Functional Genomic Annotation of Genetic Risk Loci Highlights Inflammation and Epithelial Biology Networks in CKD
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model
Downloaded from http://www.jimmunol.org/ by guest on September 25, 2021 T + is online at: average * The Journal of Immunology , 34 of which you can access for free at: 2016; 197:1477-1488; Prepublished online 1 July from submission to initial decision 4 weeks from acceptance to publication 2016; doi: 10.4049/jimmunol.1600589 http://www.jimmunol.org/content/197/4/1477 Molecular Profile of Tumor-Specific CD8 Cell Hypofunction in a Transplantable Murine Cancer Model Katherine A. Waugh, Sonia M. Leach, Brandon L. Moore, Tullia C. Bruno, Jonathan D. Buhrman and Jill E. Slansky J Immunol cites 95 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html http://www.jimmunol.org/content/suppl/2016/07/01/jimmunol.160058 9.DCSupplemental This article http://www.jimmunol.org/content/197/4/1477.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 25, 2021. The Journal of Immunology Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model Katherine A. -

Interoperability in Toxicology: Connecting Chemical, Biological, and Complex Disease Data
INTEROPERABILITY IN TOXICOLOGY: CONNECTING CHEMICAL, BIOLOGICAL, AND COMPLEX DISEASE DATA Sean Mackey Watford A dissertation submitted to the faculty at the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Gillings School of Global Public Health (Environmental Sciences and Engineering). Chapel Hill 2019 Approved by: Rebecca Fry Matt Martin Avram Gold David Reif Ivan Rusyn © 2019 Sean Mackey Watford ALL RIGHTS RESERVED ii ABSTRACT Sean Mackey Watford: Interoperability in Toxicology: Connecting Chemical, Biological, and Complex Disease Data (Under the direction of Rebecca Fry) The current regulatory framework in toXicology is expanding beyond traditional animal toXicity testing to include new approach methodologies (NAMs) like computational models built using rapidly generated dose-response information like US Environmental Protection Agency’s ToXicity Forecaster (ToXCast) and the interagency collaborative ToX21 initiative. These programs have provided new opportunities for research but also introduced challenges in application of this information to current regulatory needs. One such challenge is linking in vitro chemical bioactivity to adverse outcomes like cancer or other complex diseases. To utilize NAMs in prediction of compleX disease, information from traditional and new sources must be interoperable for easy integration. The work presented here describes the development of a bioinformatic tool, a database of traditional toXicity information with improved interoperability, and efforts to use these new tools together to inform prediction of cancer and complex disease. First, a bioinformatic tool was developed to provide a ranked list of Medical Subject Heading (MeSH) to gene associations based on literature support, enabling connection of compleX diseases to genes potentially involved. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
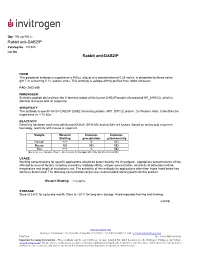
Rabbit Anti-DAB2IP Rabbit Anti-DAB2IP
Qty: 100 μg/400 μL Rabbit anti-DAB2IP Catalog No. 487300 Lot No. Rabbit anti-DAB2IP FORM This polyclonal antibody is supplied as a 400 µL aliquot at a concentration of 0.25 mg/mL in phosphate buffered saline (pH 7.4) containing 0.1% sodium azide. This antibody is epitope-affinity purified from rabbit antiserum. PAD: ZMD.689 IMMUNOGEN Synthetic peptide derived from the C-terminal region of the human DAB2IP protein (Accession# NP_619723), which is identical to mouse and rat sequence. SPECIFICITY This antibody is specific for the DAB2IP (DAB2 interacting protein, AIP1, DIP1/2) protein. On Western blots, it identifies the target band at ~110 kDa. REACTIVITY Reactivity has been confirmed with human DU145, SK-N-MC and rat B49 cell lysates. Based on amino acid sequence homology, reactivity with mouse is expected. Sample Western Immuno- Immuno- Blotting precipitation cytochemistry Human +++ 0 ND Mouse ND ND ND Rat +++ 0 ND (Excellent +++, Good++, Poor +, No reactivity 0, Not applicable N/A, Not Determined ND) USAGE Working concentrations for specific applications should be determined by the investigator. Appropriate concentrations will be affected by several factors, including secondary antibody affinity, antigen concentration, sensitivity of detection method, temperature and length of incubations, etc. The suitability of this antibody for applications other than those listed below has not been determined. The following concentration ranges are recommended starting points for this product. Western Blotting: 1-3 μg/mL STORAGE Store at 2-8°C for up to one month. Store at –20°C for long-term storage. Avoid repeated freezing and thawing. (cont’d) www.invitrogen.com Invitrogen Corporation • 542 Flynn Rd • Camarillo • CA 93012 • Tel: 800.955.6288 • E-mail: [email protected] PI487300 (Rev 10/08) DCC-08-1089 Important Licensing Information - These products may be covered by one or more Limited Use Label Licenses (see the Invitrogen Catalog or our website, www.invitrogen.com). -

