S13104-019-4337-6.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Resistance to Paromomycinis Conferred by Rpsl Mutations
VOL.53 NO. 12, DEC.2000 THE JOURNAL OF ANTIBIOTICS pp.1424 - 1427 COMMUNICATIONS TO THE EDITOR Resistance to Paromomycinis Conferred by paromomycin at a frequency of 10 7 or 10 8, respectively. rpsL Mutations, Accompaniedby an Out of 77 randomly selected paromomycin resistant Enhanced Antibiotic Production in mutants, 4 strains, designated as KO-347-350, were found to produce actinorhodin in 7 to 10-fold greater amounts Streptomyces coelicolor A3 (2) than the parent strain (Table 1). In our previous studies10'11>14) we established that an antibiotic- Sir: overproducing characteristic frequently appears together Aminoglycoside antibiotics interfere with bacterial with the mutation within the rpsL gene. To address this protein synthesis by binding to the 3OS ribosomal relationship weexamined for the presence of mutations in subunit1>2). Their binding is known to stabilize the tRNA- rpsL. Strikingly, all antibiotic-overproducing mutants mRNAinteraction in the A-site by decreasing the tRNA (Class I) examined had rpsL mutations, resulting in the dissociation rates3). Eventually, aminoglycoside antibiotics alteration of amino acid residue 91 from proline to serine cause a decrease in translational accuracy and inhibit (Table 1). In contrast, another group of paromomycin translocation of the ribosome. Such detrimental effects of resistant mutant, (Class II; KO-351-356) which do not aminoglycoside antibiotics can be circumvented by overproduce antibiotic, was found to have no mutation mutations altering 16S rRNA4~6) or certain ribosomal within the rpsL gene. It should be pointed out that Class I proteins6^; these mutations have been found in either the mutants displayed a higher level of resistance to nucleotide 530 or 915 regions of 16S rRNAor in ribosomal paromomycin than that of Class II mutants (Table 1). -

Antibiotic Resistance and Typing of the Methicillin-Resistant Staphylococcus Aureus Clones in Kuwait Hospitals, 2016–2017 Samar S
Boswihi et al. BMC Microbiology (2020) 20:314 https://doi.org/10.1186/s12866-020-02009-w RESEARCH ARTICLE Open Access Antibiotic resistance and typing of the methicillin-resistant Staphylococcus aureus clones in Kuwait hospitals, 2016–2017 Samar S. Boswihi, Edet E. Udo* and Wadha AlFouzan Abstract Background: Methicillin-resistant Staphylococcus aureus (MRSA) belong to diverse genetic backgrounds that differ in antibiotic resistance. Knowledge of the local clonal composition of MRSA strains is important for patients’ management and for designing effective control and eradication methods. The aim of this study was to compare the antibiotic resistance patterns and genotypic characteristics of MRSA isolates obtained in public hospitals in Kuwait in 2016 and 2017 for changes in their resistance patterns and clonal composition. Methods: A total of 4726 MRSA isolates obtained in 2016–2017 from clinical specimens in Kuwait public hospitals were characterized using antibiogram, SCCmec typing, spa typing and DNA microarray. Results: The isolates expressed resistance to fusidic acid (52.9%), kanamycin (41.6%), gentamicin (32.5%) and erythromycin (36.2%). The prevalence of high-level mupirocin resistance decreased from 3.7% in 2016 to 2.4% in 2017, while the proportion of resistance to other antibiotics remained relatively stable. A total of 382 spa types were detected with eight spa types, t688 (N = 547), t304 (N = 428), t860 (N = 394), t127 (N = 306), t044 (N = 230), t311 (N = 243), t223 (N = 184) and t002 (N = 181) constituting 53.1% of the MRSA isolates in 2016–2017. Of the 3004 MRSA isolates obtained in 2016 (N = 1327) and 2017 (N = 1677) selected for DNA microarray analysis, 26 clonal complexes (CCs) were identified. -

