Laboratory Thyroid Function Testing: Do Abnormalities Always Mean
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Laboratory Procedure Manual
Laboratory Procedure Manual Analyte: Thyroid Stimulating Hormone Matrix: Serum Method: Microparticle Enzyme Immunoassay (MEIA) Method No.: Revised: as performed by: Coulston Foundation Alamogordo, New Mexico Contact: Ms. Love Julian 1-505-434-1725 Important Information for Users Coulston periodically refines these laboratory methods. It is the responsibility of the user to contact the person listed on the title page of each write-up before using the analytical method to find out whether any changes have been made and what revisions, if any, have been incorporated. Thyroid Stimulating Hormone NHANES 2001–2002 Public Release Data Set Information This document details the Lab Protocol for NHANES 2001-2002 data. Two laboratories performed this testing during 2001-2002. In order to maintain confidentiality of the participants the quality control summary statistics and graphs were combined to mask the individual analysis dates from the two laboratories. Methods for both labs are included in this release. The method for Lab18 analyte is included in this file. The method for Lab40 is described in a separate file. A tabular list of the released analytes follows: Lab Number Analyte SAS Label lab18 LBXTSH Thyroid Stimulating Hormone Page 2 of 11 Thyroid Stimulating Hormone NHANES 2001-2002 1. Summary of Test Principle and Clinical Relevance IMx Ultrasensitive hTSH II is a Microparticle Enzyme Immunoassay (MEIA) for the quantitative determination of human thyroid stimulating hormone (hTSH) in serum or plasma on the IMx analyzer. The IMx Ultrasensitive hTSH II assay is based on the MEIA technology. The IMx Ultrasensitive hTSH II reagents and sample are added to the reaction cell in the following sequence: The probe/electrode assembly delivers the sample and anti-hTSH coated microparticles to the incubation well of the reaction cell. -

Thyroid Function Tests (Tfts) | Memorial Sloan Kettering Cancer Center
PATIENT & CAREGIVER EDUCATION Thyroid Function Tests (TFTs) This information explains thyroid function tests (TFTs). Thyroid function tests are blood tests that let your doctor see if you have the right amount of thyroid hormone in your blood. Thyroid Stimulating Hormone (TSH) Thyroid stimulating hormone (TSH) is made and released by a gland in your brain. This hormone stimulates your thyroid to work. TSH levels The level of TSH in your blood shows if your thyroid is too active or not active enough. If you don’t have a thyroid, your TSH level tells your doctor if you’re getting the right dose of thyroid hormone replacement medication. The normal TSH range differs slightly from one lab to another. At Memorial Sloan Kettering (MSK), the normal range is 0.55 milli-international units per liter (mIU/L) to 4.78 mIU/L. Depending on the type of thyroid cancer you have, your doctor may want your TSH to be below the normal range. Talk to your doctor about your TSH levels. You can write down your TSH goal below. Your TSH goal is: _______________________ If your TSH level is low, you’re in a state of hyperthyroidism. This means your thyroid function is too active. If your TSH level is high, you’re in a state of hypothyroidism. This means your thyroid function isn’t active enough. Thyroid Function Tests (TFTs) 1/3 In people without thyroid cancer, the goal is to keep their TSH level within the normal range. In some people with thyroid cancer, the goal is to keep their TSH level below the normal range for the first couple of years after being diagnosed. -

Sp — 001 Sd9900033
-SP — 001 SD9900033 to ei Mansour El Tahir Farah Supervisor: Prof. El Daw Mukhtar Co-supervisor: Assoc, Prof. El Tom Sirag El Bin Khartoum -1997 r 30-36 ,• v -\ :.-- DISCLAIMER Portions of this document may be illegible in electronic image products, Images are produced from the best available original document. Contents Declaration I Acknowledgement , II Abstract English Ill Abstract Arabic V List of Abbreviations VII List of Tables VIII List of Figures X Chapter I Introduction and Literature Review 1 Objectives of the Study 40 Chapter II Patients and Methods 41 Chapter III Results 45 Chapter IV Discussion ; 75 Conclusion 82 Recommendations 84 References 85 Appendices The Questionnaire 101 I would like to declare that all the research work was done by myself. I consulted all the literature included in this study . This work has not been submitted to any other university . The information in this thesis has not been published elsewhere. ifp I would like to express my deep gratitude to my supervisor Professor El Daw Mukhtar whose continued enthusiasm and support had guided and encouraged me throughout the study period . This work would not been possible without the benefit of his generous help and leading advices . I am greatly indebted to Dr. El Tom Sirag El Din for his valuable comments and leading advices , helping me alot during preparation of this thesis . My great thanks to the staff in the diagnostic and research laboratory centre , who gave every possible help during my work . I am greatly appreciating the help that had been provided by all doctors technicians and patients . -