Conserved and Novel Properties of Clathrin-Mediated Endocytosis in Dictyostelium Discoideum" (2012)
Rockefeller University Digital Commons @ RU Student Theses and Dissertations 2012 Conserved and Novel Properties of Clathrin- Mediated Endocytosis in Dictyostelium Discoideum Laura Macro Follow this and additional works at: http://digitalcommons.rockefeller.edu/ student_theses_and_dissertations Part of the Life Sciences Commons Recommended Citation Macro, Laura, "Conserved and Novel Properties of Clathrin-Mediated Endocytosis in Dictyostelium Discoideum" (2012). Student Theses and Dissertations. Paper 163. This Thesis is brought to you for free and open access by Digital Commons @ RU. It has been accepted for inclusion in Student Theses and Dissertations by an authorized administrator of Digital Commons @ RU. For more information, please contact [email protected]. CONSERVED AND NOVEL PROPERTIES OF CLATHRIN- MEDIATED ENDOCYTOSIS IN DICTYOSTELIUM DISCOIDEUM A Thesis Presented to the Faculty of The Rockefeller University in Partial Fulfillment of the Requirements for the degree of Doctor of Philosophy by Laura Macro June 2012 © Copyright by Laura Macro 2012 CONSERVED AND NOVEL PROPERTIES OF CLATHRIN- MEDIATED ENDOCYTOSIS IN DICTYOSTELIUM DISCOIDEUM Laura Macro, Ph.D. The Rockefeller University 2012 The protein clathrin mediates one of the major pathways of endocytosis from the extracellular milieu and plasma membrane. Clathrin functions with a network of interacting accessory proteins, one of which is the adaptor complex AP-2, to co-ordinate vesicle formation. Disruption of genes involved in clathrin-mediated endocytosis causes embryonic lethality in multicellular animals suggesting that clathrin-mediated endocytosis is a fundamental cellular process. However, loss of clathrin-mediated endocytosis genes in single cell eukaryotes, such as S.cerevisiae (yeast), does not cause lethality, suggesting that clathrin may convey specific advantages for multicellularity. -

Integrating Single-Step GWAS and Bipartite Networks Reconstruction Provides Novel Insights Into Yearling Weight and Carcass Traits in Hanwoo Beef Cattle
animals Article Integrating Single-Step GWAS and Bipartite Networks Reconstruction Provides Novel Insights into Yearling Weight and Carcass Traits in Hanwoo Beef Cattle Masoumeh Naserkheil 1 , Abolfazl Bahrami 1 , Deukhwan Lee 2,* and Hossein Mehrban 3 1 Department of Animal Science, University College of Agriculture and Natural Resources, University of Tehran, Karaj 77871-31587, Iran; [email protected] (M.N.); [email protected] (A.B.) 2 Department of Animal Life and Environment Sciences, Hankyong National University, Jungang-ro 327, Anseong-si, Gyeonggi-do 17579, Korea 3 Department of Animal Science, Shahrekord University, Shahrekord 88186-34141, Iran; [email protected] * Correspondence: [email protected]; Tel.: +82-31-670-5091 Received: 25 August 2020; Accepted: 6 October 2020; Published: 9 October 2020 Simple Summary: Hanwoo is an indigenous cattle breed in Korea and popular for meat production owing to its rapid growth and high-quality meat. Its yearling weight and carcass traits (backfat thickness, carcass weight, eye muscle area, and marbling score) are economically important for the selection of young and proven bulls. In recent decades, the advent of high throughput genotyping technologies has made it possible to perform genome-wide association studies (GWAS) for the detection of genomic regions associated with traits of economic interest in different species. In this study, we conducted a weighted single-step genome-wide association study which combines all genotypes, phenotypes and pedigree data in one step (ssGBLUP). It allows for the use of all SNPs simultaneously along with all phenotypes from genotyped and ungenotyped animals. Our results revealed 33 relevant genomic regions related to the traits of interest. -

