Abnormalities of Thyroid Function Tests in Hospital Inpatients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Laboratory Procedure Manual
Laboratory Procedure Manual Analyte: Thyroid Stimulating Hormone Matrix: Serum Method: Microparticle Enzyme Immunoassay (MEIA) Method No.: Revised: as performed by: Coulston Foundation Alamogordo, New Mexico Contact: Ms. Love Julian 1-505-434-1725 Important Information for Users Coulston periodically refines these laboratory methods. It is the responsibility of the user to contact the person listed on the title page of each write-up before using the analytical method to find out whether any changes have been made and what revisions, if any, have been incorporated. Thyroid Stimulating Hormone NHANES 2001–2002 Public Release Data Set Information This document details the Lab Protocol for NHANES 2001-2002 data. Two laboratories performed this testing during 2001-2002. In order to maintain confidentiality of the participants the quality control summary statistics and graphs were combined to mask the individual analysis dates from the two laboratories. Methods for both labs are included in this release. The method for Lab18 analyte is included in this file. The method for Lab40 is described in a separate file. A tabular list of the released analytes follows: Lab Number Analyte SAS Label lab18 LBXTSH Thyroid Stimulating Hormone Page 2 of 11 Thyroid Stimulating Hormone NHANES 2001-2002 1. Summary of Test Principle and Clinical Relevance IMx Ultrasensitive hTSH II is a Microparticle Enzyme Immunoassay (MEIA) for the quantitative determination of human thyroid stimulating hormone (hTSH) in serum or plasma on the IMx analyzer. The IMx Ultrasensitive hTSH II assay is based on the MEIA technology. The IMx Ultrasensitive hTSH II reagents and sample are added to the reaction cell in the following sequence: The probe/electrode assembly delivers the sample and anti-hTSH coated microparticles to the incubation well of the reaction cell. -
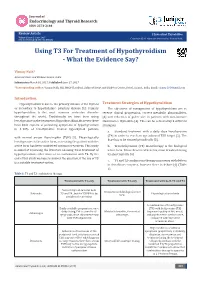
Using T3 for Treatment of Hypothyroidism - What the Evidence Say?
Journal of Endocrinology and Thyroid Research ISSN: 2573-2188 Review Article J Endocrinol Thyroid Res Volume 2 Issue 2- June 2017 Copyright © All rights are reserved by Vismay Naik, DOI: 10.19080/JETR.2017.02.555584 Using T3 For Treatment of Hypothyroidism - What the Evidence Say? Vismay Naik* Ashirvad Heart and Diabetes Centre, India Submission: March 01, 2017; Published: June 27, 2017 *Corresponding author: Vismay Naik, MD, MRCP (London), Ashirvad Heart and Diabetes Centre, Botad, Gujarat, India, Email: Introduction Hypothyroidism is due to the primary disease of the thyroid Treatment Strategies of Hypothyroidism or secondary to hypothalamic- pituitary disease [1]. Primary The objectives of management of hypothyroidism are to hypothyroidism is the most common endocrine disorder reverse clinical progression, correct metabolic abnormalities, throughout the world. Traditionally we have been using [3] and reduction of goiter size in patients with autoimmune levothyroxine in the treatment of hypothyroidism. However, there Hashimoto’s thyroiditis [4]. This can be achieved by 3 different have been reports of persisting symptoms of hypothyroidism strategies: in 5-10% of levothyroxine treated hypothyroid patients a. Standard treatment with a daily dose levothyroxine (T4) in order to reach an age adjusted TSH target [5]. The with normal serum thyrotrophin (TSH) [2]. Physiologically dose has to be titrated periodically [3]. levothyronine is the active form, so treating the patient with the active form has been considered optimum treatment. This study b. Triiodothyronine (T3) monotherapy is the biological is aimed at reviewing the literature on using T3 in treatment of hypothyroidism either alone or in combination with T4. By the its short half-life [6] end of this study we hope to answer the question, if the use of T3 active form. -

