Population Health Improvement Report 2012–2013 Table of Contents Executive Summary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Baystate Health
Baystate Health Baystate Teaching Hospital Wing Community-High Public Payer Physician Organization Baystate Franklin Health Plan Images are sized based on Baystate Medical Center Health New England the entity's portion of operating revenue within their health system. Image size is not comparable between systems. Baystate Medical Practice Operating Net Assets in Profit (Loss) Operating Revenue in Total Margin Millions in Millions Margin Millions Hospital Health System* Baystate Health $2,381.6 $1,101.8 $68.1 2.2% 2.8% Acute Hospital Baystate Franklin Medical Center $102.7 $53.2 $0.6 0.4% 0.6% Baystate Medical Center $1,296.2 $827.7 $99.8 6.6% 7.6% Baystate Noble Hospital $58.4 $16.8 $1.2 2.0% 2.0% Baystate Wing Hospital $85.6 $50.2 ($4.4) -5.7% -5.1% Physician Organization Baystate Medical Practice $307.4 ($43.6) -14.2% -14.2% Baystate Westfield Medical Corporation $12.5 ($5.4) -43.4% -43.4% Health Plan Health New England $833.9 $12.3 1.6% 1.5% * Table includes only the system's affiliated acute hospitals, physician organizations, and health plans. System totals may also include non-acute hospitals, other health care providers, other owned organizations, and consolidating eliminations. www.chiamass.gov CENTER FOR HEALTH INFORMATION AND ANALYSIS | www.chiamass.gov CHIA Berkshire Health Systems Community-High Public Payer Physician Organization Images are sized based on the entity's portion of Berkshire Medical Center Fairview Hospital operating revenue within their health system. Image size is not comparable between systems. Berkshire Faculty -

Lawrence General Hospital
Massachusetts Hospital Payment Variation 2015 2016 Share of # Hospital Relative Relative Commercial MA Acute Hospital Commercial Relative Price (Weighted Average 2016) Price Price Payments Statewide Results Published By CHIA February 2018 1 Baystate Noble 0.681 0.682 0.2% Baystate Noble Hospital 2 Holyoke Medical Center 0.722 0.728 0.2% Holyoke Medical Center 3 Lawrence General 0.754 0.736 0.4% Lawrence General Hospital 4 Anna Jaques 0.756 0.743 0.5% Anna Jaques Hospital 5 Baystate Wing 0.749 0.752 0.2% Baystate Wing Hospital 6 Cambridge Health Alliance 0.797 0.754 0.6% Cambridge Health Alliance 7 BIDH - Milton 0.760 0.757 0.4% Beth Israel Deaconess- Milton 8 Massachusetts Eye & Ear 0.833 0.760 Massachusetts Eye & Ear 9 Heywood Hospital 0.752 0.763 0.4% Heywood Hospital 10 Signature Brockton 0.785 0.787 0.7% Signature Brockton Hospital 11 Mercy Medical Center 0.806 0.796 0.6% Mercy Medical Center 12 HealthAlliance 0.781 0.804 0.4% HealthAlliance Hospital 80% of Average 13 Emerson 0.846 0.824 1.1% Emerson Hospital 14 Steward Morton 0.855 0.837 0.4% Steward Morton Hospital 15 Milford Regional 0.840 0.840 1.1% Milford Regional Medical Center 16 Lowell General 0.822 0.850 1.6% Lowell General Hospital 85% of Average 17 Northeast Beverly 0.867 0.851 1.3% Northeast Hospital 18 MetroWest 0.856 0.853 1.0% MetroWest Medical Center 19 Steward Holy Family 0.859 0.857 0.7% Steward Holy Family Hospital 20 Winchester Hospital 0.892 0.865 1.6% Beth Israel Deaconess - Plymouth 21 BIDH - Plymouth 0.861 0.865 0.8% Winchester Hospital Underpaid Hospitals -

