Lincoln Medical Center
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2019 Community Health Needs Assessment Survey
COMMUNITY HEALTH NEEDS ASSESSMENT 2019 To all New Yorkers: As New York City’s public health care system, our goal is to empower you to live your healthiest life. Clinical care starts with you and your health care team, but we recognize that many factors impact your health beyond medical care alone – a safe home environment, space to be physically active, access to fresh food, even exposure to daily stress and poor social well-being can impact your health outcomes. To assess and prioritize the greatest health needs of the neighborhoods and communities we serve, NYC Health + Hospitals conducted a comprehensive and inclusive process to complete this Community Health Needs Assessment for 2019. The findings represent the voices of the patients we serve, clinical experts and community partners, and are backed by quantitative data analysis. Recognizing that the health needs of patients coming through our hospital doors may not represent the wider health needs of the community, we embarked on an extensive stakeholder engagement process led by OneCity Health, who built new relationships with community stakeholders through the Delivery System Reform Incentive Payment (DSRIP) program. For the first time, we conducted a system-wide assessment to identify priorities that need to be addressed city-wide and will allow us to maximize our resources in response. We believe that we should reliably deliver high-quality services and that patients should have a consistent experience at our facilities. Since our 2016 assessment, we have worked tirelessly to address significant health needs of the community and to make it easier for our patients to access our services: • We opened and renovated dozens of community-based health centers to expand access to primary and preventive care. -

New York City Health and Hospitals Corporation New York City Health and Hospitals Corporation
NEW YORK CITY HEALTH AND HOSPITALS CORPORATION NEW YORK CITY HEALTH AND HOSPITALS CORPORATION Bronx Kings County Hospital Center Metropolitan Hospital Center Jacobi Medical Center 451 Clarkson Avenue 1901 First Avenue 1400 Pelham Parkway South Brooklyn, New York 11203 New York, New York 10029 Bronx, New York 10461 718-245-3131 212-423-6262 212-918-5000 Woodhull Medical and Mental Renaissance Health Care Lincoln Medical and Mental Health Center Network Diagnostic Health Center 760 Broadway & Treatment Center 234 East 149th Street Brooklyn, New York 11206 215 West 125th Street Bronx, New York 10451 718-963-8000 New York, New York 10027 718-579-5000 212-932-6500 Manhattan Morrisania Diagnostic Bellevue Hospital Center Queens & Treatment Center 462 First Avenue Elmhurst Hospital Center 1228 Gerard Avenue New York, New York 10016 79-01 Broadway Bronx, New York 10452 212-562-4141 Elmhurst, New York 11373 718-960-2777 Coler Goldwater Specialty 718-334-4000 North Central Bronx Hospital Hospital Queens Hospital Center 3424 Kossuth Avenue Roosevelt Island 82-70 164th Street Bronx, New York 10467 New York, New York 10044 Jamaica, New York 11432 718-519-5000 212-848-6000 718-883-3000 Segundo Ruiz Belvis Diagnostic Gouverneur Healthcare Services & Treatment Center 227 Madison Street Staten Island 545 East 142nd Street New York, New York 10002 Sea View Hospital Bronx, New York 10454 212-238-7000 Rehabilitation Center & Home 718-579-4000 460 Brielle Avenue Harlem Hospital Center Staten Island, New York 10314 506 Lenox Avenue Brooklyn 718-317-3000 New York, New York 10037 Coney Island Hospital 212-939-1000 2601 Ocean Parkway Brooklyn, New York 11235 718-616-30000 Cumberland Diagnostic & Treatment Center 100 North Portland Avenue Brooklyn, New York 11205 718-260-7500 Dr. -

