Shortness of Breath
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Caring for Children with Special Needs ALLERGIES and ASTHMA
caring for children with special needs ALLERGIES AND ASTHMA We don’t usually think of children with allergies or asthma as children with “special needs,” but they certainly are. In fact, children with these conditions are probably the most frequently encountered “special needs” children. Child care providers can do a great deal to help individual children manage their specific allergy or asthma needs and feel more comfortable in a child care setting. Allergies wastes. Every house has them, no matter how clean. Other inhaled Children with allergies face the allergens include mold, pollen (hay same social difficulties as do adults, fever), animal dander (especially but they have less maturity and from cats), chemicals, and per emotional resources to deal with fumes. them. Children find that they cannot eat what their friends eat or The most common allergy symp cannot play outside during some toms are seasons. Until a child is mature � a clear, runny nose and enough to understand why she sneezing, cannot do something, you must be � itchy or stuffed-up nose or careful to help the child through the itchy, runny eyes, and difficulties. Start teaching a child early on about what he is allergic to; � asthma (remember that not all you will not always be able to people with asthma have monitor everything. allergies and not all allergies Some foods can cause a life cause or develop into asthma). threatening reaction. The mouth, throat, and bronchial tubes swell enough to interfere with breathing. Strategies for inclusion The person may wheeze or faint. Some parents have found that by Often there are generalized hives volunteering to bring food to and/or a swollen face. -

Symptoms Related to Asthma and Chronic Bronchitis in Three Areas of Sweden
Eur Respir J, 1994, 7, 2146–2153 Copyright ERS Journals Ltd 1994 DOI: 10.1183/09031936.94.07122146 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 Symptoms related to asthma and chronic bronchitis in three areas of Sweden E. Björnsson*, P. Plaschke**, E. Norrman+, C. Janson*, B. Lundbäck+, A. Rosenhall+, N. Lindholm**, L. Rosenhall+, E. Berglund++, G. Boman* Symptoms related to asthma and chronic bronchitis in three areas of Sweden. E. Björnsson, *Dept of Lung Medicine and Asthma P. Plaschke, E. Norrman, C. Janson, B. Lundbäck, A. Rosenhall, N. Lindholm, L. Research Center, Akademiska sjukhu- Rosenhall, E. Berglund, G. Boman. ERS Journals Ltd 1994. set, Uppsala University, Uppsala, Sweden. ABSTRACT: Does the prevalence of respiratory symptoms differ between regions? **Asthma and Allergy Research Center, Sahlgren's Hospital, University of Göteborg, As a part of the European Community Respiratory Health Survey, we present data Göteborg, Sweden. +Dept of Pulmonary from an international questionnaire on asthma symptoms occurring during a 12 Medicine and Allergology, Univer- month period, smoking and symptoms of chronic bronchitis. The questionnaire was sity Hospital of Northern Sweden, Umeå, mailed to 10,800 persons aged 20–44 yrs living in three regions of Sweden (Västerbotten, Sweden. ++Dept of Pulmonary Medicine, Uppsala and Göteborg) with different environmental characteristics. The total Sahlgrenska University Hospital, Göteborg, response rate was 86%. Sweden. Wheezing was reported by 20.5%, and the combination of wheezing without a Correspondence: E. Björnsson, Dept of cold and wheezing with breathlessness by 7.4%. The use of asthma medication was Lung Medicine, Akademiska sjukhuset, S- reported by 5.3%. -
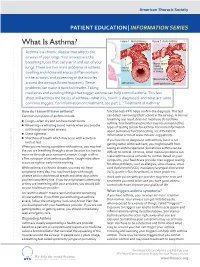
What Is Asthma? Figure 1
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What Is Asthma? Figure 1. Normal Airway Figure 2. Acute Asthma Asthma is a chronic disease that affects the airways of your lungs. Your airways are the breathing tubes that carry air in and out of your Muscle spasm causing lungs. There are two main problems in asthma: relaxed narrowing muscles swelling and increased mucus (inflammation) of airways in the airways, and squeezing of the muscles Mucus build up around the airways (bronchospasm). These open airways Swelling/inammation problems can make it hard to breathe. Taking medicines and avoiding things that trigger asthma can help control asthma. This fact sheet will address the basics of asthma—what it is, how it is diagnosed, and what are some common triggers. For information on treatment, see part 2, “Treatment of Asthma”. How do I know if I have asthma? function test–PFT) helps confirm the diagnosis. This test Common symptoms of asthma include: can detect narrowing (obstruction) in the airways. A normal breathing test result does not mean you do not have ■ Cough—often dry and can have harsh bursts asthma. Your healthcare provider may recommend other ■ Wheezing—a whistling sound mainly when you breathe types of testing to look for asthma. For more information out through narrowed airways about pulmonary function testing, see ATS Patient ■ Chest tightness Information series at www.thoracic.org/patients. ■ Shortness of breath which may occur with activity or If you have been diagnosed with asthma, but it is not even at rest getting better with treatment, you might benefit from When you are having a problem with asthma, you may feel CLIP AND COPY AND CLIP seeing an asthma specialist. -