Effect of Metformin on Thyroid Function Tests in Type 2 Diabetic Patients
Iraq J Pharm Vol. 14, No.1, 2014 Effect of metformin on thyroid function tests in type 2 diabetic patients Mohammed N. Abed Department of Pharmacology and Toxicology, College of Pharmacy, University of Mosul, Mosul, Iraq correspondence: [email protected] Received Accepted 14.1.2014 4.3.2014 ABSTRACT Background: Diabetes mellitus (DM) and thyroid disorder appears to be closely related.It has long been recognised that thyroid hormones have marked effects on glucose homeostasis, and although autoimmune thyroid disease is more prevalent in type 1 diabetes as a result of their common origin, in patients with type 2 diabetes the prevalence of hypothyroidism and hyperthyroidism is similar to that of the general population. The present study was conducted to assess the interplay between metformin treatment and thyroid function in type 2 diabetic patients. Methods: A total of 73 diabetic patients were enrolled in this study, they were divided into two groups, the first group included 37 type 2 diabetic patients on metformin therapy, whereas the second group involved 36 type 1 diabetic patients on insulin therapy. Another group involved 35 apparently healthy volunteers were also included in the study as a control group. Blood samples were taken from the patients and controls, then the serum was analyzed for measurement of fasting serum glucose (FSG), total T3, free T3 (FT3), total T4, freeT4 FT4) and TSH using ELFA (Enzyme Linked Fluorescent Assay) technique (minividas). Results: the results showed that there were no significant differences between T3, FT3, FT4 and TSH of the metformin group when compared to the same parameters in the control group. -
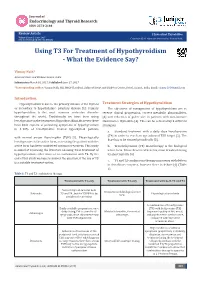
Using T3 for Treatment of Hypothyroidism - What the Evidence Say?
Journal of Endocrinology and Thyroid Research ISSN: 2573-2188 Review Article J Endocrinol Thyroid Res Volume 2 Issue 2- June 2017 Copyright © All rights are reserved by Vismay Naik, DOI: 10.19080/JETR.2017.02.555584 Using T3 For Treatment of Hypothyroidism - What the Evidence Say? Vismay Naik* Ashirvad Heart and Diabetes Centre, India Submission: March 01, 2017; Published: June 27, 2017 *Corresponding author: Vismay Naik, MD, MRCP (London), Ashirvad Heart and Diabetes Centre, Botad, Gujarat, India, Email: Introduction Hypothyroidism is due to the primary disease of the thyroid Treatment Strategies of Hypothyroidism or secondary to hypothalamic- pituitary disease [1]. Primary The objectives of management of hypothyroidism are to hypothyroidism is the most common endocrine disorder reverse clinical progression, correct metabolic abnormalities, throughout the world. Traditionally we have been using [3] and reduction of goiter size in patients with autoimmune levothyroxine in the treatment of hypothyroidism. However, there Hashimoto’s thyroiditis [4]. This can be achieved by 3 different have been reports of persisting symptoms of hypothyroidism strategies: in 5-10% of levothyroxine treated hypothyroid patients a. Standard treatment with a daily dose levothyroxine (T4) in order to reach an age adjusted TSH target [5]. The with normal serum thyrotrophin (TSH) [2]. Physiologically dose has to be titrated periodically [3]. levothyronine is the active form, so treating the patient with the active form has been considered optimum treatment. This study b. Triiodothyronine (T3) monotherapy is the biological is aimed at reviewing the literature on using T3 in treatment of hypothyroidism either alone or in combination with T4. By the its short half-life [6] end of this study we hope to answer the question, if the use of T3 active form. -