A Randomized, Masked Study of Triiodothyronine Plus Thyroxine Administration in Preterm Infants Less Than 28 Weeks of Gestational Age: Hormonal and Clinical Effects
0031-3998/04/5502-0248 PEDIATRIC RESEARCH Vol. 55, No. 2, 2004 Copyright © 2004 International Pediatric Research Foundation, Inc. Printed in U.S.A. A Randomized, Masked Study of Triiodothyronine Plus Thyroxine Administration in Preterm Infants Less Than 28 Weeks of Gestational Age: Hormonal and Clinical Effects PAOLO G. VALERIO, ALEID G. VAN WASSENAER, JAN J.M. DE VIJLDER, AND JOKE H. KOK Department of Neonatology [P.G.V., A.G.v.W., J.H.K.] and Laboratory of Pediatric Endocrinology [J.J.M.d.V.], Academic Medical Center, Emma Children’s Hospital, 1105 AZ Amsterdam, The Netherlands ABSTRACT A randomized, placebo-controlled, masked study was con- effect on cortisol levels. We did not find any effects of T3 or of ducted of the responses of thyroid parameters, cortisol, and the T4 administration on the cardiovascular system. A single injec- cardiovascular system to a single dose of triiodothyronine (T3) tion of T3 (0.5 g/kg) given 22–26 h after birth only leads to a 24 h after birth, followed by a daily dose of thyroxine (T4) during 2-d increase of T3 levels and does not have effects on the Ͻ 6 wk to infants 28 wk gestational age. Thirty-one infants were cardiovascular system. This study does not support the use of T3 assigned to three groups: 1) group A: T3 24 h after birth plus according to our regimen in preterm infants. (Pediatr Res 55: daily T4 during 6 wk; 2) group B: placebo T3 and T4 during 6 wk; 248–253, 2004) and 3) group C: placebo T3 and placebo T4.T4, free T4,T3, free T3, reverse T3, thyroid-stimulating hormone, and cortisol were measured in cord blood and on days 1, 3, 7, 14, 21, 42, and 56. -

Endocrine Abnormalities of the Horse Scott M. Austin, DVM, MS, DACVIM
Endocrine abnormalities of the horse Scott M. Austin, DVM, MS, DACVIM Clinical Associate Professor of Equine Medicine Department of Veterinary Clinical Medicine University of Illinois Summary: Endocrine abnormalities occur frequently in the horse. The clinical presentation of common conditions may have significant overlap resulting in diagnostic confusion. It is important to arrive at an accurate diagnosis, as the successful therapy for endocrine abnormalities is contingent upon the correct diagnosis. Hypothyroidism: Much of the confusion around hypothyroidism is a result of the erroneous association of this condition with obesity, laminitis and infertility. Research that is more recent indicates that hypothyroidism is actually quite rare. In the limited case reports of documented hypothyroidism in horses, the primary clinical signs are lethargy, exercise intolerance, and poor quality haircoat. In horses that had thyroids removed, neither weight gain nor laminitis were seen. Diagnosis: The hypothalamus regulates the production of thyroid hormones through the actions of thyrotropin-releasing hormone (TRH), which stimulates the anterior pituitary gland to release thyroid- stimulating hormone (TSH). TSH then regulates the synthesis and release of thyroid hormones by the thyroid gland. In response to TSH stimulus, triiodothyronine (T3) and thyroxin (T4) are released from the thyroid gland into the bloodstream bound to either thyroglobulins or other proteins such as albumin. T4 has minimal activity and is essentially a prohormone. T3 is the primary active form of the hormone, and only unbound T3 can enter a cell and activate the vital functions attributable to this hormone. The common measurement of total T3 and T4 often provides erroneous values and does not provide a clear picture of thyroid function. -

DHEA Sulfate, and Aging: Contribution of the Dheage Study to a Sociobiomedical Issue
