The Neural Basis of Sodium Appetite
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

How Does the Brain Sense Osmolality?
SCIENCE IN RENAL MEDICINE www.jasn.org How Does the Brain Sense Osmolality? Joseph G. Verbalis Professor of Medicine and Physiology, Georgetown University School of Medicine, Washington, DC ABSTRACT For nearly 60 years, we have known that the brain plays a pivotal role in regulating sponses to hyperosmolality in experi- the osmolality of body fluids. Over this time period, scientists have determined the mental animals3 and in human subjects structure and function of arginine vasopressin and its receptors, the role of the with brain damage that infarcts the re- posterior pituitary as a storage site, and the determinants of vasopressin release. gion around the OVLT, who typically are The cellular mechanisms by which the kidney responds to vasopressin are also well unable to maintain normal plasma os- understood. One area that remains unclear is the neural mechanisms underlying molalities even under basal conditions.4 osmoreception. New findings have implicated the TRPV family of cation channels as In contrast to the effects of such lesions osmo-mechanoreceptors that may mediate the neuronal responses to changes in to eliminate both osmotically stimulated systemic tonicity. This topic is reviewed here. thirst and AVP secretion, diabetes insip- idus caused by destruction of the magno- J Am Soc Nephrol 18: 3056–3059, 2007. doi: 10.1681/ASN.2007070825 cellular AVP neurons in the supraoptic (SON) and paraventricular (PVN) nu- clei eliminates dehydration-induced Body fluid homeostasis is directed at WHERE ARE OSMORECEPTORS AVP secretion but not thirst, clearly in- maintaining the stability of the osmo- LOCATED? dicating that osmotically stimulated lality of body fluids (osmotic ho- thirst must be generated proximally to meostasis) and the intravascular blood The pioneering investigations of Verney the AVP-secreting cells themselves (Fig- volume (volume homeostasis). -

The Effect of High Salt Intake on Osmoreceptor Gain in Salt
The Effect of High Salt Intake on Osmoreceptor Gain in Salt-Sensitive Hypertension David Levi Integrated Program in Neuroscience McGill University Montreal, QC August 2018 A thesis submitted to McGill University in partial fulfillment of the requirement of the degree of Master of Science. © David Levi 2018 Table of Contents Abstract ....................................................................................................................................... i Resumé ....................................................................................................................................... ii Acknowledgements .................................................................................................................. iii Preface and Contribution of Authours .................................................................................. iv Symbols and Abbreviations ..................................................................................................... v 1. Introduction ............................................................................................................................... 1 1.1 General Introduction to Hypertension .............................................................................. 1 1.1.1 Epidemiology of Hypertension ...................................................................................... 1 1.1.2 Risk Factors of Hypertension ......................................................................................... 2 1.2 Homeostasis of Blood Pressure -
![L7-Renal Regulation of Body Fluid [PDF]](https://docslib.b-cdn.net/cover/6571/l7-renal-regulation-of-body-fluid-pdf-746571.webp)
L7-Renal Regulation of Body Fluid [PDF]