Masshealth Enrollment Guide Your Choices Starting JULY 2021
MassHealth Enrollment Guide Your Choices Starting JULY 2021 LEARN about health plans COMPARE health plans ENROLL in a health plan COMMONWEALTH OF MASSACHUSETTS | Executive Office of Health and Human Services We are here to help We speak your language If you need an interpreter or translation help, please call the MassHealth Customer Service Center. Questions? www.mass.gov/masshealth MassHealth Customer Service Center (800) 841-2900 TTY: (800) 497-4648 for people who are deaf, hard of hearing, or speech disabled. Monday–Friday 8:00 a.m.–5:00 p.m. Hello and welcome MassHealth is the Medicaid program in Massachusetts. We have health plans to choose from so you can get the health care you need. Please read this guide to learn about the plans and choose the one that’s best for you. This guide will help you... Learn Learn about the health plans available in your area and how to choose a provider. Compare Compare health plans in your area and choose the one that’s right for you. Enroll Enroll in a health plan or change to a different health plan. Let’s enroll in a health plan. i Is this guide for you? Certain members in the MassHealth program will need to enroll in a health plan. Use this guide if you ■ Are under 65 ■ Do not have other insurance (including Medicare) ■ Live in the community (for example, not in a nursing facility), and ■ Are in MassHealth Standard, CommonHealth, CarePlus, or Family Assistance. For information about MassHealth coverage, visit www.mass.gov/masshealth. Members described below are not eligible for the health plan options described in this guide. -

Wayfair Preferred (Narrow) Network Plan Hospitals
Wayfair Preferred (Narrow) Network Hospitals Hospital Name City State Addison Gilbert Hospital Gloucester MA Anna Jaques Hospital Newburyport MA BayRidge Hospital (acute psychiatric hospital) Lynn MA Beth Israel Deaconess Medical Center—Boston Boston MA Beth Israel Deaconess Hospital—Milton Milton MA Beth Israel Deaconess Hospital—Needham Campus Needham MA Beth Israel Deaconess Hospital—Plymouth Plymouth MA Beverly Hospital Beverly MA Boston Children’s Hospital Boston MA Boston Medical Center Boston MA Brigham and Women’s/Mass General Health Care Center at Patriot Place Foxborough MA Cambridge Health Alliance—Cambridge Campus Cambridge MA Cambridge Health Alliance—Somerville Campus Somerville MA Cambridge Health Alliance—Whidden Campus Everett MA Carney Hospital Dorchester MA Clinton Hospital Clinton MA Cooley Dickinson Hospital Northampton MA Emerson Hospital Concord MA Faulkner Hospital Jamaica Plain MA Good Samaritan Medical Center Brockton MA HealthAlliance Hospitals—Burbank Campus Fitchburg MA HealthAlliance Hospitals—Leominster Campus Leominster MA Heywood Hospital Gardner MA Holyoke Medical Center Holyoke MA Lahey Hospital and Medical Center Burlington MA Hospital Name City State Lahey Medical Center Peabody MA Lawrence General Hospital Lawrence MA Lawrence Memorial Hospital Medford MA Lowell General Hospital (includes the campus Lowell MA formerly known as Saints Medical Center) Massachusetts Eye and Ear®´ Infirmary Boston MA Mass General/North Shore Center for Outpatient Care Danvers MA Melrose-Wakefield Hospital Melrose MA Mercy -