Dehydroepiandrosterone (DHEA), DHEA sulfate, and aging: Contribution of the DHEAge Study to a sociobiomedical issue Etienne-Emile Baulieua,b, Guy Thomasc, Sylvie Legraind, Najiba Lahloue, Marc Rogere, Brigitte Debuiref, Veronique Faucounaug, Laurence Girardh, Marie-Pierre Hervyi, Florence Latourj, Marie-Ce´ line Leaudk, Amina Mokranel, He´ le` ne Pitti-Ferrandim, Christophe Trivallef, Olivier de Lacharrie` ren, Stephanie Nouveaun, Brigitte Rakoto-Arisono, Jean-Claude Souberbiellep, Jocelyne Raisonq, Yves Le Boucr, Agathe Raynaudr, Xavier Girerdq, and Franc¸oise Foretteg,j aInstitut National de la Sante´et de la Recherche Me´dicale Unit 488 and Colle`ge de France, 94276 Le Kremlin-Biceˆtre, France; cInstitut National de la Sante´et de la Recherche Me´dicale Unit 444, Hoˆpital Saint-Antoine, 75012 Paris, France; dHoˆpital Bichat, 75877 Paris, France; eHoˆpital Saint-Vincent de Paul, 75014 Paris, France; fHoˆpital Paul Brousse, 94804 Villejuif, France; gFondation Nationale de Ge´rontologie, 75016 Paris, France; hHoˆpital Charles Foix, 94205 Ivry, France; iHoˆpital de Biceˆtre, 94275 Biceˆtre, France; jHoˆpital Broca, 75013 Paris, France; kCentre Jack-Senet, 75015 Paris, France; lHoˆpital Sainte-Perine, 75016 Paris, France; mObservatoire de l’Age, 75017 Paris, France; nL’Ore´al, 92583 Clichy, France; oInstitut de Sexologie, 75116 Paris, France; pHoˆpital Necker, 75015 Paris, France; qHoˆpital Broussais, 75014 Paris, France; and rHoˆpital Trousseau, 75012 Paris, France Contributed by Etienne-Emile Baulieu, December 23, 1999 The secretion and the blood levels of the adrenal steroid dehydro- number of consumers. Extravagant publicity based on fantasy epiandrosterone (DHEA) and its sulfate ester (DHEAS) decrease pro- (‘‘fountain of youth,’’ ‘‘miracle pill’’) or pseudoscientific asser- foundly with age, and the question is posed whether administration tion (‘‘mother hormone,’’ ‘‘antidote for aging’’) has led to of the steroid to compensate for the decline counteracts defects unfounded radical assertions, from superactivity (‘‘keep young,’’ associated with aging. -
In Vitro Effect of Triiodothyronine on the Cyclic Amp, Progesterone and Testosterone Level in Porcine Theca, Granulosa and Luteal Cells
ENDOCRINE REGULATIONS, Vol. 32, 93 – 98, 1998 93 IN VITRO EFFECT OF TRIIODOTHYRONINE ON THE CYCLIC AMP, PROGESTERONE AND TESTOSTERONE LEVEL IN PORCINE THECA, GRANULOSA AND LUTEAL CELLS E.L. GREGORASZCZUK, J. GALAS Laboratory of Animal Endocrinology and Tissue Culture, Department of Animal Physiology, Institute of Zoology, Jagiellonian University, Krakow, Poland Objective. To investigate the influence of thyroid hormone on steroid production and cAMP accumulation in porcine theca (Tc) and granulosa cells (Gc) isolated from preovulatory follicles as well as in luteal cells isolated during the mid-developing luteal phase. Methods. Granulosa and theca cells separated from pig ovarian follicles and pieces of corpora lutea were cultured in the incubation medium M199 with 5 % calf serum. After the addition of triiodothyronine (T3) and 3-isobutyl-1-methyl xanthine (IBMX) to the culture medium cAMP, progesterone and testosterone were estimated with the aid of specific RIA. Results. T 3 added to the culture media stimulated the steroid secretion and cAMP accumulation in all cell types investigated. In theca cells, T3 alone increased androgen production by 2 fold and the addition of IBMX further augmented the steroidogenesis by 2.2 fold. In granulosa cell culture, IBMX had no effect either on the basal or T3 stimulated progesterone secretion and cAMP accumu- lation. In luteal cell culture, IBMX added alone increased progesterone secretion and cAMP accu- mulation in the same manner as T3. Further augmentation of progesterone secretion (1.3-fold) and cAMP accumulation (1.1-fold) was observed after the addition of IBMX together with T3. Conclusion. The influence of thyroid hormone on cyclic nucleotide release by ovarian cells may suggest the involvement of cAMP-dependent mechanism in the realization of T3 action in ovarian cells. -