Topical Antibiotics for Impetigo: a Review of the Clinical Effectiveness and Guidelines
CADTH RAPID RESPONSE REPORT: SUMMARY WITH CRITICAL APPRAISAL Topical Antibiotics for Impetigo: A Review of the Clinical Effectiveness and Guidelines Service Line: Rapid Response Service Version: 1.0 Publication Date: February 21, 2017 Report Length: 23 Pages Authors: Rob Edge, Charlene Argáez Cite As: Topical antibiotics for impetigo: a review of the clinical effectiveness and guidelines. Ottawa: CADTH; 2017 Feb. (CADTH rapid response report: summary with critical appraisal). ISSN: 1922-8147 (online) Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services. While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. CADTH does not guarantee and is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in any third-party materials used in preparing this document. -

Farrukh Javaid Malik
I Farrukh Javaid Malik THESIS PRESENTED TO OBTAIN THE GRADE OF DOCTOR OF THE UNIVERSITY OF BORDEAUX Doctoral School, SP2: Society, Politic, Public Health Specialization Pharmacoepidemiology and Pharmacovigilance By Farrukh Javaid Malik “Analysis of the medicines panorama in Pakistan – The case of antimicrobials: market offer width and consumption.” Under the direction of Prof. Dr. Albert FIGUERAS Defense Date: 28th November 2019 Members of Jury M. Francesco SALVO, Maître de conférences des universités – praticien hospitalier, President Université de Bordeaux M. Albert FIGUERAS, Professeur des universités – praticien hospitalier, Director Université Autonome de Barcelone Mme Antonia AGUSTI, Professeure, Vall dʹHebron University Hospital Referee Mme Montserrat BOSCH, Praticienne hospitalière, Vall dʹHebron University Hospital Referee II Abstract A country’s medicines market is an indicator of its healthcare system, the epidemiological profile, and the prevalent practices therein. It is not only the first logical step to study the characteristics of medicines authorized for marketing, but also a requisite to set up a pharmacovigilance system, thus promoting rational drug utilization. The three medicines market studies presented in the present document were conducted in Pakistan with the aim of describing the characteristics of the pharmaceutical products available in the country as well as their consumption at a national level, with a special focus on antimicrobials. The most important cause of antimicrobial resistance is the inappropriate consumption of antimicrobials. The results of the researches conducted in Pakistan showed some market deficiencies which could be addressed as part of the national antimicrobial stewardship programmes. III Résumé Le marché du médicament d’un pays est un indicateur de son système de santé, de son profil épidémiologique et des pratiques [de prescription] qui y règnent. -
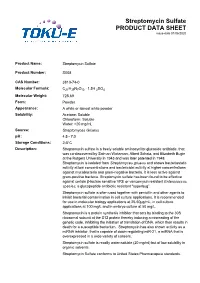
Streptomycin Sulfate PRODUCT DATA SHEET Issue Date 01/06/2020
Streptomycin Sulfate PRODUCT DATA SHEET issue date 01/06/2020 Product Name: Streptomycin Sulfate Product Number: S008 CAS Number: 3810-74-0 Molecular Formula: C21H39N7O12 · 1.5H 2SO4 Molecular Weight: 728.69 Form: Powder Appearance: A white or almost white powder Solubility: Acetone: Soluble Chloroform: Soluble Water: >20 mg/mL Source: Streptomyces Griseus pH: 4.5 - 7.0 Storage Conditions: 28°C Description: Streptomycin sulfate is a freely soluble aminocyclitol glycoside antibiotic, that was co-discovered by Salman Waksman, Albert Schatz, and Elizabeth Bugie at the Rutgers University in 1943 and was later patented in 1948. Streptomycin is isolated from Streptomyces griseus and shows bacteriostatic activity at low concentrations and bactericidal activity at higher concentrations against mycobacteria and gram-negative bacteria. It is less active against gram-positive bacteria. Streptomycin sulfate has been found to be effective against certain βlactam sensitive VRE or vancomycin resistant Enterococcus species; a glycopeptide antibiotic resistant "superbug”. Streptomycin sulfate is often used together with penicillin and other agents to inhibit bacterial contamination in cell culture applications. It is recommended for use in molecular biology applications at 2550μg/mL, in cell culture applications at 100 mg/L and in embryo culture at 50 mg/L. Streptomycin is a protein synthesis inhibitor that acts by binding to the 30S ribosomal subunit at the S12 protein thereby inducing a misreading of the genetic code, inhibiting the initiation of translation of DNA, which then results in death for a susceptible bacterium. Streptomycin has also shown activity as a miRNA inhibitor, that is capable of down-regulating miR-21, a miRNA that is overexpressed in a wide variety of cancers. -

