Different Munc18 Proteins Mediate Baseline and Stimulated Airway Mucin Secretion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Peroxisomal Proliferator–Activated Receptor- Upregulates
Peroxisomal Proliferator–Activated Receptor-␥ Upregulates Glucokinase Gene Expression in -Cells Ha-il Kim,1 Ji-Young Cha,1 So-Youn Kim,1 Jae-woo Kim,1 Kyung Jin Roh,2 Je-Kyung Seong,2 Nam Taek Lee,3 Kang-Yell Choi,1 Kyung-Sup Kim,1 and Yong-ho Ahn1 Thiazolidinediones, synthetic ligands of peroxisomal because of severe hyperglycemia (2,3). Adenovirus-medi- proliferator–activated receptor-␥ (PPAR-␥), improve ated expression of GLUT2 and GK in IL cells results in peripheral insulin sensitivity and glucose-stimulated gaining of glucose sensitivity (4). Thus, GLUT2 and GK are insulin secretion in pancreatic -cells. To explore the important in glucose sensing of -cells. However, GLUT2, role of PPAR-␥ in glucose sensing of -cells, we have being a low-affinity, high-capacity glucose transporter, is   dissected the -cell–specific glucokinase ( GK) pro- believed to play a more permissive role in glucose sensing, moter, which constitutes glucose-sensing apparatus in pancreatic -cells, and identified a peroxisomal prolif- allowing rapid equilibration of glucose across the plasma erator response element (PPRE) in the promoter. The membrane. GK traps glucose in -cells by phosphorylation GK-PPRE is located in the region between ؉47 and (5) and is the flux-controlling enzyme for glycolysis in ؉68 bp. PPAR-␥/retinoid X receptor-␣ heterodimer -cells (4). Thus, it serves as the gatekeeper for metabolic binds to the element and activates the GK promoter. signaling, suggesting that GK rather than GLUT2 is directly The GK promoter lacking or having mutations in PPRE ␥ ␥ responsible for the insulin secretion in response to in- cannot be activated by PPAR- . -

(12) Patent Application Publication (10) Pub. No.: US 2014/0155567 A1 Burk Et Al
US 2014O155567A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2014/0155567 A1 Burk et al. (43) Pub. Date: Jun. 5, 2014 (54) MICROORGANISMS AND METHODS FOR (60) Provisional application No. 61/331,812, filed on May THE BIOSYNTHESIS OF BUTADENE 5, 2010. (71) Applicant: Genomatica, Inc., San Diego, CA (US) Publication Classification (72) Inventors: Mark J. Burk, San Diego, CA (US); (51) Int. Cl. Anthony P. Burgard, Bellefonte, PA CI2P 5/02 (2006.01) (US); Jun Sun, San Diego, CA (US); CSF 36/06 (2006.01) Robin E. Osterhout, San Diego, CA CD7C II/6 (2006.01) (US); Priti Pharkya, San Diego, CA (52) U.S. Cl. (US) CPC ................. CI2P5/026 (2013.01); C07C II/I6 (2013.01); C08F 136/06 (2013.01) (73) Assignee: Genomatica, Inc., San Diego, CA (US) USPC ... 526/335; 435/252.3:435/167; 435/254.2: (21) Appl. No.: 14/059,131 435/254.11: 435/252.33: 435/254.21:585/16 (22) Filed: Oct. 21, 2013 (57) ABSTRACT O O The invention provides non-naturally occurring microbial Related U.S. Application Data organisms having a butadiene pathway. The invention addi (63) Continuation of application No. 13/101,046, filed on tionally provides methods of using Such organisms to produce May 4, 2011, now Pat. No. 8,580,543. butadiene. Patent Application Publication Jun. 5, 2014 Sheet 1 of 4 US 2014/O155567 A1 ?ueudos!SMS |?un61– Patent Application Publication Jun. 5, 2014 Sheet 2 of 4 US 2014/O155567 A1 VOJ OO O Z?un61– Patent Application Publication US 2014/O155567 A1 {}}} Hººso Patent Application Publication Jun. -