Cornell University Official Publication
CORNELL UNIVERSITY OFFICIAL PUBLICATION Volume XXVIII Number I Announcement of The Medical College for 1936-37 at 1300 York Avenue, New York City and the first year, also, at Ithaca, N. Y. Ithaca, New York Published by the University July 1, 1936 Printed by W. F. Humphrey Press Inc. Geneva, N. Y. CONTENTS PAGE Calendar _ 5 Board of Trustees . 6 New York Hospital-Cornell Medical College Association . 7 Medical College Council . 7 Officers of Administration . .8 and . Executive Faculty Committees of the Faculty . 9 and Faculty Teaching Staff. 10 New York Hospital Staff . 27 Bellevue Hospital, Staff of Second Division . 38 Memorial Hospital Staff 40 General Statement . 43 Requirements for Admission .... 48 Admission to Advanced Standing . 49 Requirements for Promotion and Graduation ......50 General Information:. .52 Fees, Scholarships, Loans, Prizes. 52 Educational Policy and Description of Courses: . 56 Summary of Hours in Medical Course . 58 Anatomy .... 59 Applied Pathology and Bacteriology . 67 Bacteriology 64 Biochemistry . 62 Legal Medicine 83 Medicine and Medical Specialties. 67 72 Obstetrics and Gynecology 64 Pathology . Pediatrics 74 Pharmacology 66 Physiology 63 Psychiatry. 75 81 Public Health and Preventive Medicine 3 PAGE and Surgery Surgical Specialties ... 77 . ... 82 Radiology . Schedule of Courses . ..... 84 Special Students . .....88 The Graduate School . .... 89 The Ithaca Division: of 91 Faculty Medicine at Ithaca . 92 University Calendar . 92 General Statement . Plan of Instruction 94 Anatomy . 94 Histology and Embryology 96 Physiology and Biochemistry . 97 Summarized Statement . ... 99 General Information . 100 Schedule of Instruction . 102 Combined A.B. and M.D. Degrees . 102 Graduate Work at Ithaca .... 104 Internship Appointments ..... ... 106 Register of Students, 1936-1937 . -

Network Review | SUMMER/FALL 2008 Edition SUMMER/FALL 2008 Edition | Network Review
NNetworketwork ReviewReview Building for Success SUMMER/FALL 2008 Edition Harlem Hospital Center Lincoln Medical and Mental Health Center Metropolitan Hospital Center Morrisania Neighborhood Family Health Center Renaissance Health Care Network Segundo Ruiz Belvis Neighborhood Family Health Center 4BSBI+POFT "OJUB4POJ .% -JODPMO)PTQJUBM.FEJDBM%JSFDUPS3JDIBSE,4UPOF .% .FUSPQPMJUBO)PTQJUBM.FEJDBM%JSFDUPS.FSZM 8FJOCFSH .FUSPQPMJUBO)PTQJUBM&YFDVUJWF%JSFDUPS'SPOUSPX%S"ZNBO&M.PIBOEFT LFZOPUFTQFBLFS4S7JDF Sarah Jones’ performance brought the 1SFTJEFOU +PTn34gODIF[ ))$1SFTJEFOU"MBO%"WJMFTBOE$IBSMZOO(PJOT $IBJSQFSTPO ))$#PBSEPG%JSFDUPST audience to a standing ovation. 5)"//6"-63#"/ )&"-5)$0/'&3&/$& 4)08$"4&%.0%&-40'*/5&37&/5*0/ continues on pg. 11 453"5&(*&4"/%#&4513"$5*$&4 1BSUOFSTIJQT As racial and ethnic disparities in workshops with participants from New CAB/Auxiliary Network Annual Dinner healthcare outcomes continue to make York, Texas and California and focused headlines both locally and nationally, on specific health disciplines that have the 7th Annual Conference on Urban garnered measurable successes in Health brought together healthcare treatment modalities. professionals and other stakeholders to share innovative strategies aimed The clinical expertise of our Network at eliminating such inequalities in hospitals and Neighborhood Family health. The forum, held on June 12th Health Centers was prominently and 13th at the Helmsley Park Lane showcased during the workshops. continues on pg. 12 Hotel in Manhattan, featured clinical continues on pg. 11 Network Review | SUMMER/FALL 2008 Edition SUMMER/FALL 2008 Edition | Network Review &NCSBDJOH$IBOHF Welcome to the 2008 Summer/Fall Please join me in wishing Metropolitan of 15,000 square feet including 37 exam Edition of our Network Newsletter. This the best in their future endeavors. -