Neomycin—Production and Antibiotic Properties
NEOMYCIN—PRODUCTION AND ANTIBIOTIC PROPERTIES Selman A. Waksman, … , Hubert A. Lechevalier, Dale A. Harris J Clin Invest. 1949;28(5):934-939. https://doi.org/10.1172/JCI102182. Research Article Find the latest version: https://jci.me/102182/pdf NEOMYCIN-PRODUCTION AND ANTIBIOTIC PROPERTIES 1, 2 3 By SELMAN A. WAKSMAN, HUBERT A. LECHEVALIER, AND DALE A. HARRIS (From the Department of Microbiology, New Jersey Agricultural Experiment Station, Rutgers University, New Brunswick, N. J.) ANTIBIOTIC SURVEYS All these cultures proved to be highly active against mycobacteria. of During the last 10 years, a large number anti- Only few of the cultures, however, that gave biotics which are active against Gram-negative good activity by the agar-streak method yielded and Gram-positive bacteria, mycobacteria, rickett- filtrates which possessed corresponding potency. siae, and certain of the larger viruses were iso- This may be due to a variety of factors, such as lated (1) from various species and strains of the the formation by a single organism of more than genus Streptomyces. This served to focus atten- one antibiotic or the production of different anti- tion on the actinomycetes as potential producers of biotics under different conditions of culture. One antimicrobial agents that might possess promising of these cultures proved to be highly promising chemotherapeutic properties. The fact that nearly and was selected for more detailed investigations. 20 to 50%o of these organisms possess antimicrobial This culture was entered into the Collection as No. activities served to heighten this interest. Numer- 3535. The nature of its antimicrobial spectrum, ous surveys have been conducted. -

Empirical Antimicrobial Therapy for Children with Cystic Fibrosis
Empirical antimicrobial therapy for children with Cystic Fibrosis Document ID CHQ-GDL-01073 Version no. 2.0 Approval date 17/12/2020 Executive sponsor Executive Director of Medical Services Effective date 17/12/2020 Director Respiratory Medicine Review date 17/12/2022 Author/custodian Director Infection Management and Prevention Service, Immunology and Rheumatology Supersedes 1.1 Applicable to All Children’s Health Queensland staff Authorisation Executive Director Clinical Services (QCH) Purpose This guideline provides Children’s Health Queensland (CHQ) recommendations for empirical antimicrobial therapy for children with Cystic Fibrosis (CF), for inpatient and outpatient management. Scope This guideline provides information for CHQ staff caring for paediatric CF patients. Related documents Procedures, Guidelines, Protocols • CHQ Paediatric Therapeutic Drug Monitoring – Tobramycin/Gentamicin • CHQ Paediatric Therapeutic Drug Monitoring - Vancomycin • CHQ@Home Outpatient Parenteral Antimicrobial Therapy Prescribing, Administration and monitoring guideline • CHQ-PROC-01036 Antimicrobial: Prescribing, Management and Stewardship and CHQ Antimicrobial Restriction list • CHQ-PROC-63223 Management of patients with cystic fibrosis • CHQ-GDL-01061 Immunisation Guideline for Medically at Risk Children • CHQ-GDL-01076 Paediatric antibiotic allergy assessment, testing and de-labelling • CHQ-GDL-70047 Clinical guidelines for the care of children and adolescents with Cystic Fibrosis - Volume 1: Respiratory Care Guideline Empirical antimicrobial therapy -