Iden8fy and describe the role of the Sensors and Objectives Effectors in the Abbreviations renal regulaon of body fluid volume ADH An8diurec hormone & osmolality ECF Extracellular fluid ECV Effec8ve Circulang Iden8fy the site and Volume describe the Describe the role of ANF Atrial natriure8c factor influence of the kidney in aldosterone on regulaon of body ANP ATRIAL NATRIURETIC PEPTIDE reabsorp8on of Na+ fluid volume & in the late distal osmolality tubules. PCT Proximal convoluted tubules AVP arginine vasopressin Understand the role of ADH in the reabsorp8on of water and urea Mind map Blood volume remains exactly constant despite extreme changes in daily fluid intake and the reason for that is : 1- slight change in blood volume ! Renal regulaNon of marked change in Extra Cellular cardiac output Volume Is a reflex 2- a slight change mechanism in RegulaNon of ECF Thus, regulaon of in cardiac output which variables volume = Na+ also dependent !large change in reflecng total RegulaNon of body upon blood pressure body sodium and Na+= RegulaNon BP baroreceptors. 3-slight change in ECV are monitor by blood pressure ! appropriate sensor large change in (receptors) URINE OUTPUT . Con. Blood Volume regulation : Sensors Effectors Affecng 1- Rennin angiotensin, aldosterone. 1- Caro8d sinus Urinary Na excre8on. 2- ADH ( the result will cause a change in NA+ and water excre8on either 3- Renal sympathe8c nerve by increasing it or 2- Volume receptors decreasing it ) . (large vein, atria, intrarenalartery) 4- ANP Con. Blood Volume regulation : Cardiac atria Low pressure receptors Pulmonary vasculature Central vascular sensors Carod sinus Sensors in the CNS High pressure receptors AorNc arch Juxtaglomerular apparatus (renal afferent arteriole) Sensors in the liver ECF volume Receptors Con. -
Study Guide Renal Module
STUDY GUIDE RENAL MODULE 2nd Professional MBBS (Session 2020-21) Prepared by: Dr Sadaf Durrani 1 CONTENTS List of Abbreviations 2 Module Planning Committee 3 Distribution of Academic Activities among different Disciplines 4 Introduction to Renal Module and Themes 5 General Learning Outcomes 6 Individual Themes 7-26 o Introduction o Learning objectives o List of Practicals o List of SGDs o List of DSL / Others o List of dissection and FDTs o Timetable (with designated teachers and venues) Books and other reading resources 27 Block Assessments 28 o MCQs o OSPE 2 LIST OF ABBREVIATIONS Anat-L Anatomy Lecture MCQs Multiple Choice Questions Anat-SGD Small Group Discussion in Anatomy Neph-L Nephrology lecture Bio-L Biochemistry Lecture Path-L Pathology Lecture Bio-P Biochemistry Practical Phar-L Pharmacology Lecture Bio-SGD Small Group Discussion in Biochemistry Phy-L Physiology Lecture CMed Community Medicine Phy-P Physiology Practical DSL Directed Self Learning Phy-SGD Small Group Discussion in Physiology FDT Film/Demonstration/Tutorial SDL Self-Directed learning FMed Forensic Medicine SAQs Short Essay Questions Histo-P Histology Practical SGD Small Group Discussion IPS Islamiyat/Pak Studies Surg-L General surgery lecture OSPE Objectively Structured Practical Examination SLRC Self Learning Resource Center Professionalism and communication skills, Research, Identity formation, Management and leadership, PRIME Ethics 3 MODULE PLANNING COMMITTEE Patron Prof. Dr. Mahmood Aurangzeb Dean, KMC Chairman Prof. Dr. Farooq Ahmed Director Medical Education, KMC Course Coordinator Prof. Dr. Ubaid ur Rahman Department of Biochemistry, KMC Module Director Associate Prof. Dr. Sadaf Durrani Department of Biochemistry, KMC Member Prof. Dr. Mudassir Ahmad Khan Chairman, Department of Biochemistry, KMC Member Prof. -

Hypothalamic Disconnection Caudal to Paraventricular Nucleus Affects Cardiovascular and Drinking Responses to Central Angiotensin II and Carbachol
BRAIN RESEARCH 1388 (2011) 100– 108 available at www.sciencedirect.com www.elsevier.com/locate/brainres Research Report Hypothalamic disconnection caudal to paraventricular nucleus affects cardiovascular and drinking responses to central angiotensin II and carbachol Lilia Simone Urzedo–Rodrigues, Tatiane Depieri, Anderson Julio Cherobino, Oswaldo U. Lopes, José V. Menani, Débora S.A. Colombari⁎ Department of Physiology and Pathology, School of Dentistry, UNESP—São Paulo State University Araraquara, SP, Brazil ARTICLE INFO ABSTRACT Article history: The paraventricular nucleus of the hypothalamus (PVN) is an important area of the brain Accepted 8 March 2011 involved in the control of cardiovascular system and fluid-electrolyte balance. In the present Available online 13 March 2011 study we evaluated the effects of hypothalamic disconnection (HD) caudal to PVN in the pressor and dipsogenic responses induced by intracerebroventricular (icv) injections