A Randomized, Masked Study of Triiodothyronine Plus Thyroxine Administration in Preterm Infants Less Than 28 Weeks of Gestational Age: Hormonal and Clinical Effects
0031-3998/04/5502-0248 PEDIATRIC RESEARCH Vol. 55, No. 2, 2004 Copyright © 2004 International Pediatric Research Foundation, Inc. Printed in U.S.A. A Randomized, Masked Study of Triiodothyronine Plus Thyroxine Administration in Preterm Infants Less Than 28 Weeks of Gestational Age: Hormonal and Clinical Effects PAOLO G. VALERIO, ALEID G. VAN WASSENAER, JAN J.M. DE VIJLDER, AND JOKE H. KOK Department of Neonatology [P.G.V., A.G.v.W., J.H.K.] and Laboratory of Pediatric Endocrinology [J.J.M.d.V.], Academic Medical Center, Emma Children’s Hospital, 1105 AZ Amsterdam, The Netherlands ABSTRACT A randomized, placebo-controlled, masked study was con- effect on cortisol levels. We did not find any effects of T3 or of ducted of the responses of thyroid parameters, cortisol, and the T4 administration on the cardiovascular system. A single injec- cardiovascular system to a single dose of triiodothyronine (T3) tion of T3 (0.5 g/kg) given 22–26 h after birth only leads to a 24 h after birth, followed by a daily dose of thyroxine (T4) during 2-d increase of T3 levels and does not have effects on the Ͻ 6 wk to infants 28 wk gestational age. Thirty-one infants were cardiovascular system. This study does not support the use of T3 assigned to three groups: 1) group A: T3 24 h after birth plus according to our regimen in preterm infants. (Pediatr Res 55: daily T4 during 6 wk; 2) group B: placebo T3 and T4 during 6 wk; 248–253, 2004) and 3) group C: placebo T3 and placebo T4.T4, free T4,T3, free T3, reverse T3, thyroid-stimulating hormone, and cortisol were measured in cord blood and on days 1, 3, 7, 14, 21, 42, and 56. -

Endocrine Abnormalities of the Horse Scott M. Austin, DVM, MS, DACVIM
Endocrine abnormalities of the horse Scott M. Austin, DVM, MS, DACVIM Clinical Associate Professor of Equine Medicine Department of Veterinary Clinical Medicine University of Illinois Summary: Endocrine abnormalities occur frequently in the horse. The clinical presentation of common conditions may have significant overlap resulting in diagnostic confusion. It is important to arrive at an accurate diagnosis, as the successful therapy for endocrine abnormalities is contingent upon the correct diagnosis. Hypothyroidism: Much of the confusion around hypothyroidism is a result of the erroneous association of this condition with obesity, laminitis and infertility. Research that is more recent indicates that hypothyroidism is actually quite rare. In the limited case reports of documented hypothyroidism in horses, the primary clinical signs are lethargy, exercise intolerance, and poor quality haircoat. In horses that had thyroids removed, neither weight gain nor laminitis were seen. Diagnosis: The hypothalamus regulates the production of thyroid hormones through the actions of thyrotropin-releasing hormone (TRH), which stimulates the anterior pituitary gland to release thyroid- stimulating hormone (TSH). TSH then regulates the synthesis and release of thyroid hormones by the thyroid gland. In response to TSH stimulus, triiodothyronine (T3) and thyroxin (T4) are released from the thyroid gland into the bloodstream bound to either thyroglobulins or other proteins such as albumin. T4 has minimal activity and is essentially a prohormone. T3 is the primary active form of the hormone, and only unbound T3 can enter a cell and activate the vital functions attributable to this hormone. The common measurement of total T3 and T4 often provides erroneous values and does not provide a clear picture of thyroid function. -

Should Human Chorionic Gonadotropine Treatment Increase
original article Should human chorionic gonadotropine treatment increase thyroid volume? Ayten Oguz1, Dilek Tuzun1, Murat Sahin1, Nese Bulbul1, Ahmet Celik2, Numan Guvenc3, Elif Inanc4, Kamile Gul1 ABSTRACT 1 Kahramanmaras Sutcu Objective: Our aim was to investigate the thyroid function tests and thyroid volume differences Imam University, Faculty of among males with isolated hypogonadotropic hypogonadism (IHH) who take androgen replacement Medicine, Department of treatment (ART). Materials and methods: Forty-four male with IHH with a mean age 33.2 (18-54), Endocrinology and Metabolism, Kahramanmaras, Turkey diagnosed in Endocrinology and Metabolism Department between September 2013 and September 2 Kahramanmaras Sutcu Imam 2014 and 40 healthy male control with a mean age 27.77 (18-55) were involved to study. Patient group University, Faculty of Medicine, was divided to testosterone-treated patients (n = 19) and human chorionic gonadotropine (hCG)- Department of Biochemistry, treated patients (n = 25). Patient group was compared in terms of total testosterone, thyroid func- Kahramanmaras, Turkey tion tests [thyroid stimulating hormone (TSH), free thyroxine (fT )] and thyroid volume, before and 3 4 Kahramanmaras Sutcu Imam 6 months after treatment. Patient group was compared with control group as well. Results: When University, Faculty of Medicine, Department of Family Medicine, we compared the patient group with the control group, there was no significant difference for age, Kahramanmaras, Turkey Body mass index, TSH, fT4 and thyroid volume between two groups before treatment. There was no 4 Kahramanmaras Sutcu Imam difference in terms of TSH, but fT4, testosterone levels and thyroid volume were significantly higher University, Faculty of Medicine, after treatment, when the patient group was compared before and after treatment (p < 0.05). -