Topical Antibiotics
Topical antibiotics Microbiological point of view [email protected] • Topical antibiotics • Efficacy • Antibiotic resistance – Propionibacteria/acne • Tetracyclines • macrolides – Staphylococci/impetigo • Fusidic acid • Mupirocin • Epilogue Topical antibiotics in dermatology • Bacitracin • Chloramphénicol • Clindamycin • Erythromycin • Fusidic acid • Gentamicin • Miconazol • Mupirocin • Neomycin • Polymyxin B • Sulfamides • Tétracyclines • Benzoyle peroxyde • Azelaic acid + “bactéries (filtrat polyvalent) + huile de foie de morue 125 mg + sulfanilamide 200 mg/1 g “ Topical antibiotics in ophtalmology / ORL • Bacitracine • Chloramphénicol • Fusidic acid • Gentamicin • Gramicidin* • Quinolones: o-,nor-, cipro-, lome- floxacin* • Neomycin • Polymyxin B • Rifamycin* • Sulfamides • Tétracyclines • Trimethoprim* • Tobramycin* • Tyrothricine* Topical antibiotics: efficacy • Impetigo: mupirocin & fusidic acid*: + ** • Acne: + ~ benzoyl peroxyde • Chronic suppurative otitis media*: + ** • Acute bacterial conjunctivitis*: + * (Cochrane review) ** better than antiseptics Topical antibiotics: resistance • Propionibacterium spp: resistance to erythromycin: – mutation in the genes encoding 23S ribosomal RNA (3 phenotypes) resistance to tetracycline: – Mutation of the gene encoding 16S ribosomal RNA Propionibacteria Distribution and differentiation of human commensal propionibacterium P. acnes P. avidum P. granulosum P. propionicum distribution Skin +++ +++ +++ - Eye + - - +++ Mouth ++ - + +++ Gut +++ - - - differentiation Esculin - + - - Catalase + -

Retrospective Clinical Trial of Fusidic Acid Versus Petrolatum in the Postprocedure Care of Clean Dermatologic Procedures
Fusidic Acid vs. Petrolatum for Clean Procedures Ann Dermatol Vol. 27, No. 1, 2015 http://dx.doi.org/10.5021/ad.2015.27.1.15 ORIGINAL ARTICLE Retrospective Clinical Trial of Fusidic Acid versus Petrolatum in the Postprocedure Care of Clean Dermatologic Procedures Dong Hun Lee1,2, Dong Young Kim1,3, So Young Yoon1,3, Hyun Sun Park1,2,3, Hyun-Sun Yoon1,2,3, Soyun Cho1,2,3 1Department of Dermatology, Seoul National University College of Medicine, 2Institute of Human-Environment Interface Biology, Seoul National University, 3Department of Dermatology, SMG-SNU Boramae Medical Center, Seoul, Korea Background: Clean dermatologic procedures create wounds Conclusion: Our findings support the hypothesis that the with a low risk of infection (usually up to 5%). Whether the routine prophylactic use of topical antibiotics is not indicated use of topical antibiotics is advocated, with regard to its for clean dermatologic procedures. We recommend the use efficacy and safety issues such as antibiotic resistance and of petrolatum in the postoperative care of clean dermatologic sensitizing potential, is controversial. Fusidic acid, a topical procedures because of its equivalent efficacy and superior antibiotic against gram-positive bacteria, is a rare sensitizer safety profiles. (Ann Dermatol 27(1) 15∼20, 2015) and commonly used in postprocedure care in Korea. Objective: This is a retrospective study aimed at comparing -Keywords- the efficacy and safety between fusidic acid and petrolatum Dermatologic surgical procedures, Fusidic acid, Infection, for the postprocedure care of clean dermatologic procedures. Petrolatum, Wound healing Methods: Patients were treated with either fusidic acid or petrolatum ointment, applied on the wound created during clean dermatologic procedures such as biopsy of the punch, INTRODUCTION incisional, excisional, and shave types. -