Signal Transduction Convergence: Phorbol Esters and Insulin Inhibit Phosphoenolpyruvate Carboxykinase Gene Transcription Through
Proc. Natl. Acad. Sci. USA Vol. 88, pp. 6580-6584, August 1991 Biochemistry Signal transduction convergence: Phorbol esters and insulin inhibit phosphoenolpyruvate carboxykinase gene transcription through the same 10-base-pair sequence RICHARD M. O'BRIEN, MARIA T. BONOVICH, CLAUDE D. FOREST, AND DARYL K. GRANNER* Department of Molecular Physiology and Biophysics, Vanderbilt University Medical School, Nashville, TN 37232-0615 Communicated by Charles R. Park, April 29, 1991 ABSTRACT Pbosphoenolpyruvate carboxykinase describe such an element here and in so doing report an (PEPCK) governs the rate-limiting step in gluconeogenesis. example of signal transduction convergence: the inhibitory Glucocorticoids and cAMP increase PEPCK gene transcription effects of phorbol esters and insulin on the PEPCK gene, and gluconeogenesis, whereas insulin and phorbol esters have which start with the generation of unique signals, are medi- the opposite effect. Insulin and phorbol esters are dominant, ated through a common 10-base-pair (bp) sequence. since they prevent cAMP and glucocorticoid-stinulated tran- scription. Basal promoter elements and hormone response elements for cAMP, glucocorticoids, and insulin have been MATERIALS AND METHODS defined in previous studies. By using stable transfectants containing a variety of different PEPCK-chloramphenicol Plasmid Construction. The construction of a series of acetyltransferase fusion gene constructs, a phorbol ester re- reporter constructs containing 5' deletion mutations of the sponse sequence, located between positions -437 and -402 PEPCK promoter ligated to the chloramphenicol acetyltrans- relative to the transcription start site, was identified. This ferase (CAT) gene has been described (23). Plasmid TKC-VI region coincides with the insulin response sequence that has (provided by T. -
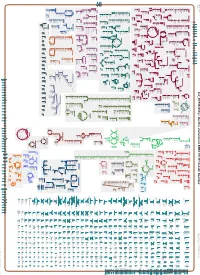
Generate Metabolic Map Poster
Authors: Pallavi Subhraveti Ron Caspi Peter Midford Peter D Karp An online version of this diagram is available at BioCyc.org. Biosynthetic pathways are positioned in the left of the cytoplasm, degradative pathways on the right, and reactions not assigned to any pathway are in the far right of the cytoplasm. Transporters and membrane proteins are shown on the membrane. Ingrid Keseler Periplasmic (where appropriate) and extracellular reactions and proteins may also be shown. Pathways are colored according to their cellular function. Gcf_001591825Cyc: Bacillus vietnamensis NBRC 101237 Cellular Overview Connections between pathways are omitted for legibility. Anamika Kothari sn-glycerol phosphate phosphate pro phosphate phosphate phosphate thiamine molybdate D-xylose D-ribose glutathione 3-phosphate D-mannitol L-cystine L-djenkolate lanthionine α,β-trehalose phosphate phosphate [+ 3 more] α,α-trehalose predicted predicted ABC ABC FliY ThiT XylF RbsB RS10935 UgpC TreP PutP RS10200 PstB PstB RS10385 RS03335 RS20030 RS19075 transporter transporter of molybdate of phosphate α,β-trehalose 6-phosphate L-cystine D-xylose D-ribose sn-glycerol D-mannitol phosphate phosphate thiamine glutathione α α phosphate phosphate phosphate phosphate L-djenkolate 3-phosphate , -trehalose 6-phosphate pro 1-phosphate lanthionine molybdate phosphate [+ 3 more] Metabolic Regulator Amino Acid Degradation Amine and Polyamine Biosynthesis Macromolecule Modification tRNA-uridine 2-thiolation Degradation ATP biosynthesis a mature peptidoglycan a nascent β an N-terminal- -