Genetic and Genomic Analysis of Hyperlipidemia, Obesity and Diabetes Using (C57BL/6J × TALLYHO/Jngj) F2 Mice
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Nutrition Publications and Other Works Nutrition 12-19-2010 Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P. Stewart Marshall University Hyoung Y. Kim University of Tennessee - Knoxville, [email protected] Arnold M. Saxton University of Tennessee - Knoxville, [email protected] Jung H. Kim Marshall University Follow this and additional works at: https://trace.tennessee.edu/utk_nutrpubs Part of the Animal Sciences Commons, and the Nutrition Commons Recommended Citation BMC Genomics 2010, 11:713 doi:10.1186/1471-2164-11-713 This Article is brought to you for free and open access by the Nutrition at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Nutrition Publications and Other Works by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. Stewart et al. BMC Genomics 2010, 11:713 http://www.biomedcentral.com/1471-2164/11/713 RESEARCH ARTICLE Open Access Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P Stewart1, Hyoung Yon Kim2, Arnold M Saxton3, Jung Han Kim1* Abstract Background: Type 2 diabetes (T2D) is the most common form of diabetes in humans and is closely associated with dyslipidemia and obesity that magnifies the mortality and morbidity related to T2D. The genetic contribution to human T2D and related metabolic disorders is evident, and mostly follows polygenic inheritance. The TALLYHO/ JngJ (TH) mice are a polygenic model for T2D characterized by obesity, hyperinsulinemia, impaired glucose uptake and tolerance, hyperlipidemia, and hyperglycemia. -

Análise Integrativa De Perfis Transcricionais De Pacientes Com
UNIVERSIDADE DE SÃO PAULO FACULDADE DE MEDICINA DE RIBEIRÃO PRETO PROGRAMA DE PÓS-GRADUAÇÃO EM GENÉTICA ADRIANE FEIJÓ EVANGELISTA Análise integrativa de perfis transcricionais de pacientes com diabetes mellitus tipo 1, tipo 2 e gestacional, comparando-os com manifestações demográficas, clínicas, laboratoriais, fisiopatológicas e terapêuticas Ribeirão Preto – 2012 ADRIANE FEIJÓ EVANGELISTA Análise integrativa de perfis transcricionais de pacientes com diabetes mellitus tipo 1, tipo 2 e gestacional, comparando-os com manifestações demográficas, clínicas, laboratoriais, fisiopatológicas e terapêuticas Tese apresentada à Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo para obtenção do título de Doutor em Ciências. Área de Concentração: Genética Orientador: Prof. Dr. Eduardo Antonio Donadi Co-orientador: Prof. Dr. Geraldo A. S. Passos Ribeirão Preto – 2012 AUTORIZO A REPRODUÇÃO E DIVULGAÇÃO TOTAL OU PARCIAL DESTE TRABALHO, POR QUALQUER MEIO CONVENCIONAL OU ELETRÔNICO, PARA FINS DE ESTUDO E PESQUISA, DESDE QUE CITADA A FONTE. FICHA CATALOGRÁFICA Evangelista, Adriane Feijó Análise integrativa de perfis transcricionais de pacientes com diabetes mellitus tipo 1, tipo 2 e gestacional, comparando-os com manifestações demográficas, clínicas, laboratoriais, fisiopatológicas e terapêuticas. Ribeirão Preto, 2012 192p. Tese de Doutorado apresentada à Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo. Área de Concentração: Genética. Orientador: Donadi, Eduardo Antonio Co-orientador: Passos, Geraldo A. 1. Expressão gênica – microarrays 2. Análise bioinformática por module maps 3. Diabetes mellitus tipo 1 4. Diabetes mellitus tipo 2 5. Diabetes mellitus gestacional FOLHA DE APROVAÇÃO ADRIANE FEIJÓ EVANGELISTA Análise integrativa de perfis transcricionais de pacientes com diabetes mellitus tipo 1, tipo 2 e gestacional, comparando-os com manifestações demográficas, clínicas, laboratoriais, fisiopatológicas e terapêuticas. -