Careconnect Facilities
CareConnect Facilities Manhattan Hospitals Yale-New Haven Northern Harlem Westchester Bridgeport Metropolitan Lenox Hill Manhattan Eye, Ear & Throat Phelps Memorial Lenox Health Greenwich Greenwich Montefiore White Plains Village Medical Bellevue Centers Peconic Bay Medical Center North Central Bronx Jacobi Huntington Glen Cove Lincoln Syosset North Shore University Zucker Hillside Plainview Elmhurst LIJ Medical Center Cohen Children’s LIJ Forest Nassau University Hills Queens Medical Center Southside Woodhull Wyckoff Heights South Oaks Kings County LIJ Valley Stream Staten Island Maimonides University (North) Coney Island Staten Island University (South) For a searchable list of CareConnect’s providers, visit CareConnect.com/providersearch Hospitals • Bellevue Hospital Center, 462 First Avenue, New York, NY 10016, P: 212-562-4141 • Bridgeport Hospital, 267 Grant St, Bridgeport, CT 06610, P: 203-688-8412 • Coney Island Hospital, 2601 Ocean Parkway, Brooklyn, NY 11235, P: 718 616-3000 • Elmhurst Hospital Center, 79-01 Broadway, Elmhurst, NY, 11373, P: 718-334-4000 • Glen Cove Hospital, 101 St. Andrews Lane, Glen Cove, NY 11542, P: 516-674-7540 • Greenwich Hospital, 5 Perryridge Road, Greenwich, CT 06 830, P: 203-688-8412 • Harlem Hospital Center, 506 Lenox Avenue, New York, NY 10037, P: 212-939-1000 • Huntington Hospital, 270 Park Avenue, Huntington, NY 11743, P: 631-351-2000 • Jacobi Medical Center, 1400 Pelham Parkway South, Bronx, NY 10461, P: 718-918-5000 • Kings County Hospital Center, 451 Clarkson Avenue, Brooklyn, NY 11203, P: 718-245-3131 -

Standpoints on Psychiatric Deinstitutionalization Alix Rule Submitted in Partial Fulfillment of the Requirements for the Degre
Standpoints on Psychiatric Deinstitutionalization Alix Rule Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Graduate School of Arts and Sciences COLUMBIA UNIVERSITY 2018 © 2018 Alix Rule All rights reserved ABSTRACT Standpoints on Psychiatric Deinstitutionalization Alix Rule Between 1955 and 1985 the United States reduced the population confined in its public mental hospitals from around 600,000 to less than 110,000. This dissertation provides a novel analysis of the movement that advocated for psychiatric deinstitutionalization. To do so, it reconstructs the unfolding setting of the movement’s activity historically, at a number of levels: namely, (1) the growth of private markets in the care of mental illness and the role of federal welfare policy; (2) the contested role of states as actors in driving the process by which these developments effected changes in the mental health system; and (3) the context of relevant events visible to contemporaries. Methods of computational text analysis help to reconstruct this social context, and thus to identify the closure of key opportunities for movement action. In so doing, the dissertation introduces an original method for compiling textual corpora, based on a word-embedding model of ledes published by The New York Times from 1945 to the present. The approach enables researchers to achieve distinct, but equally consistent, actor-oriented descriptions of the social world spanning long periods of time, the forms of which are illustrated here. Substantively, I find that by the early 1970s, the mental health system had disappeared from public view as a part of the field of general medicine — and with it a target around which the existing movement on behalf of the mentally ill might have effectively reorganized itself. -