Herpes Simplex Virus Thymidine Kinase Gene Therapy in Experimental Rat BT4C Glioma Model
© 2000 Nature America, Inc. 0929-1903/00/$15.00/ϩ0 www.nature.com/cgt Herpes simplex virus thymidine kinase gene therapy in experimental rat BT4C glioma model: Effect of the percentage of thymidine kinase-positive glioma cells on treatment effect, survival time, and tissue reactions Anu-Maaria Sandmair,1,2 Marita Turunen,1,3 Kristiina Tyynela¨,1,3 Sami Loimas,1 Pauli Vainio,4 Ritva Vanninen,4 Matti Vapalahti,2,5 Rolf Bjerkvig,6 Juhani Ja¨nne,1,5 and Seppo Yla¨-Herttuala1,5,7 1A.I. Virtanen Institute, University of Kuopio, Kuopio, Finland; Departments of 2Neurosurgery, 3Oncology, and 4Clinical Radiology, and 5Gene Therapy Unit, University Hospital of Kuopio, Kuopio, Finland; 6Department of Anatomy and Cell Biology, University of Bergen, Bergen, Norway; and 7Department of Medicine, University Hospital of Kuopio, Kuopio, Finland. Herpes simplex virus thymidine kinase (HSV-tk) gene transfer and ganciclovir (GCV) administration have been suggested for the treatment of malignant gliomas. To understand tissue responses and possible ways to improve the treatment effect, we studied tumor growth, tissue reactions, and survival time after HSV-tk/GCV treatment in a syngeneic BT4C rat glioma model by mixing various ratios of stably transfected HSV-tk-expressing BT4C-tk glioma cells with wild-type BT4C glioma cells (percentage of BT4C-tk cells: 0%, 1%, 10%, 30%, 50%, and 100%), followed by injection into BDIX rat brains (n ϭ 79). With the exception of some animals with end-stage tumors, very little astroglia or microglia reactivity was detected in the wild-type tumors as analyzed by immunocytochemistry using glial fibrillary acid protein (GFAP)-, vimentin-, human histocompatibility leukocyte antigen-DR-, OX-42-, and CD68-specific monoclonal antibodies. -

The Effect of Glucosone on the Proliferation and Energy Metabolism of in Vitro Grown Ehrlich Ascites Tumor Cells Karl A
The Effect of Glucosone on the Proliferation and Energy Metabolism of in vitro Grown Ehrlich Ascites Tumor Cells Karl A. Reiffen, Monika Löffler, and Friedh. Schneider Physiologisch-Chemisches Institut der Universität Marburg, Lahnberge, D-3550 Marburg Dedicated to Prof. F. Zilliken on the Occasion of His 60th Birthday Z. Naturforsch. 36 c, 255-261 (1981); received November 4/November 17, 1980 Ehrlich Ascites Tumor Cells, Proliferation, Energy Metabolism, Glucosone 1) Proliferation and energy metabolism of in vitro grown Ehrlich ascites tumor (EAT) cells in the presence of glucosone, (D-arabino-3.4.5.6-tetrahydroxy-2-oxo-hexanal) a competitive inhibitor of hexokinase, were studied. 2) Proliferation of the cells was completely inhibited by 2 m M glucosone without severely affecting viability (dye exclusion test). No phase specific arrest of cell growth was observed. 3) Incorporation of [14C]thymidine into an acid insoluble fraction of the cells decreases to 5% of the controls within 8 -1 0 h . Incorporation of [14C]leucine begins to slow down immediately after treatment with glucosone. 4) The inhibitor (2 m M ) reduces the lactate production of the cells by 60%, respiration by about 20%; the ATP/ADP ratio slows down from 4.75 to 3.5. 5) The total inhibition of cell proliferation by 2 m M glucosone cannot be explained exclusively by inhibition of hexokinase activity and impairment of energy metabolism. Because of a lack of specificity, glucosone is not a suitable inhibitor for studies on the relationship between hexo kinase activity and cell proliferation of tumor cells. Of all the glycolytic enzymes it may be that Rather additional effects of glucosone on cellular hexokinase is the most important in amplifying the metabolism must be taken into consideration. -