Genetic, Cytogenetic and Physical Refinement of the Autosomal Recessive CMT Linked to 5Q31ð Q33: Exclusion of Candidate Genes I
European Journal of Human Genetics (1999) 7, 849–859 © 1999 Stockton Press All rights reserved 1018–4813/99 $15.00 t http://www.stockton-press.co.uk/ejhg ARTICLE Genetic, cytogenetic and physical refinement of the autosomal recessive CMT linked to 5q31–q33: exclusion of candidate genes including EGR1 Ang`ele Guilbot1, Nicole Ravis´e1, Ahmed Bouhouche6, Philippe Coullin4, Nazha Birouk6, Thierry Maisonobe3, Thierry Kuntzer7, Christophe Vial8, Djamel Grid5, Alexis Brice1,2 and Eric LeGuern1,2 1INSERM U289, 2F´ed´eration de Neurologie and 3Laboratoire de Neuropathologie R Escourolle, Hˆopital de la Salpˆetri`ere, Paris 4Laboratoire de cytog´en´etique, Villejuif 5G´en´ethon, Evry, France 6Service de Neurologie, Hˆopital des Sp´ecialit´es, Rabat, Morocco 7Service de Neurologie, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland 8Service D’EMG et de pathologie neuromusculaire, Hˆopital neurologique Pierre Wertheimer, Lyon, France Charcot-Marie-Tooth disease is an heterogeneous group of inherited peripheral motor and sensory neuropathies with several modes of inheritance: autosomal dominant, X-linked and autosomal recessive. By homozygosity mapping, we have identified, in the 5q23–q33 region, a third locus responsible for an autosomal recessive form of demyelinating CMT. Haplotype reconstruction and determination of the minimal region of homozygosity restricted the candidate region to a 4 cM interval. A physical map of the candidate region was established by screening YACs for microsatellites used for genetic analysis. Combined genetic, cytogenetic and physical mapping restricted the locus to a less than 2 Mb interval on chromosome 5q32. Seventeen consanguineous families with demyelinating ARCMT of various origins were screened for linkage to 5q31–q33. -

Quantitative Proteomics Identify DAB2 As a Cardiac Developmental Regulator That Inhibits WNT/Β-Catenin Signaling
Quantitative proteomics identify DAB2 as a cardiac developmental regulator that inhibits WNT/β-catenin signaling Peter Hofsteena,b,c,1, Aaron M. Robitaillec,d,1, Daniel Patrick Chapmana,b, Randall T. Moonc,d,e,2, and Charles E. Murrya,b,c,f,g,2 aDepartment of Pathology, University of Washington, Seattle, WA 98109; bCenter for Cardiovascular Biology, University of Washington, Seattle, WA 98109; cInstitute for Stem Cell and Regenerative Medicine, University of Washington, Seattle, WA 98109; dDepartment of Pharmacology, University of Washington, Seattle, WA 98109; eHoward Hughes Medical Institute, Chevy Chase, MD 20815; fDepartment of Bioengineering, University of Washington, Seattle, WA 98109; and gDivision of Cardiology, Department of Medicine, University of Washington, Seattle, WA 98109 Contributed by Randall T. Moon, December 11, 2015 (sent for review September 19, 2015; reviewed by Loren J. Field and Sean P. Palecek) To reveal the molecular mechanisms involved in cardiac lineage endocardial-like endothelial cells to differentiate toward the cardiac determination and differentiation, we quantified the proteome of lineage (3). Thus, understanding which proteins are involved in pro- human embryonic stem cells (hESCs), cardiac progenitor cells (CPCs), moting or repressing the WNT/β-catenin signaling pathway is crucial and cardiomyocytes during a time course of directed differentiation for resolving the ambiguities associated with cardiac development. by label-free quantitative proteomics. This approach correctly iden- Here, using label-free quantitation (LFQ) proteomics, we tified known stage-specific markers of cardiomyocyte differentiation, measured protein expression patterns during a time course of including SRY-box2 (SOX2), GATA binding protein 4 (GATA4), and hESC-derived cardiomyocyte differentiation. LFQ proteomics is myosin heavy chain 6 (MYH6). -