DHEA Sulfate, and Aging: Contribution of the Dheage Study to a Sociobiomedical Issue
Dehydroepiandrosterone (DHEA), DHEA sulfate, and aging: Contribution of the DHEAge Study to a sociobiomedical issue Etienne-Emile Baulieua,b, Guy Thomasc, Sylvie Legraind, Najiba Lahloue, Marc Rogere, Brigitte Debuiref, Veronique Faucounaug, Laurence Girardh, Marie-Pierre Hervyi, Florence Latourj, Marie-Ce´ line Leaudk, Amina Mokranel, He´ le` ne Pitti-Ferrandim, Christophe Trivallef, Olivier de Lacharrie` ren, Stephanie Nouveaun, Brigitte Rakoto-Arisono, Jean-Claude Souberbiellep, Jocelyne Raisonq, Yves Le Boucr, Agathe Raynaudr, Xavier Girerdq, and Franc¸oise Foretteg,j aInstitut National de la Sante´et de la Recherche Me´dicale Unit 488 and Colle`ge de France, 94276 Le Kremlin-Biceˆtre, France; cInstitut National de la Sante´et de la Recherche Me´dicale Unit 444, Hoˆpital Saint-Antoine, 75012 Paris, France; dHoˆpital Bichat, 75877 Paris, France; eHoˆpital Saint-Vincent de Paul, 75014 Paris, France; fHoˆpital Paul Brousse, 94804 Villejuif, France; gFondation Nationale de Ge´rontologie, 75016 Paris, France; hHoˆpital Charles Foix, 94205 Ivry, France; iHoˆpital de Biceˆtre, 94275 Biceˆtre, France; jHoˆpital Broca, 75013 Paris, France; kCentre Jack-Senet, 75015 Paris, France; lHoˆpital Sainte-Perine, 75016 Paris, France; mObservatoire de l’Age, 75017 Paris, France; nL’Ore´al, 92583 Clichy, France; oInstitut de Sexologie, 75116 Paris, France; pHoˆpital Necker, 75015 Paris, France; qHoˆpital Broussais, 75014 Paris, France; and rHoˆpital Trousseau, 75012 Paris, France Contributed by Etienne-Emile Baulieu, December 23, 1999 The secretion and the blood levels of the adrenal steroid dehydro- number of consumers. Extravagant publicity based on fantasy epiandrosterone (DHEA) and its sulfate ester (DHEAS) decrease pro- (‘‘fountain of youth,’’ ‘‘miracle pill’’) or pseudoscientific asser- foundly with age, and the question is posed whether administration tion (‘‘mother hormone,’’ ‘‘antidote for aging’’) has led to of the steroid to compensate for the decline counteracts defects unfounded radical assertions, from superactivity (‘‘keep young,’’ associated with aging. -
In Vitro Effect of Triiodothyronine on the Cyclic Amp, Progesterone and Testosterone Level in Porcine Theca, Granulosa and Luteal Cells
ENDOCRINE REGULATIONS, Vol. 32, 93 – 98, 1998 93 IN VITRO EFFECT OF TRIIODOTHYRONINE ON THE CYCLIC AMP, PROGESTERONE AND TESTOSTERONE LEVEL IN PORCINE THECA, GRANULOSA AND LUTEAL CELLS E.L. GREGORASZCZUK, J. GALAS Laboratory of Animal Endocrinology and Tissue Culture, Department of Animal Physiology, Institute of Zoology, Jagiellonian University, Krakow, Poland Objective. To investigate the influence of thyroid hormone on steroid production and cAMP accumulation in porcine theca (Tc) and granulosa cells (Gc) isolated from preovulatory follicles as well as in luteal cells isolated during the mid-developing luteal phase. Methods. Granulosa and theca cells separated from pig ovarian follicles and pieces of corpora lutea were cultured in the incubation medium M199 with 5 % calf serum. After the addition of triiodothyronine (T3) and 3-isobutyl-1-methyl xanthine (IBMX) to the culture medium cAMP, progesterone and testosterone were estimated with the aid of specific RIA. Results. T 3 added to the culture media stimulated the steroid secretion and cAMP accumulation in all cell types investigated. In theca cells, T3 alone increased androgen production by 2 fold and the addition of IBMX further augmented the steroidogenesis by 2.2 fold. In granulosa cell culture, IBMX had no effect either on the basal or T3 stimulated progesterone secretion and cAMP accumu- lation. In luteal cell culture, IBMX added alone increased progesterone secretion and cAMP accu- mulation in the same manner as T3. Further augmentation of progesterone secretion (1.3-fold) and cAMP accumulation (1.1-fold) was observed after the addition of IBMX together with T3. Conclusion. The influence of thyroid hormone on cyclic nucleotide release by ovarian cells may suggest the involvement of cAMP-dependent mechanism in the realization of T3 action in ovarian cells. -