Your Unpublished Thesis, Submitted for a Degree at Williams College and Administered by the Williams College Libraries, Will Be Made Available for Research Usc
WILLIAMS COLLEGE LIBRARIES COPYRICiHT ASSIGNMENT AND INSTRUCTIONS FOR A STUDENT THESIS Your unpublished thesis, submitted for a degree at Williams College and administered by the Williams College Libraries, will be made available for research usc. You may, through this form, provide instructions regarding copyright, access, dissemination and reproduction of' your thesis. The College has the right in all cases to maintain and preserve theses both in hardcopy and electronic format, and to make such copies as the Libraries require !'or their research and archival functions. _The f~1culty advisor/s to the student writing the thesis claims joint authorship in this work. -~ 1/wc have included in this thesis copyrighted material for which 1/we have not received permission from the copyright holdcr/s. If' you do not secure copyright permissions by the time your thesis is submitted, you will still be allowed to submit. However, if the necessary copyright permissions arc not received, c-posting of your thesis may be affected. Copyrighted material may include images (tables, drawings, photographs, figures, maps, graphs, etc.), sound files, video material, data sets, and large portions of text. l. COI'YRICiiiT An author by law owns the copyright to his/her work, whether or not a copyright symbol and elate arc placed on the piece. Please choose one of the options below with respect to the cupyright in your the,; is. 1/wc choose not to retain the copyright to the thesis, and hereby assign the copyright to Williams College. Selecting this option will assign copyright to the College. !Cthc author/swishes later to publish the work, he/she/they will need to obtain permission to do so Crom the Libraries, which will be granted except in unusual circumstances. -
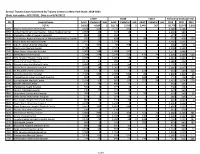
Annual Trauma Cases Submitted by Trauma Centers in New York State
Annual Trauma Cases Submitted by Trauma Centers in New York State: 2018-2021 (Date last update: 8/17/2021, Data as of 8/3/2021) Y2019 Y2020 Y2021 TOTALS by Discharge Year PFI Hospital Name Adult Pediatric Unk Adult Pediatric Unk Adult Pediatric Unk 2019 2020 2021 TOTAL 54,562 4,209 1 50,176 3,793 3 5,443 367 - 58,772 53,972 5,810 0001 Albany Medical Center Hospital 3,168 320 . 3,772 392 . 3,488 4,164 - 0058 United Health Services Hospital - Wilson Medical Center 1,067 23 . 934 13 . 1,090 947 - 0135 Champlain Valley Physicians Hospital 465 12 . 314 2 . 477 316 - 0180 Mid Hudson Regional Hospital of Westchester Medical Center 745 22 . 428 . 98 2 767 428 100 0181 Vassar Brothers Medical Center 1,141 15 . 1,029 2 . 1,156 1,031 - 0208 John R. Oishei Children's Hospital 64 335 . 68 258 2 4 399 326 6 0210 Erie County Medical Center 2,598 1 . 2,525 . 2,599 2,525 - 0245 Stony Brook University Hospital 2,003 168 . 1,686 162 . 2,171 1,848 - 0413 Strong Memorial Hospital 2,244 254 . 2,246 223 470 74 2,498 2,469 544 0511 NYU Langone Hospital-Long Island 1,288 77 . 1,305 56 26 8 1,365 1,361 34 0527 Mount Sinai South Nassau 1,171 17 . 989 4 . 1,188 993 - 0528 Nassau University Medical Center 1,384 34 . 1,187 25 . 1,418 1,212 - 0541 North Shore University Hospital 2,150 16 . 1,907 10 . -