Health Care System ACUTE INPATIENT HOSPITALS
A B C D E 1 ACUTE INPATIENT HOSPITALS PARTICIPATING IN MASSHEALTH (June 2021) Has Inpatient 2 Health Care System Acute Inpatient Hospital Town Psychiatric Unit? 3 Beth Israel Lahey Health Anna Jaques Hospital Newburyport X 4 Heywood Healthcare Athol Hospital Athol 5 Baystate Health Baystate Franklin Medical Center Greenfield X 6 Baystate Health Baystate Medical Center Springfield X 7 Baystate Health Baystate Noble Hospital Westfield X 8 Baystate Health Baystate Wing Hospital Palmer X 9 Berkshire Health Systems Berkshire Fairview Hospital Great Barrington 10 Berkshire Health Systems Berkshire Medical Center Pittsfield X 11 Beth Israel Lahey Health Beth Israel Deaconess Hospital - Milton Milton 12 Beth Israel Lahey Health Beth Israel Deaconess Hospital - Needham Needham 13 Beth Israel Lahey Health Beth Israel Deaconess Hospital - Plymouth Plymouth X 14 Beth Israel Lahey Health Beth Israel Deaconess Medical Center Boston X 15 Beth Israel Lahey Health Beverly Hospital (aka Northeast Health) Beverly X 16 Boston Children's Hospital Boston X 17 Boston Medical Center Boston 18 MassGeneralBrigham Brigham & Women's Hospital Boston 19 MassGeneralBrigham Brigham and Women's Faulkner Hospital Boston X 20 Cambridge Health Alliance Cambridge Hospital Cambridge X 21 Cape Cod Healthcare Cape Cod Hospital Hyannis X 22 Steward Health Care Carney Hospital Boston X 23 MassGeneralBrigham Cooley Dickinson Hospital Northampton X 24 Dana Farber Cancer Institute Boston 25 Emerson Hospital Concord X 26 Cambridge Health Alliance Everett Hospital Everett X 27 Cape -
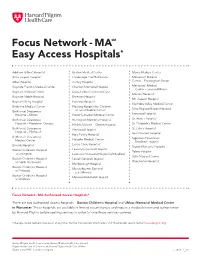
Focus Network - MASM Easy Access Hospitals*
Focus Network - MASM Easy Access Hospitals* Addison Gilbert Hospital Boston Medical Center Mercy Medical Center Anna Jaques Hospital Cambridge Health Alliance Metrowest Medical Athol Hospital Carney Hospital Center – Framingham Union Baystate Franklin Medical Center Charlton Memorial Hospital Metrowest Medical Center – Leonard Morse Baystate Medical Center Dana-Farber Cancer Institute Morton Hospital Baystate Noble Hospital Emerson Hospital Mt. Auburn Hospital Baystate Wing Hospital Fairview Hospital Nashoba Valley Medical Center Berkshire Medical Center Floating Hospital for Children New England Baptist Hospital Beth Israel Deaconess at Tufts Medical Center Hospital – Milton Good Samaritan Medical Center Norwood Hospital Beth Israel Deaconess Harrington Memorial Hospital St. Anne’s Hospital Hospital – Needham Campus Health Alliance – Clinton Hospital St. Elizabeth’s Medical Center Beth Israel Deaconess Heywood Hospital St. Luke’s Hospital Hospital – Plymouth Holy Family Hospital Saint Vincent Hospital Beth Israel Deaconess Holyoke Medical Center Signature Healthcare Medical Center Brockton Hospital Lahey Clinic Hospital Beverly Hospital Sturdy Memorial Hospital Lawrence General Hospital Boston Children’s Hospital Tobey Hospital at Lexington Lawrence Memorial Hospital of Medford Tufts Medical Center Boston Children’s Hospital Lowell General Hospital at North Dartmouth Winchester Hospital Marlborough Hospital Boston Children’s Hospital Massachusetts Eye and at Peabody Ear Infirmary Boston Children’s Hospital Melrose-Wakefield Hospital at Waltham Focus Network - MA Authorized Access Hospitals* There are two Authorized Access hospitals – Boston Children’s Hospital and UMass Memorial Medical Center in Worcester. These hospitals are available in limited circumstances and require a medical review and authorization by Harvard Pilgrim before seeking services in order to have those services covered. *Changes to our network may occur at any time. -

Low Price Hospitals
Health Policy Commission Public Hearing Modification of the 2018 Health Care Cost Growth Benchmark Wednesday, March 8, 2017, 1:00pm 50 Milk Street, 8th Floor Boston, MA 02109 Testimony Steward Health Care System From 2013-2015, The Highest Priced Hospitals Experienced Significant Growth in Inpatient Discharges While Low Priced Hospitals Lost Volume, Yet Remained Efficient Highest Price Hospitals Low Price Hospitals 317,000 2013-2015 488,000 2013-2015 316,305 486,042 316,000 486,000 + 4,143 - 8,973 484,000 315,000 482,000 314,000 480,000 313,000 478,000 312,162 477,069 312,000 476,000 311,000 474,000 310,000 472,000 2013 2015 2013 2015 17 Hospitals with Avg. 46 Hospitals with Price of 1.4 Avg. Price of 1.0 Source: CHIA Inpatient Case Mix Data 2013-2015, CHIA Relative Price 2014 Note: Highest Priced hospitals are defined as those with the 75% highest Relative Prices in 2014 On Average, Every Discharge That Takes Place at a High Price Provider Costs the System Over $9,000 More Than If It Took Place At A Low Price, High Quality Provider $25,000 Weighted Average WAPR $22,491 $20,000 $15,000 $13,265 $10,000 $5,000 $0 High Price Low Price Boston Hospitals Account for Nearly Half of All Hospital Commercial Reimbursements Boston Teaching Beth Israel Deaconess Medical Center Share of Commercial Payments by Payer Brigham and Women's Hospital Massachusetts General Hospital Tufts Medical Center 2014 Boston Medical Center Boston Children's Hospital Dana-Farber Cancer Institute Massachusetts Eye and Ear Infirmary Brigham and Women's Faulkner Hospital -