Annual Changes in the Concentrations of Free Triiodothyronine, Progesterone and Testosterone in Prepubertal Red Deer (Cervus Elaphus Elaphus) Males and Females
Journal of Animal and Feed Sciences, 24, 2015, 113–117 The Kielanowski Institute of Animal Physiology and Nutrition, PAS, Jabłonna Annual changes in the concentrations of free triiodothyronine, progesterone and testosterone in prepubertal red deer (Cervus elaphus elaphus) males and females J. Kuba1, B. Błaszczyk, T. Stankiewicz and J. Udała West Pomeranian University of Technology in Szczecin, Department of Animal Reproduction Biotechnology and Environmental Hygiene, Dr. Judyma 6, 71-466 Szczecin, Poland KEY WORDS: free triiodothyronine, season, ABSTRACT. The aim of the study was to analyse the annual changes in the puberty, sex, red deer concentration of free triiodothyronine, progesterone and testosterone in the serum of prepubertal red deer males and females. Blood was collected monthly from 8 stags and 8 hinds for a period of one year, beginning in November. Hormone concentrations were determined using an immunofluorescence method (TR-FIA). Monitoring of the duration of the prepubertal period, based on the progesterone concentrations in females and testosterone concentrations in the males, suggested that the prepubertal period ended in September in both Received: 4 March 2015 sexes. The experiment revealed the annual rhythm in free triiodothyronine (FT3) Revised: 18 May 2015 Accepted: 15 June 2015 secretion, with significantly higher concentrations in the winter-spring period in comparison with summer-autumn in both, males (P < 0.01) and females (P < 0.05). The results showed that the season considerably influenced the intensity of FT3 secretion in prepubertal red deer and that the secretion dynamics in both sexes were similar, however, the concentrations in the males 1 Corresponding author: reached higher levels than in the females in each season and across the whole e-mail: [email protected] experiment. -

The Unique Endocrine Milieu of the Fetus
Perspectives The Unique Endocrine Milieu of The Fetus Delbert A. Fisher Department ofPediatrics, University of California, Los Angeles School ofMedicine, Harbor-UCLA Medical Center, Torrance, California 90509 Since the pioneering studies of Jost and colleagues four decades hormone precursor. DHAS is transported to the liver for 16- ago, there has been impressive progress in our understanding of hydroxylation and/or to the placenta, where it is hydrolyzed by the intrauterine endocrine milieu (1). Fetal endocrine physiology a steroid sulfatase and utilized as substrate for placental estrogen differs in many important ways from the endocrinology of post- biosynthesis. DHAS serves as substrate for placental estrone and natal life. It is characterized by a series of unique fetal endocrine estradiol production; 160H-DHAS is the major substrate for organs, by a number of hormones or metabolites uniquely placental estriol synthesis (1-6). Estriol is a hormone unique to prominent in the fetal compartment, by the adaptation of several pregnancy; it is not secreted by the ovary of nonpregnant women. fetal endocrine systems to special intrauterine functions, and by There is evidence that placental chorionic gonadotropin mechanisms to neutralize the biological actions of several potent (hCG) is an important stimulus to fetal adrenal function early hormones critical for normal postnatal development (Table I). in pregnancy; fetal pituitary adrenocorticotropin (ACTH) is es- The following discussion is intended to provide a brief perspective sential for maintenance of fetal zone function by midgestation of this unique environment. (4, 5, 7). Other pro-opiomelanocortin (POMC)-derived pep- tides-alpha-melanocyte-stimulating hormone (a-MSH), cor- Fetal endocrine adaptations ticotropin-like intermediate peptide (CLIP), and f,-endorphin- In several instances, fetal endocrine systems or hormones have seem to have only limited roles (4, 5). -