Supplementary Information
Supplementary information (a) (b) Figure S1. Resistant (a) and sensitive (b) gene scores plotted against subsystems involved in cell regulation. The small circles represent the individual hits and the large circles represent the mean of each subsystem. Each individual score signifies the mean of 12 trials – three biological and four technical. The p-value was calculated as a two-tailed t-test and significance was determined using the Benjamini-Hochberg procedure; false discovery rate was selected to be 0.1. Plots constructed using Pathway Tools, Omics Dashboard. Figure S2. Connectivity map displaying the predicted functional associations between the silver-resistant gene hits; disconnected gene hits not shown. The thicknesses of the lines indicate the degree of confidence prediction for the given interaction, based on fusion, co-occurrence, experimental and co-expression data. Figure produced using STRING (version 10.5) and a medium confidence score (approximate probability) of 0.4. Figure S3. Connectivity map displaying the predicted functional associations between the silver-sensitive gene hits; disconnected gene hits not shown. The thicknesses of the lines indicate the degree of confidence prediction for the given interaction, based on fusion, co-occurrence, experimental and co-expression data. Figure produced using STRING (version 10.5) and a medium confidence score (approximate probability) of 0.4. Figure S4. Metabolic overview of the pathways in Escherichia coli. The pathways involved in silver-resistance are coloured according to respective normalized score. Each individual score represents the mean of 12 trials – three biological and four technical. Amino acid – upward pointing triangle, carbohydrate – square, proteins – diamond, purines – vertical ellipse, cofactor – downward pointing triangle, tRNA – tee, and other – circle. -

The Metabolic Building Blocks of a Minimal Cell Supplementary
The metabolic building blocks of a minimal cell Mariana Reyes-Prieto, Rosario Gil, Mercè Llabrés, Pere Palmer and Andrés Moya Supplementary material. Table S1. List of enzymes and reactions modified from Gabaldon et. al. (2007). n.i.: non identified. E.C. Name Reaction Gil et. al. 2004 Glass et. al. 2006 number 2.7.1.69 phosphotransferase system glc + pep → g6p + pyr PTS MG041, 069, 429 5.3.1.9 glucose-6-phosphate isomerase g6p ↔ f6p PGI MG111 2.7.1.11 6-phosphofructokinase f6p + atp → fbp + adp PFK MG215 4.1.2.13 fructose-1,6-bisphosphate aldolase fbp ↔ gdp + dhp FBA MG023 5.3.1.1 triose-phosphate isomerase gdp ↔ dhp TPI MG431 glyceraldehyde-3-phosphate gdp + nad + p ↔ bpg + 1.2.1.12 GAP MG301 dehydrogenase nadh 2.7.2.3 phosphoglycerate kinase bpg + adp ↔ 3pg + atp PGK MG300 5.4.2.1 phosphoglycerate mutase 3pg ↔ 2pg GPM MG430 4.2.1.11 enolase 2pg ↔ pep ENO MG407 2.7.1.40 pyruvate kinase pep + adp → pyr + atp PYK MG216 1.1.1.27 lactate dehydrogenase pyr + nadh ↔ lac + nad LDH MG460 1.1.1.94 sn-glycerol-3-phosphate dehydrogenase dhp + nadh → g3p + nad GPS n.i. 2.3.1.15 sn-glycerol-3-phosphate acyltransferase g3p + pal → mag PLSb n.i. 2.3.1.51 1-acyl-sn-glycerol-3-phosphate mag + pal → dag PLSc MG212 acyltransferase 2.7.7.41 phosphatidate cytidyltransferase dag + ctp → cdp-dag + pp CDS MG437 cdp-dag + ser → pser + 2.7.8.8 phosphatidylserine synthase PSS n.i. cmp 4.1.1.65 phosphatidylserine decarboxylase pser → peta PSD n.i. -