2019 Community Health Needs Assessment
2019 Community Health Needs Assessment 0 Mission Statement Tufts Medical Center (Tufts MC) is committed to improving the health and wellbeing of the communities we serve. As part of that mission, Tufts MC strives to reduce both health disparities and health inequities in those communities. We seek to identify current and emerging health needs, collaborate with community partners, provide culturally and linguistically appropriate health services and resources, and address community health needs through education, prevention, and treatment. Background The Medical Center is committed not only to its role in providing the highest quality care to its patients and their families, but also to its role as an anchor institution in Boston. In addition to the life-saving care that takes place within its walls, Tufts Medical Center supports impactful work in its partner communities. That work is guided by the findings of our triennial Community Health Needs Assessment (CHNA). In order to ensure that Tufts MC remains at the forefront of the effort to improve the health of community members, we must understand what issues and systems most affect the health of these communities. To that end, the CHNA is an opportunity to engage community members and to seek their input to inform our efforts over the ensuing three years. With an emphasis on the Boston neighborhoods of Chinatown, Dorchester, South Boston, and the South End, as well as the City of Quincy and the Greater Boston Asian community, Tufts MC combines the invaluable insights and contributions offered by community members with an analysis of available public health data in order to identify health priorities in each of these communities. -

Choicenet Tiered Hospitals – 2020
HARVARD PILGRIM’S ChoiceNet Tiered Hospitals – 2020 ChoiceNet, our tiered provider network, includes thousands of Harvard Pilgrim’s participating doctors and clinicians, plus 184 hospitals, who have met Harvard Pilgrim’s high standards for providing quality care. Using national quality benchmarks, as well as plan medical expense information, we placed participating hospitals in Tier 1, Tier 2 or Tier 3. You will pay different cost sharing based on a provider’s assigned benefit tier.1 When you see participating providers in a lower tier, you’ll pay If you have established relationships with certain doctors, you’ll less. You pay more when you receive services from higher tier want to find out what tiers they are in before receiving care from providers. Refer to your Harvard Pilgrim Schedule of Benefits them. Just because doctors are affiliated with certain hospitals, to determine your plan’s actual cost sharing. it doesn’t mean that they’ll have the same tier level. To find your doctors’ tiers, use the provider search tool at harvardpilgrim.org or call us at (800) 848-9995 for assistance. If you’re already a Harvard Pilgrim member, call (888) 333-4742. Participating hospitals and their tiers MASSACHUSETTS MASSACHUSETTS (CONTINUED) Hospital Tier Hospital Tier Anna Jaques Hospital 1 Brigham and Women’s Faulkner Hospital 2 Athol Memorial Hospital 1 Brigham and Women’s Hospital Foxboro 1 Baystate Franklin Medical Center 2 Brockton Hospital 1 Baystate Medical Center 1 Cape Cod Hospital 3 Baystate Wing Hospital 1 Carney Hospital 2 Berkshire Medical -

For Immediate Release Contact
FOR IMMEDIATE RELEASE CONTACT: Chris Murphy Steward Health Care 617-419-4729 [email protected] Andrew Davis named President of Carney Hospital Dorchester, MA, April 24, 2012 – Today, Steward Health Care System LLC (Steward) announced that Andrew Davis will assume the role of President of Carney Hospital effective May 7, 2012. “Andrew is an experienced hospital leader with a strong track record of success,” said Josh Putter, Chief Operating Officer at Steward. “He is the ideal person to implement the Steward integrated care model in Dorchester and position Carney for the future.” Prior to joining Steward, Davis was the Chief Executive Officer of Davis Regional Medical Center in Statesville, NC. Previous, he acted as Chief Executive Officer of Sandhills Regional Medical Center in Hamlet, NC. Davis also served as the Chief Operating Officer at a hospital in NC and the Chief Financial Officer at a hospital in AR. Davis holds a B.S. in Accounting and an MBA from Troy University and is a Certified Public Accountant. “I am thrilled to have the opportunity to join the talented and dedicated staff at Carney Hospital,” said Davis. “I am looking forward to working with them to make Carney the hospital of choice for residents of Dorchester.” About Steward Health Care Steward Health Care is the largest fully integrated community care organization and community hospital network in New England. Headquartered in Boston, Steward is the third largest employer in MA with more than 17,000 employees serving more than one million patients annually in 85 communities. Hospitals in the system include Saint Anne’s in Fall River, Holy Family Hospital in Methuen, St. -