(12) Patent Application Publication (10) Pub. No.: US 2015/0072349 A1 Diamandis Et Al
US 201500 72349A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0072349 A1 Diamandis et al. (43) Pub. Date: Mar. 12, 2015 (54) CANCER BOMARKERS AND METHODS OF (52) U.S. Cl. USE CPC. G0IN33/57484 (2013.01); G0IN 2333/705 (2013.01) (71) Applicant: University Health Network, Toronto USPC ......................................... 435/6.12: 435/7.94 (CA) (57) ABSTRACT A method of evaluating a probability a Subject has a cancer, (72) Inventors: Eleftherios P. Diamandis, Toronto diagnosing a cancer and/or monitoring cancer progression (CA); Ioannis Prassas, Toronto (CA); comprising: a. measuring an amount of a biomarker selected Shalini Makawita, Toronto (CA); from the group consisting of CUZD1 and/or LAMC2 and/or Caitlin Chrystoja, Toronto (CA); Hari the group CUZD1, LAMC2, AQP8, CELA2B, CELA3B, M. Kosanam, Maple (CA) CTRB1, CTRB2, GCG, IAPP, INS, KLK1, PNLIPRP1, PNLIPRP2, PPY, PRSS3, REG3G, SLC30A8, KLK3, NPY, (21) Appl. No.: 14/385,449 PSCA, RLN1, SLC45A3, DSP GP73, DSG2, CEACAM7, CLCA1, GPA33, LEFTY1, ZG16, IRX5, LAMP3, MFAP4, (22) PCT Fled: Mar. 15, 2013 SCGB1A1, SFTPC, TMEM100, NPY, PSCA RLN1 and/or SLC45A3 in a test sample from a subject with cancer; (86) PCT NO.: PCT/CA2O13/OOO248 wherein the cancer is pancreas cancer if CUZD1, LAMC2, S371 (c)(1), AQP8, CELA2B, CELA3B, CTRB1, CTRB2, GCG, LAPP (2) Date: Sep. 23, 2014 INS, KLK1, PNLIPRP1, PNLIPRP2, PPY, PRSS3, REG3G, SLC30A8, DSP GP73 and/or DSG2 is selected; the cancer is colon cancer if CEACAM7, CLCA1, GPA33, LEFTY 1 and/ Related U.S. Application Data or ZG16 is selected, the cancer is lung cancer if IRX5, (60) Provisional application No. -

Aneuploidy: Using Genetic Instability to Preserve a Haploid Genome?
Health Science Campus FINAL APPROVAL OF DISSERTATION Doctor of Philosophy in Biomedical Science (Cancer Biology) Aneuploidy: Using genetic instability to preserve a haploid genome? Submitted by: Ramona Ramdath In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Science Examination Committee Signature/Date Major Advisor: David Allison, M.D., Ph.D. Academic James Trempe, Ph.D. Advisory Committee: David Giovanucci, Ph.D. Randall Ruch, Ph.D. Ronald Mellgren, Ph.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: April 10, 2009 Aneuploidy: Using genetic instability to preserve a haploid genome? Ramona Ramdath University of Toledo, Health Science Campus 2009 Dedication I dedicate this dissertation to my grandfather who died of lung cancer two years ago, but who always instilled in us the value and importance of education. And to my mom and sister, both of whom have been pillars of support and stimulating conversations. To my sister, Rehanna, especially- I hope this inspires you to achieve all that you want to in life, academically and otherwise. ii Acknowledgements As we go through these academic journeys, there are so many along the way that make an impact not only on our work, but on our lives as well, and I would like to say a heartfelt thank you to all of those people: My Committee members- Dr. James Trempe, Dr. David Giovanucchi, Dr. Ronald Mellgren and Dr. Randall Ruch for their guidance, suggestions, support and confidence in me. My major advisor- Dr. David Allison, for his constructive criticism and positive reinforcement.