Thyroid Function Tests WHAT IS the THYROID GLAND? T4 and T3 Circulate Almost Entirely Bound to Specific Transport Proteins
AMERICAN THYROID ASSOCIATION® www.thyroid.org Thyroid Function Tests WHAT IS THE THYROID GLAND? T4 and T3 circulate almost entirely bound to specific transport proteins. If the levels of these transport proteins The thyroid gland is a butterfly-shaped endocrine gland changes, there can be changes in how much bound that is normally located in the lower front of the neck. T4 and T3 is measured. This frequently happens during The thyroid’s job is to make thyroid hormones, which are pregnancy and with the use of birth control pills. The “free” secreted into the blood and then carried to every tissue T4 or T3 is the hormone that is unbound and able to enter in the body. Thyroid hormones help the body use energy, and affect the body tissues. stay warm and keep the brain, heart, muscles, and other organs working as they should. TESTS HOW DOES THE THYROID GLAND FUNCTION? Blood tests to measure these hormones are readily available and widely used, but not all are useful in all situations. Tests The major thyroid hormone secreted by the thyroid to evaluate thyroid function include the following: gland is thyroxine, also called T4 because it contains four iodine atoms. To exert its effects, T4 is converted to TSH TESTS triiodothyronine (T3) by the removal of an iodine atom. This The best way to initially test thyroid function is to occurs mainly in the liver and in certain tissues where T3 measure the TSH level in a blood sample. Changes in acts, such as in the brain. The amount of T4 produced by TSH can serve as an “early warning system” – often the thyroid gland is controlled by another hormone, which occurring before the actual level of thyroid hormones in is made in the pituitary gland located at the base of the the body becomes too high or too low. -

Clinical Applications
HORMONE BALANCE CLINICAL APPLICATIONS © 2014 SpectraCell Laboratories, Inc. All rights reserved. DOC 502 12.14 Visit us at www.spectracell.com or call us at 800.227.LABS (5227) HORMONES 101 Steroid Hormones • Dehydroepiandrosterone sulfate (DHEAS) • Androstenedione • Testosterone • Estradiol (E2) • Estrone (E1) • Estriol (E3) • Progesterone Peptide Hormones • Sex hormone binding globulin (SHBG) • Luteinizing hormone (LH) • Follicle stimulating hormone (FSH) • Prolactin Hormone Biosynthesis Pathway DHEAS → Androstenedione → Testosterone or Estrogens Dehydroepiandrosterone sulfate (DHEAS) DHEA is the most abundant sex hormone in the body, with levels typically around 20 times that of any other steroid hormone. Produced primarily in the adrenal gland, it circulates the body in the form of DHEAS (sulfated form), and it is the major precursor hormone to androstenedione and subsequently estrogen and testosterone. DHEA has important functions unrelated to its role as a precursor to other sex hormones such as enhancing immunity to viruses (by increasing natural killer cell activity), alleviating autoimmune conditions, cancer prevention, bone health, cognitive function (via its role in the calming neurotransmitter GABA) and improving insulin sensitivity (by inhibiting glucose-6-phosphate dehydrogenase, the enzyme responsible for fat accumulation). Levels of DHEAS, which is synthesized through a series of reactions from cholesterol, peak when a person is in their mid 20’s and gradually decline in later decades of life. Increasing DHEAS levels may eventually increase levels of downstream sex hormones (testosterone and estrogen, but not necessarily progesterone) and the clinical effects are similar. In addition, the effects of DHEAS may depend on the levels of other hormones. For example, in premenopausal women, DHEAS seems to have a protective effect against hormone related cancers (breast, ovarian, uterine), while in postmenopausal women, if estrogen levels are low, DHEAS may contribute to growth of rogue cells in hormone sensitive tissues. -