Supplementary Informations SI2. Supplementary Table 1
Supplementary Informations SI2. Supplementary Table 1. M9, soil, and rhizosphere media composition. LB in Compound Name Exchange Reaction LB in soil LBin M9 rhizosphere H2O EX_cpd00001_e0 -15 -15 -10 O2 EX_cpd00007_e0 -15 -15 -10 Phosphate EX_cpd00009_e0 -15 -15 -10 CO2 EX_cpd00011_e0 -15 -15 0 Ammonia EX_cpd00013_e0 -7.5 -7.5 -10 L-glutamate EX_cpd00023_e0 0 -0.0283302 0 D-glucose EX_cpd00027_e0 -0.61972444 -0.04098397 0 Mn2 EX_cpd00030_e0 -15 -15 -10 Glycine EX_cpd00033_e0 -0.0068175 -0.00693094 0 Zn2 EX_cpd00034_e0 -15 -15 -10 L-alanine EX_cpd00035_e0 -0.02780553 -0.00823049 0 Succinate EX_cpd00036_e0 -0.0056245 -0.12240603 0 L-lysine EX_cpd00039_e0 0 -10 0 L-aspartate EX_cpd00041_e0 0 -0.03205557 0 Sulfate EX_cpd00048_e0 -15 -15 -10 L-arginine EX_cpd00051_e0 -0.0068175 -0.00948672 0 L-serine EX_cpd00054_e0 0 -0.01004986 0 Cu2+ EX_cpd00058_e0 -15 -15 -10 Ca2+ EX_cpd00063_e0 -15 -100 -10 L-ornithine EX_cpd00064_e0 -0.0068175 -0.00831712 0 H+ EX_cpd00067_e0 -15 -15 -10 L-tyrosine EX_cpd00069_e0 -0.0068175 -0.00233919 0 Sucrose EX_cpd00076_e0 0 -0.02049199 0 L-cysteine EX_cpd00084_e0 -0.0068175 0 0 Cl- EX_cpd00099_e0 -15 -15 -10 Glycerol EX_cpd00100_e0 0 0 -10 Biotin EX_cpd00104_e0 -15 -15 0 D-ribose EX_cpd00105_e0 -0.01862144 0 0 L-leucine EX_cpd00107_e0 -0.03596182 -0.00303228 0 D-galactose EX_cpd00108_e0 -0.25290619 -0.18317325 0 L-histidine EX_cpd00119_e0 -0.0068175 -0.00506825 0 L-proline EX_cpd00129_e0 -0.01102953 0 0 L-malate EX_cpd00130_e0 -0.03649016 -0.79413596 0 D-mannose EX_cpd00138_e0 -0.2540567 -0.05436649 0 Co2 EX_cpd00149_e0 -

Increased Cytotoxicity of Herpes Simplex Virus Thymidine Kinase Expression in Human Induced Pluripotent Stem Cells
International Journal of Molecular Sciences Article Increased Cytotoxicity of Herpes Simplex Virus Thymidine Kinase Expression in Human Induced Pluripotent Stem Cells Chizuru Iwasawa 1, Ryota Tamura 2, Yuki Sugiura 3, Sadafumi Suzuki 4, Naoko Kuzumaki 1, Minoru Narita 1, Makoto Suematsu 3, Masaya Nakamura 5, Kazunari Yoshida 2, Masahiro Toda 2, Hideyuki Okano 4,* and Hiroyuki Miyoshi 4,* 1 Department of Pharmacology, Hoshi University School of Pharmacy and Pharmaceutical Sciences, 2-4-41, Ebara, Shinagawa-ku, Tokyo 142-8501, Japan; [email protected] (C.I.); [email protected] (N.K.); [email protected] (M.N.) 2 Department of Neurosurgery, Keio University School of Medicine, 35 Shinanomachi, Shinjuku-ku, Tokyo 160-8582, Japan; [email protected] (R.T.); [email protected] (K.Y.); [email protected] (M.T.) 3 Department of Biochemistry, Keio University School of Medicine, 35 Shinanomachi, Shinjuku-ku, Tokyo 160-8582, Japan; [email protected] (Y.S.); [email protected] (M.S.) 4 Department of Physiology, Keio University School of Medicine, 35 Shinanomachi, Shinjuku-ku, Tokyo 160-8582, Japan; [email protected] 5 Department of Orthopedic Surgery, Keio University School of Medicine, 35 Shinanomachi, Shinjuku-ku, Tokyo 160-8582, Japan; [email protected] * Correspondence: [email protected] (H.O.); [email protected] (H.M.); Tel.: +81-3-5363-3747 (H.O. & H.M.); Fax: +81-3-3357-5445 (H.O. & H.M.) Received: 19 November 2018; Accepted: 11 February 2019; Published: 14 February 2019 Abstract: Human induced pluripotent stem cells (iPSCs) hold enormous promise for regenerative medicine. The major safety concern is the tumorigenicity of transplanted cells derived from iPSCs. -