of Keywords: angiotensin II (ANG II) or carbachol (cholinergic agonist). Male Holtzman rats (280–320 g) Blood pressure with a stainless steel cannula implanted into the lateral ventricle and submitted to sham or Thirst HD surgery were used. HD (2 or 15 days) reduced the pressor responses to ANG II (50 ng/1 μl) Paraventricular nucleus icv (8±3 and 11±3 mm Hg, respectively, vs. sham: 23±3 and 21±2 mm Hg) or carbachol of hypothalamus (4 nmol/1 μl) icv (8±2 and 21±3 mm Hg, respectively, vs. sham: 33±3 and 33±3 mm Hg), Vasopressin without changing baseline arterial pressure. Acutely (2–4 days), HD also reduced water Knife-cut intake to icv ANG II (3.3±2.2 vs. -

Renal Physiology a Clinical Approach
Renal Physiology A Clinical Approach LWBK1036-FM_pi-xiv.indd 1 12/01/12 1:16 PM LWBK1036-FM_pi-xiv.indd 2 12/01/12 1:16 PM Renal Physiology A Clinical Approach John Danziger, MD Instructor in Medicine Division of Nephrology Beth Israel Deaconess Medical Center Harvard Medical School Boston, MA Mark Zeidel, MD Herrman L. Blumgart Professor of Medicine Harvard Medical School Physician-in-Chief and Chair, Department of Medicine Beth Israel Deaconess Medical Center Boston, MA Michael J. Parker, MD Assistant Professor of Medicine Division of Pulmonary, Critical Care, and Sleep Medicine Beth Israel Deaconess Medical Center Senior Interactive Media Architect Center for Educational Technology Harvard Medical School Boston, MA Series Editor Richard M. Schwartzstein, MD Ellen and Melvin Gordon Professor of Medicine and Medical Education Director, Harvard Medical School Academy Vice President for Education and Director, Carl J. Shapiro Institute for Education Beth Israel Deaconess Medical Center Boston, MA LWBK1036-FM_pi-xiv.indd 3 12/01/12 1:16 PM Acquisitions Editor: Crystal Taylor Product Managers: Angela Collins and Jennifer Verbiar Marketing Manager: Joy Fisher-Williams Designer: Doug Smock Compositor: Aptara, Inc. Copyright © 2012 Lippincott Williams & Wilkins, a Wolters Kluwer business. 351 West Camden Street Two Commerce Square Baltimore, MD 21201 2001 Market Street Philadelphia, PA 19103 Printed in China All rights reserved. This book is protected by copyright. No part of this book may be reproduced or trans- mitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. -

Regulation of Water and Electrolyte Metabolism During Dehydration and Rehydration in Camels Ali Abdullah Al-Qarawi Iowa State University
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 1997 Regulation of water and electrolyte metabolism during dehydration and rehydration in camels Ali Abdullah Al-Qarawi Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Animal Sciences Commons, Physiology Commons, and the Veterinary Physiology Commons Recommended Citation Al-Qarawi, Ali Abdullah, "Regulation of water and electrolyte metabolism during dehydration and rehydration in camels " (1997). Retrospective Theses and Dissertations. 11766. https://lib.dr.iastate.edu/rtd/11766 This Dissertation is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. INFORMATION TO USERS This manuscript has been reproduced from the microfilm master. UMI films the text directly fi'om the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter face, while others may be fi'om any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper aligxmient can adversely affect reproduction. In the unlikely event that the author did not send UMI a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. -

Selectively Inhibiting the Median Preoptic Nucleus Attenuates Angiotensin II and Hyperosmotic- Induced Drinking Behavior and Vasopressin Release in Adult Male Rats
New Research Integrative Systems Selectively Inhibiting the Median Preoptic Nucleus Attenuates Angiotensin II and Hyperosmotic- Induced Drinking Behavior and Vasopressin Release in Adult Male Rats Alexandria B. Marciante, Lei A. Wang, George E. Farmer, and J. Thomas Cunningham https://doi.org/10.1523/ENEURO.0473-18.2019 Department of Physiology and Anatomy, University of North Texas Health Science Center, Fort Worth, TX 76107 Visual Abstract The median preoptic nucleus (MnPO) is a putative integrative region that contributes to body fluid balance. Activation of the MnPO can influence thirst, but it is not clear how these responses are