Isolated Central Hypothyroidism in Short Stature
003 1-399819513806-0967$03.00/0 PEDIATRIC RESEARCH Vol. 38, No. 6, 1995 Copyright O 1995 International Pediatric Research Foundation, Inc. Printed in U.S.A. Isolated Central Hypothyroidism in Short Stature SUSAN R. ROSE Department of Pediatrics, University of Tennessee, Memphis, Tennessee 38103-4901 Mild hypothyroidism can be difficult to diagnose, particularly tent with values seen in documented central hypothyroidism. when it is caused by deficiency of TSH or TSH-releasing hor- They were 13% of the total group, 16% of the ISS children, and mone (TRH). Such central hypothyroidism occurs most often in 32% of the ISS children with FT, in the lowest third of normal. association with growth hormone deficiency (GHD). Isolated (In comparison, diagnosis of GHD was made in 16% of the total central hypothyroidism has been considered rare. The TSH surge group.) In conclusion, use of a direct FT, assay to screen short test is the most sensitive test currently available for confirming children for possible subtle hypothyroidism (along with other the diagnosis. Results are abnormal in many cases where re- appropriate testing) identifies a subgroup with a one in three sponse to TRH is normal. Short children referred between 1986 possibility of an easily treated cause-isolated central hypothy- and 1994 for evaluation (n = 235, 74 girls; height 2 or more SD roidism. (Pediatr Res 38: 967-973, 1995) below mean for age; no history of radiation therapy) were selected for study. TSH samples were obtained hourly for study of TSH surge (1400-1800 h and 2200-0400 h). Growth hor- Abbreviations mone (GH) samples were obtained every 20 min (2000-0800 h). -

Annual Changes in the Concentrations of Free Triiodothyronine, Progesterone and Testosterone in Prepubertal Red Deer (Cervus Elaphus Elaphus) Males and Females
Journal of Animal and Feed Sciences, 24, 2015, 113–117 The Kielanowski Institute of Animal Physiology and Nutrition, PAS, Jabłonna Annual changes in the concentrations of free triiodothyronine, progesterone and testosterone in prepubertal red deer (Cervus elaphus elaphus) males and females J. Kuba1, B. Błaszczyk, T. Stankiewicz and J. Udała West Pomeranian University of Technology in Szczecin, Department of Animal Reproduction Biotechnology and Environmental Hygiene, Dr. Judyma 6, 71-466 Szczecin, Poland KEY WORDS: free triiodothyronine, season, ABSTRACT. The aim of the study was to analyse the annual changes in the puberty, sex, red deer concentration of free triiodothyronine, progesterone and testosterone in the serum of prepubertal red deer males and females. Blood was collected monthly from 8 stags and 8 hinds for a period of one year, beginning in November. Hormone concentrations were determined using an immunofluorescence method (TR-FIA). Monitoring of the duration of the prepubertal period, based on the progesterone concentrations in females and testosterone concentrations in the males, suggested that the prepubertal period ended in September in both Received: 4 March 2015 sexes. The experiment revealed the annual rhythm in free triiodothyronine (FT3) Revised: 18 May 2015 Accepted: 15 June 2015 secretion, with significantly higher concentrations in the winter-spring period in comparison with summer-autumn in both, males (P < 0.01) and females (P < 0.05). The results showed that the season considerably influenced the intensity of FT3 secretion in prepubertal red deer and that the secretion dynamics in both sexes were similar, however, the concentrations in the males 1 Corresponding author: reached higher levels than in the females in each season and across the whole e-mail: [email protected] experiment.