Final Program
FINAL PROGRAM www.MohsCollege.org/AnnualMeeting THE REVOLUTIONARY 12 QSCRYOSTAT Avantik Biogroup The #1 Name in Mohs. Eliminate chatter, venetian blind & thick/thin Up to 75% Less Noise Ergonomically Designed Adjustable LED Lighting Ultra Smooth Handwheel Operation Precision & Accuracy Perfect Sections Dovetail Bladeholder Perfect Sections Peltier - Fast Freezing UV Disinfection Option The Mohs Laboratory Solution Your laboratory... quick, efficient, easy. The QS12 and QS12UV have been the result of extensive research and development over the span of years. From bladeholder to microtome, cryobar to refrigeration... every aspect of the QS12 and QS12UV is unsurpassed in quality and precision. A Perfect Section...it’s unmistakable! The Mohs Laboratory Performers CALL TODAY TO SPEAK TO YOUR MOHS LAB SPECIALIST REGARDING ALL OF YOUR MOHS LAB NEEDS! 888.392.8411 www.avantik-us.com Table of Contents ACMS Board of Directors ..................................................................................................................................... 2 THE REVOLUTIONARY ACMS Committees and Task Forces – 2016-17 ......................................................................................................... 3 Welcome from the President ................................................................................................................................... 4 12 Welcome from the Scientific Program Committee Chair ............................................................................................... 4 QSCRYOSTAT Program -
Nr********************************************************** I' ,...°4' L`,1 ,'.1{ II
VP DOCUMENT RESUME ED 179 511 SP 014 905 .TITLE Nurse Staffing ReqUirements and Related Toidcs: Sea.ected Bib,licgraphy. Nurse Flanning Information Series No. 9. INSTITUTION Franklin Research Center, Philadelpg), Pa. SPONS AGENCY Health Resources Administration WI /PHS), Bethesda, Md. Div. of Nursing. FEPORT NO HRA-79-39: HRP-0501001 PUB DATE Jul 79 , CONTRACT 232-7R-0000 NOTE 224p. 't EDRS PRICE MF01/PCO9 Plus Postage. U.SCRIPIORS Health Personnel: *Hospital Personnel; *Labor; *Manpower Needs: 'Manpower Utilization; Models; .*Nurses; Nursing: Nursing Homes: *0ccupationa4 Surveys: *Staff Utili2ation ABSTRACT Recent literature on the changing staffing requirements for regitered nurses arid the factors affectingthose requirements is cited in this annctated bibliographythat comprises the ninth volume in the NOrse Planning InformationSeries. A broad concept ot staffing is emplo7cd and includes information usefulto . both managers wit n individual institutions and to heAlth planners concerned with co munity, county, ot state institutions.Abstracts of the literature arg ouped accerding to the following categories: hospitel inpatient nd hospital'outpatient settings; long-termcare settings; models and strategies, and economic-studiesot staffing methodoiogies: regional, state, and national -studies ofneeds and requirements:-and bibliographies And summaries. (JD) 4 *********************************************************************** Reproductions supplied by EPPS are the'best thatcan be made from the origin01 document. ***********Nr********************************************************** I' ,...°4' l`,1 ,'.1{ II l'. ; ).. i ' ,.' .. '. ',"',441. .. ;,.1.1r7 'At, ,. IT. , .. 1 ,:tt . ,.. !,,,,, ;,',i:4.'el:? :: ', , ,,,,a.... .:: y, ;44) .. '' If0V:,:i A ',54,T.i14;, : -4 t ., h.d.'ci!t r "-F 4 , .. tikitiathaNWk e , f , A, .1.1.,..1. ,,,,e it,-.4' i:: re f.:1.,e.. : 'c ,: L'.. it, I , s1,11, :t; .. -