Fisher Bioreagents Antibiotics and Antimycotics Catalog
Fisher BioReagents® Antibiotics and Antimycotics In many life science laboratories, the in vitro culturing of bacterial, Optimized for cell culture plant, and animal cells is a routine task. High quality antibiotics and antimycotics from Fisher BioReagents can be used to ensure success- ful growth of cells by eliminating unwanted bacterial strains and fungi while maintaining the health and vitality of the desired cells. Advantages • High quality - antibiotics and antimycotics meet rigorous quality control tests, including verifi cation of potency, purity, and solubility using microbiological and chromatographic methods. • Built for selection - excellent choice of antibiotics for selection of antibiotic resistance genes in both bacterial and mammalian cells. • High purity and stability - ultrapure antibiotics ensure successful growth of target cells and reproducible results. • Maximum convenience - antibiotics and antimycotics come in both sterile powder and liquid forms. Applications • Plant cell culture • Mammalian cell culture • Tissue culture • Genetic marker selection Table 1. Antibiotic modes of action Molecular Catalog No. Product Description Mode of Action Susceptible Organisms Form Size Packaging Weight Inhibitor of protein disulfide isomerase. Interferes with BP2950-1 Bacitracin 1422.7 Gram+ Dry 1g Amber glass bottle building blocks of peptidoglycan bacterial cell wall. Inhibitor of bacterial cell wall synthesis. Eliminates BP2951-1 Cefotaxime Sodium Salt 477.5 Gram- Dry 1g Amber glass bottle Agrobacterium species after inoculation. BP2952- Prokaryotes and higher Crimp top on glass Hygromycin B 527.5 Inhibits protein synthesis. Liquid 1mu 1MU eukaryotes bottle Alters membrane permeability and allows potassium ion BP2949-5 Nystatin 926.1 Yeasts and molds Dry 5g Amber glass bottle leakage. BP2953-1 Paromomycin Sulfate 615.6 Inhibits protein synthesis. -

SEPSIS AMINOGLYCOSIDES Examples: Streptomycin, Gentamicin
SEPSIS AMINOGLYCOSIDES Examples: streptomycin, gentamicin, tobramycin Mechanism of action A bactericidal group of drugs which inhibit bacterial protein synthesis by irreversibly binding bacterial ribosomes. They require entry to Gram negative bacterial cells through outer cell membrane (via porins) and inner cytoplasmic membrane (an oxygen-dependent system) in order to exert their effect. They have difficulty penetrating Gram positive cell walls. They are therefore effective against Gram negative aerobic bacteria but not against anaerobic gram negative bacteria whose cell wall/membranes the antibiotic cannot penetrate. They have limited application against Gram positive bacteria. Synergistic with penicillins - cell wall synthesis inhibitors increase the permeability of the cell wall to aminoglycosides. They do not cross the blood brain barrier and have low concentrations in many tissues. They reach high concentrations in the inner ears and kidneys. Adverse Effects Ototoxicity - accumulates in the endolymph and perilymph of the inner ear causing deafness, tinnitus and vertigo. Increased risk with co-use of loop diuretics and cisplatin. Nephrotoxicity - retention of aminoglycosides by proximal tubular cells disrupts calcium- mediated transport processes resulting in nephrotoxicity. This ranges from mild, reversible renal impairment to severe, irreversible acute tubular necrosis. Dose, frequency and duration of therapy determine the extent of nephrotoxicity. Other adverse effects - allergy, neuromuscular blockade. They cross the placenta and may cause congenital deafness. Gentamicin Prescribing Where possible prescribe gentamicin using the Gentamicin calculator. If critically ill and gentamicin is needed prescribe 5mg/kg actual body weight (max 400mg). If critically ill and known CKD stage V give 2.5mg/kg (max 180mg). Always prescribe gentamicin on the Gentamicin prescription chart. -

Third ESVAC Report
Sales of veterinary antimicrobial agents in 25 EU/EEA countries in 2011 Third ESVAC report An agency of the European Union The mission of the European Medicines Agency is to foster scientific excellence in the evaluation and supervision of medicines, for the benefit of public and animal health. Legal role Guiding principles The European Medicines Agency is the European Union • We are strongly committed to public and animal (EU) body responsible for coordinating the existing health. scientific resources put at its disposal by Member States • We make independent recommendations based on for the evaluation, supervision and pharmacovigilance scientific evidence, using state-of-the-art knowledge of medicinal products. and expertise in our field. • We support research and innovation to stimulate the The Agency provides the Member States and the development of better medicines. institutions of the EU the best-possible scientific advice on any question relating to the evaluation of the quality, • We value the contribution of our partners and stake- safety and efficacy of medicinal products for human or holders to our work. veterinary use referred to it in accordance with the • We assure continual improvement of our processes provisions of EU legislation relating to medicinal prod- and procedures, in accordance with recognised quality ucts. standards. • We adhere to high standards of professional and Principal activities personal integrity. Working with the Member States and the European • We communicate in an open, transparent manner Commission as partners in a European medicines with all of our partners, stakeholders and colleagues. network, the European Medicines Agency: • We promote the well-being, motivation and ongoing professional development of every member of the • provides independent, science-based recommenda- Agency.