linked to body fluid homeostasis. We used designer receptors exclusively activated by designer drugs (DREADDs) to determine the Significance Statement The median preoptic nucleus (MnPO) is an important regulatory center that influences thirst, cardiovascular and neuroendocrine function. Activation of different MnPO neuronal populations can inhibit or stimulate water intake. However, the role of the MnPO and its pathway-specific projections during angiotensin II (ANG II) and hyperosmotic challenges still have not yet been fully elucidated. These studies directly address this by using designer receptors exclusively activated by designer drugs (DREADDs) to acutely and selectively inhibit pathway-specific MnPO neurons, and uses techniques that measure changes at the protein, neuronal, and overall physiologic and behavioral level. More importantly, we have been able to demonstrate that physiologic challenges related to extracellular (ANG II) or cellular (hypertonic saline) dehydration activate MnPO neurons that may project to different parts of the hypothalamus. March/April 2019, 6(2) e0473-18.2019 1–19 New Research 2 of 19 role of the MnPO in drinking behavior and vasopressin release in response to peripheral angiotensin II (ANG II) or 3% hypertonic saline (3% HTN) in adult male Sprague Dawley rats (250–300 g). -

Fluid Balance
CLINICAL systems of life Homeostasis part 4: fluid balance fiG 1. HoRmoNal CoNtRol of tHe kiDNey By NeGative feeDBaCk looPs Authors Brendan Docherty, msc, PGCe, RN, l Chemical and bioelectrical distributions within and is patient access manager, Executive Director’s between cells and tissues; Unit, Prince of Wales Hospital, Sydney, Australia; l Heat, hormone and nutrient distribution around Colette foudy, RN, GradDip, is clinical care the tissues; coordinator, intensive care unit, St George Private l Carriage of waste products to the appropriate Hospital, Sydney, Australia. organ for excretion – generally through the liver and renal system. In this article, the last in a four-part series, we explore fluid maintenance with particular reference to Homeostatic control disorders of the pituitary gland. Fluid management When fluid volume decreases, the concentration techniques and related nursing care are also covered. of sodium in the blood will increase (increased Body fluids are mainly water and electrolytes, and osmolarity, the amount of solute per unit volume), the three main organs that regulate fluid balance which in turn stimulates the hypothalamus (Tortora are the brain, the adrenal glands and the kidneys and Grabowski, 2002). The hypothalamus is an (Tortora and Grabowski, 2002). One-third of the total osmoreceptor – a sensory end organ that reacts to is circulatory fluid, sometimes known as extracellular changes in osmotic pressure and has an effect on fluid (ECF); the remainder is intracellular fluid (ICF) the pituitary gland. contained within cells (Docherty and McIntyre, 2002; In response, the posterior pituitary gland releases Edwards 2001). The anatomy and physiology of antidiuretic hormone (ADH, sometimes called homeostasis are covered in part one of this series. -
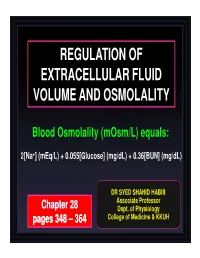
Regulation of Extracellular Fluid Volume and Osmolality
REGULATION OF EXTRACELLULAR FLUID VOLUME AND OSMOLALITY Blood Osmolality (mOsm/L) equals: 2[Na +] (mEq/L) + 0.055[Glucose] (mg/dL) + 0.36[BUN] (mg/dL) DR SYED SHAHID HABIB Associate Professor Chapter 2828 Dept. of Physiology pages 348 ––364364 College of Medicine & KKUH OBJECTIVES At the end of this lecture you should be able to: • Identify and describe the role of the Sensors and Effectors in the renal regulation of body fluid volume & osmolality • describe the role of the kidney in regulation of body fluid volume & osmolality • Understand the role of ADH in the reabsorption of water and urea • Identify the site and describe the influence of aldosterone on reabsorption of Na + in the late distal tubules. Renal regulation of ECF Volume & Osmolality Is a reflex mechanism in which variables reflecting total body sodium and ECV are monitored by appropriate sensors Regulation of ECF volume = Regulation of body Na + = Regulation BP Thus, regulation of Na + is also dependent upon baroreceptors. Renal Regulation of ECV • Sensor – Carotid sinus – Volume receptors (large vein, atria, intrarenal artery) • Effectors – Rennin/angiotensin, aldosterone – Renal sympathetic nerve – ANF – ADH • Affecting – Urinary Na excretion Renal regulation of blood osmolality – Sensors • Hypothalamic osmoreceptors – Effectors • ADH • thirst – Affecting • Urine osmolaity • Water intake Osmoreceptor ADH Feedback System 1. INCREASED OSMOLALITY 2. DECREASED ARTERIAL PRESSURE 3. DECREASED BLOOD VOLUME FACTORS AFFECTING ADH Increase ADH Decrease ADH ↑Osmolarity ↓Osmolarity -