A Review of Isozymes in Cancer1
Cancer Research VOLUME31 NOVEMBER 1971 NUMBER11 [CANCER RESEARCH 31, 1523-1542, November 1971] A Review of Isozymes in Cancer1 Wayne E. Criss Department of Obstetrics and Gynecology, University of Florida College of Medicine, Gainesville, Florida 32601 TABLE OF CONTENTS postulated role for that particular isozymic system in cellular metabolism. Summary 1523 Introduction 1523 Normal enzyme differentiation 1523 INTRODUCTION Tumor enzyme differentiation 1524 Isozymes 1524 Normal Enzyme Differentiation DNA polymerase 1524 Enzyme differentiation is the process whereby, during the Hexokinase 1525 Fructose 1,6-diphosphatase 1525 development of an organ in an animal, the organ acquires the quantitative and qualitative adult enzyme patterns (122). Key Aldolase 1526 pathway enzymes in several metabolic processes have been Pyruvate kinase 1527 found to undergo enzymatic differentiation. The enzymes Láclatedehydrogenase 1527 Isocitrate dehydrogenase 1527 involved in nitrogen metabolism, and also in urea cycle Malate dehydrogenase 1528 metabolism (180), are tyrosine aminotransferase (123, 151, Glycerol phosphate dehydrogenase 1529 330, 410), tryptophan pyrrolase (261), serine dehydratase Glutaminase 1529 (123, 410), histidine ammonia lyase (11), and aspartate Aspartate aminotransferase 1530 aminotransferase (337, 388). The enzymes involved in nucleic Adenylate kinase 1531 acid metabolism are DNA polymerase (156, 277) and RNase (52). In glycolysis the enzymes are hexokinase-glucokinase Carbamyl phosphate synthetase 1531 Lactose synthetase 1533 (98, 389), galactokinase 30, aldolase (267, 315), pyruvate Discussion 1533 kinase (73, 386), and lactate dehydrogenase (67, 69). In References 1533 mitochondrial oxidation they are NADH oxidase, succinic oxidase, a-glycero-P oxidase, ATPase, cytochrome oxidase, and flavin content (84, 296). In glycogen metabolism the SUMMARY enzymes involved are UDPG pyrophosphorylase and UDPG glucosyltransferase (19). -

Monitoring of Successive Phosphorylations of Thymidine
Monitoring of successive phosphorylations of thymidine using free and immobilized human nucleoside/nucleotide kinases by Flow Injection Analysis with High-Resolution Mass Spectrometry Justine Ferey, David da Silva, Cyril Colas, Reine Nehmé, Pierre Lafite, Vincent Roy, Philippe Morin, Richard Daniellou, Luigi Agrofoglio, Benoît Maunit To cite this version: Justine Ferey, David da Silva, Cyril Colas, Reine Nehmé, Pierre Lafite, et al.. Monitoring of successive phosphorylations of thymidine using free and immobilized human nucleoside/nucleotide kinases by Flow Injection Analysis with High-Resolution Mass Spectrometry. Analytica Chimica Acta, Elsevier Masson, 2019, 1049, pp.115-122. 10.1016/j.aca.2018.10.032. hal-02090335 HAL Id: hal-02090335 https://hal.archives-ouvertes.fr/hal-02090335 Submitted on 29 Nov 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Monitoring of successive phosphorylations of thymidine using free and immobilized human nucleoside/nucleotide kinases by Flow Injection Analysis with High-Resolution Mass Spectrometry Justine Ferey1, David Da Silva*1, Cyril Colas1,2, Reine Nehmé*1, Pierre Lafite1, Vincent Roy1, Philippe Morin1, Richard Daniellou1, Luigi Agrofoglio1, Benoît Maunit1. 1 Univ. Orléans, CNRS, ICOA, UMR 7311, F-45067 Orléans, France.