparesthesias, burning and tingling pain in upper and lower extremities, hypohidrosis, even anhidrosis.