Principles Of, and Pitfalls In, Thyroid Function Tests
JOURNAL OF NUCLEAR MEDICINE 6:853-901, 1965 Principles of, and Pitfalls in, Thyroid Function Tests James C. Sisson, M.D.' Ann Arbor, Michigan INTRODUCTION Thyroid function tests are now readily available to, and widely used by, practitioners of the medical arts. However, proper interpretation of the results of such tests requires an understanding of the physiological processes being evaluated, and how this evaluation is accomplished. It is the purpose of this communication to describe the principles of, and some pitfalls in, the uses of certain well established clinical tests with an em phasis on the vagaries encountered. Not all thyroid function procedures will be reviewed, but only those which are in common usage, and which, by apparent inconsistencies, may puzzle the practitioner. Thyroid diseases will not be discussed in any detail. The various clinical entities of thyroid dysfunction will be discussed only as they affect the function tests, and hyper- and hypothyroidism will be included only as points of reference for the laboratory procedures. Hyperthyroidism may be defined as the state of response of the body tissues to too much thyroid hormone, and, conversely, hypothyroidism occurs when the body tissues function in the presence of too little thyroid hormone. No laboratory procedure now available specifically indicates the existence of hyper- or hypo thyroidism. Of the clinical tests in current usage, the basal metabolic rate (BMR) best reflects the action of thyroid hormones on the body cells. However, many factors other than thyroid hormones are involved in the rate of body metabolism, and the BMR is perforce a nonspecific and frequently an imprecise diagnostic aid in thyroid dysfunction. -

Absence of Acute Cardiac Effect of Triiodothyronine in Isolated, Blood-Perfused Canine Atrium
Absence of Acute Cardiac Effect of Triiodothyronine in Isolated, Blood-perfused Canine Atrium Miyoharu KOBAYASHI, M.D., Yasuyuki FURUKAWA, M.D., and Shigetoshi CHIBA, M.D. SUMMARY Effects of triiodothyronine (T3) on SA node pacemaker activity, atrial contractility and on chronotropic and inotropic responses to nor- epinephrine were investigated, using 9 isolated, blood-perfused dog atrium preparations. T3 (0.001pg-0.1ƒÊg) did not cause a significant direct action injected into the cannulated sinus node artery. When T3 (10pg/ min, 40pg/min, 0.1ƒÊg/min, or 0.4ƒÊg/min) was continuously infused into the sinus node artery, both positive chronotropic and inotropic actions of norepinephrine (0.03ƒÊg-0.3ƒÊg) were not influenced. From these results, it is concluded that T3 has neither acutely direct chronotropic nor inotropic effects, and also T3 does not have an acute ef- fect on responses to norepinephrine in the isolated, blood-perfused canine atrium. Additional Indexing Words: Isolated canine atrium Triiodothyronine Norepinephrine Chronotropic effect Inotropic effect T has been known for many years that clinical manifestations of hyper- thyroidism are similar to those caused by overactivity of the sympathetic nervous system. However, considerable controversy still remains whether the cardiovascular manifestations of hyperthyroidism are due to a direct action of thryroid hormones or due to a sensitization to catecholamines. Cairoli and Crout1) reported that tachycardia in hyperthyroidism was attributed to a direct effect of thyroid hormone on pacemaker cells. Murayama and Goodkind2) reported that the enhanced developed tension of isolated atrial muscle from hyperthyroid guinea pigs was produced by a direct effect of thyroid hormone on the heart.