Amplification of Transducer Gain by Angiotensin II- Mediated Enhancement of Cortical Actin Density in Osmosensory Neurons
9536 • The Journal of Neuroscience, September 17, 2008 • 28(38):9536–9544 Cellular/Molecular Amplification of Transducer Gain by Angiotensin II- Mediated Enhancement of Cortical Actin Density in Osmosensory Neurons Zizhen Zhang and Charles W. Bourque Centre for Research in Neuroscience, McGill University and Montreal General Hospital, Montreal, Quebec, Canada H3G 1A4 Osmosensory neurons transduce osmotic signals into a neural spike code that commands behavioral and endocrine responses that mediate body fluid homeostasis. Although changes in osmoregulatory reflex gain are known to occur under physiological and patholog- ical conditions, the basis for this modulation is unknown. Here, we show that angiotensin II amplifies osmosensory transduction by enhancing the proportional relationship between osmolality, receptor potential, and action potential firing in rat supraoptic nucleus neurons. This effect is mediated by a phospholipase C- and protein kinase C-dependent increase in cellular mechanosensitivity that is associated with a rapid increase in cortical actin filament density. Preventing this increase with cytochalasin D eliminated the enhance- ment of mechanosensitivity, whereas enhancing actin filament density with jasplakinolide potentiated mechanosensitivity and occluded theeffectsofangiotensinII.Theseresultsindicatethatareceptor-mediatedincreaseincorticalactindensitycanenhanceosmosensitivity in acutely isolated supraoptic neurons. Key words: actin; angiotensin II; cytoskeleton; osmotic pressure; osmosensitivity; supraoptic nucleus; vasopressin Introduction et al., 1983; Wilkin et al., 1989), where they excite the magnocel- Osmosensory neurons play a fundamental role in the control of lular neurosecretory cells (MNCs) that release vasopressin from extracellular fluid (ECF) osmolality. In mammals, these neurons the neurohypophysis (Sgro et al., 1984). In vivo, subfornical or- detect small changes in ECF osmolality and transduce them into gan neurons are activated by hypovolemia (Ishibashi et al., 1985; proportional changes in action potential firing rate. -
Application for Amend to License 06-00092-05,Designating FS
.y - _ - - _ - - .- _ - - - - - - . - - - - - - - - - - - - - - - - - -, * y k * * , Mrdicti Cantsr West Spring Street ' . West Haven, CT 06516 . ' q veteransAdm,inistration, er March 5, 1985 \ 6 / k / 5j 5 Materials Licens g Branch \,,8 i ! Division of F' and Materials Safety / U.S. Nuclea egulatory Commission 'g%.,/ Washingt , D.C. 20555 Gentlemen: NBC Lic. #06-00092-05 Subject: New Chairman, Medical Isotopes and Radiatien Safety Committee Ronald D. Neumann, M.D. is leaving this VA Medical Center and is resigning the position of Chairman of the Medical Isotopes and Radiation Safety Committee. At the meeting of the Medical Isotopea and Radiation Safety Committee held on February 7,1985, Fred S. Wright, M.D. was approved as the next Chairman. Dr. Wright's curricula vitae is enclosed. Sincerely, HECE E.-U MAR 1 BSS /? ,,o * utitAR 14LDiCild 5thW bka,)h'| ta.b UW ALBERT M. BLECICH Medical Center Director Encl. -. cc: Dr. James J. Smith / VAC0 /e D , nuy.auw . '&&p- _ , D2:e. * '' - ANY J AE3 J/ CH JH. W. D. (115) ' , Direct r, h c'r a r IN31cino CeI71C8 ter.. .. , , VA Ce tral C.'" t ca "/' - flacht 1. D.C. 20420 ! n re . ........ eI z q,s m a,gt - s - aN/aa/h,. i ;;2 . men .- __ - "0FFICIAl. RECORD COPY" in 8% nur, 689/115 U'1d n- np m .ly ()3651 851ooeo204 eso91s ' p,np?'Q(pli' T O p REG 1 LIC30 w ta=* D ' * d 'd 06-00092-o5 PDR APR 0 51985 , . , * * , CURRICULUM VITAE FRED SMITH WRICHT, M.D. Born: St. Louis, Missouri, June 10, 1937 Education: Whitefish Bay H.S.