Exempt Health Care Facilities List
Exempt Health Care Facilities Address City Zip BELLEVUE HOSPITAL CENTER FIRST AVENUE AT 27TH STREET NEW YORK 10016 BELLEVUE HOSPITAL CENTER@BELLEVUE TREATMENT 26TH ST & 1ST AVE NEW YORK 10016 BETH ISRAEL MEDICAL CENTER/HERBERT & NELL SINGER DIVISION 170 EAST END AVENUE NEW YORK 10128 BETH ISRAEL MEDICAL CENTER-KINGS HWY DIV 3201 KINGS HIGHWAY BROOKLYN 11234 BETH ISRAEL MEDICAL CENTER-PETRIE CAMPUS FIRST AVE AT 16TH STREET NEW YORK 10003 BETH ISRAEL MEDICAL CENTER@ALCOHOL TREATMENT PROGRAM 50 COOPER SQUARE NEW YORK 10003 BETH ISRAEL MEDICAL CENTER@BETH ISRAEL CHRONIC DIALYSIS CTR 120 EAST 16TH STREET NEW YORK 10003 BETH ISRAEL MEDICAL CENTER@BIMC #2 103 EAST 125TH STREET NEW YORK 10035 BETH ISRAEL MEDICAL CENTER@BIMC #4 21 OLD BROADWAY NEW YORK 10027 BETH ISRAEL MEDICAL CENTER@BIMC 1-E 2-F 3-G 429 2ND AVENUE NEW YORK 10010 BETH ISRAEL MEDICAL CENTER@BIMC 2-C 435 2ND AVENUE NEW YORK 10010 BETH ISRAEL MEDICAL CENTER@BIMC 3-C 433 2ND AVENUE NEW YORK 10010 BETH ISRAEL MEDICAL CENTER@BIMC 8 & 8-D 140 WEST 125TH STREET NEW YORK 10027 BETH ISRAEL MEDICAL CENTER@BIMC CONEY ISLAND 2601 OCEAN PARKWAY BROOKLYN 11235 BETH ISRAEL MEDICAL CENTER@BIMC COOPER SQUARE 26 AVENUE A NEW YORK 10003 BETH ISRAEL MEDICAL CENTER@BIMC CUMBERLAND 98 FLATBUSH AVENUE BROOKLYN 11217 BETH ISRAEL MEDICAL CENTER@BIMC DIALYSIS AT 1555 THIRD AVENUE 1555 THIRD AVENUE NEW YORK 10128 BETH ISRAEL MEDICAL CENTER@BIMC DIALYSIS CTR AT NORTH DIVISION 170 EAST END AVENUE NEW YORK 10128 BETH ISRAEL MEDICAL CENTER@BIMC LENOX HILL 1082 LEXINGTON AVENUE NEW YORK 10021 BETH ISRAEL MEDICAL -

Lincoln Medical and Mental Health Center 234 Eugenio Maria De Hostos Blvd.(149Th Street) the Bronx, New York 10451 718-579-5000
LINCOLN LINCOLN MEDICAL AND MENTAL HEALTH CENTER 234 EUGENIO MARIA DE HOSTOS BLVD.(149TH STREET) THE BRONX, NEW YORK 10451 718-579-5000 LINCOLN MEDICAL AND MENTAL HEALTH CENTER Predoctoral Psychology Internship Program Dear Applicant: Thank you for your interest in the Internship Program at Lincoln Medical and Mental Health Center. Please take the time to review our 2017-2018 Psychology Internship Program brochure (for the 2018-2019 training year). Please note that we will be operating in accordance with the APPI Online Application process for the 2018-2019 internship year. We are accepting online applications this year. Please click on the following link for more information: http://www.appic.org/match/5_3_match_application.html Also, to maximize your chances for a successful match, please take the time to read below, as well as our brochure. ♦ Each applicant is responsible for compiling all the documentation that is requested, including APPI Online Application, CV, transcripts, and only three letters of recommendation. ♦ Your application must be received by November 30th. ♦ Please be aware that we participate in the APPIC Internship Matching Program. You must obtain the Application Agreement Package from the National Matching Services Inc, P.O.Box 1208, Lewiston, NY 14092-8208. Tel# (716)282- 4013, Fax# (716)282-0611, Internet web address www.natmatch.com/psychint. (Please note: once matched, all interns-to- be are required to pass preliminary background checks and drug screenings in August with our Human Resources Department. It is upon successful clearance that internship may begin in September.) ♦ Our program code number is 144711 ♦ Our training program involves a wide range of training opportunities, from newborns to geriatric populations.