Anna Jaques Hospital - Newburyport, MA 25,752 $25,357,881 62,725 2.44
MHDC Emergency Dept Visits FY2012 Massachusetts Hospitals Average Total LOS Los HOSPITAL Visits Total Charges (Hours) (Hours) Anna Jaques Hospital - Newburyport, MA 25,752 $25,357,881 62,725 2.44 Athol Memorial Hospital - Athol, MA 9,942 $22,184,229 27,336 2.75 Baystate Health - Baystate Medical Center - Springfield, MA 79,890 $110,781,883 369,053 4.62 Baystate Health - Franklin Medical Center - Greenfield, MA 23,799 $36,281,235 88,358 3.71 Baystate Health - Mary Lane Hospital - Ware, MA 13,670 $17,675,008 32,210 2.36 Berkshire Health Systems - Berkshire Medical Center - Pittsfield, MA 44,993 $84,441,787 151,409 3.37 Berkshire Health Systems - Fairview Hospital - Great Barrington, MA 11,797 $21,370,183 28,426 2.41 Beth Israel Deaconess Hospital - Needham - Needham, MA 11,441 $17,369,676 33,162 2.90 Beth Israel Deaconess Medical Center - Boston, MA 28,164 $60,592,428 115,948 4.12 Beth Isreal Deaconess Hospital - Milton - Milton, MA 19,756 $33,603,250 59,107 2.99 Boston Children's Hospital - Boston, MA 46,782 $41,846,070 157,129 3.36 Boston Medical Center - Boston, MA 102,507 $125,855,189 309,132 3.02 MHDC Emergency Dept Visits FY2012 Massachusetts Hospitals Average Total LOS Los HOSPITAL Visits Total Charges (Hours) (Hours) Brigham and Women's - Faulkner Hospital - Boston, MA 19,204 $43,652,476 48,592 2.53 Brigham and Women's Hospital - Boston, MA 36,583 $90,621,008 128,676 3.52 Cambridge Health Alliance - Cambridge Hospital - Cambridge, MA 28,906 $40,967,627 88,037 3.05 Cambridge Health Alliance - Somerville Campus 19,157 $25,430,134 -

Internal Medicine Residency Program
Carney Hospital Internal Medicine Residency Program Carney Hospital is a 159-bed community teaching hospital in Dorchester, MA affiliated with Tufts University School of Medicine. Carney Hospital: A History of Firsts In 1877, the first outpatient department in Boston was established by the hospital. The first abdominal surgery in the USA was carried out in the hospital in 1882. The same year, the first ovariectomy in Boston was carried out in Carney. The first Catholic nursing school in New England was opened in 1892. In 1920 the hospital introduced the first residency training program in Boston. In 1950 the first plastic hip operation in the US was performed at Carney Hospital. In 1974, Carney Hospital provided the first medical emergency rooftop helistop in Massachusetts. In March 2020, Carney Hospital was announced as the first COVID19 only hospital in the US. Carney Hospital Steward Health Care Carney Hospital https://youtu.be/9u0dDa 4ajTY Carney Hospital ER Carney Hospital Internal Medicine Training Program Carney Hospital Internal Meidcine Training Program https://www.youtube.co m/watch?v=7XybNwR6 4nQ&list=PLD7RUGfnUt HoX8NC4- O9T60Vuoaza82KZ&ind ex=13&t=5s&fbclid=Iw AR3GbaIupGqbudHvdpr -Wpy- 4YtDO24aMXv2WXwL0 Affiliated Sites St. Elizabeth’s Medical Center Lemuel Shattuck Hospital Affiliated Sites Tufts Medical Center Program Structure Starting from the academic year 2020/2021 the program has switched to “ 4 + 2 ” structure. Interns and residents will spend 4 weeks on inpatient services (wards or ICU) followed by two