Acute Chest Syndrome in Sickle Cell Disease Care Guideline
Acute Chest Syndrome in Sickle Cell Disease Care Guideline Inclusion Criteria: · Children with sickle cell disease Recommendations/ · New pulmonary infiltrate on CXR, involving at least one Considerations complete lung segment, excluding atelectasis Predictors: · Pain crisis involving chest, shoulders Assessment and back · Admit to 5S or PICU · Post anesthesia complication · NPO · Respiratory Infections · History and physical with focus on pulmonary exam · On narcotics · Vitals, accurate height and weight · Asthma exacerbation · Strict I/O; Daily Weight · O2 saturation · Baseline Hgb level may run low < · Diagnostics: 9gm/dl CBC with retic, CMP with LDH, STAT type and screen, Hgb electrophoresis · If suspected pulmonary embolism, · Consider VBG for significant respiratory distress obtain CT angiogram of chest · CXR 2 view · Blood culture if fever >38, elevated WBC · May need more than 1 exchange · VRP if URI symptoms transfusion if clinical findings not improving Interventions · After recovery from acute crisis, pt · Stat Hematology consult (if not admitted to Hematology service) should be started on hydroxyurea if · Pulmonary consult not already taking; optimize dose · Notify apheresis team as soon as possible during working hours if anticipated procedure · History of more than 1 acute chest · Consult PICU for possible apheresis catheter placement crisis, consider chronic transfusion · Oxygen to keep O2 sat >=94% protocols to keep HgbS < 25% · Maintenance IV fluids · Antibiotics: ceftriaxone and azithromycin · If recurrent crises, consider -

Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation
Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation Dr Rohit Bazaz National Aspergillosis Centre, UK Manchester University NHS Foundation Trust/University of Manchester ~ ABPA -a41'1 Severe asthma wl'th funga I Siens itisat i on Subacute IA Chronic pulmonary aspergillosjs Simp 1Ie a:spe rgmoma As r§i · bronchitis I ram une dysfu net Ion Lun· damage Immu11e hypce ractivitv Figure 1 In t@rarctfo n of Aspergillus Vliith host. ABP A, aHerg tc broncho pu~ mo na my as µe rgi ~fos lis; IA, i nvas we as ?@rgiH os 5. MANCHl·.'>I ER J:-\2 I Kosmidis, Denning . Thorax 2015;70:270–277. doi:10.1136/thoraxjnl-2014-206291 Allergic Fungal Airway Disease Phenotypes I[ Asthma AAFS SAFS ABPA-S AAFS-asthma associated with fu ngaIsensitization SAFS-severe asthma with funga l sensitization ABPA-S-seropositive a llergic bronchopulmonary aspergi ll osis AB PA-CB-all ergic bronchopulmonary aspergi ll osis with central bronchiectasis Agarwal R, CurrAlfergy Asthma Rep 2011;11:403 Woolnough K et a l, Curr Opin Pulm Med 2015;21:39 9 Stanford Lucile Packard ~ Children's. Health Children's. Hospital CJ Scanford l MEDICINE Stanford MANCHl·.'>I ER J:-\2 I Aspergi 11 us Sensitisation • Skin testing/specific lgE • Surface hydroph,obins - RodA • 30% of patients with asthma • 13% p.atients with COPD • 65% patients with CF MANCHl·.'>I ER J:-\2 I Alternar1a• ABPA •· .ABPA is an exagg·erated response ofthe imm1une system1 to AspergUlus • Com1pUcatio n of asthm1a and cystic f ibrosis (rarell·y TH2 driven COPD o r no identif ied p1 rior resp1 iratory d isease) • ABPA as a comp1 Ucation of asth ma affects around 2.5% of adullts. -

Diseases of the Respiratory System (J00-J99) ICD-10-CM
Diseases of the Respiratory System (J00-J99) ICD-10-CM Coverage provided by Amerigroup Inc. This publication contains proprietary information. This material is for informational purposes only. Reference the Centers for Medicare and Medicaid Services (CMS) for more information on Risk Adjustment and the CMS-HCC Model. Redistribution or other use is strictly forbidden This publication is for informational purposes only and is not guaranteed to be without defect. Please reference the current version(s) of the ICD-10-CM codebook, CMS-HCC Risk Adjustment Model, and AHA Coding Clinic for complete code sets and official coding guidance. AGPCARE-0080-19 63321MUPENABS 10/05/16 Diseases of the respiratory system are located in chapter Intermittent asthma which is defined as less 10 of the ICD-10-CM code book; this chapter includes than or equal to two occurrences per week. conditions such as asthma, pneumonia, and chronic Persistent asthma which includes three levels obstructive pulmonary disease (COPD). of severity: Mild: more than two times per week Reporting respiratory conditions Moderate: daily and may restrict Codes for reporting diseases of the respiratory physical activity system in ICD-10-CM feature relatively minor Severe: throughout the day with changes from ICD-9-CM. Most of the changes recurrent severe attacks limiting the involve understanding the medical terminology that ability to breathe the more specific codes include, as well as, the new The fourth character indicates severity, and the general coding structure and rules. fifth identifies whether status asthmaticus or At the beginning of chapter 10 for “Diseases of exacerbation is present. the Respiratory System (J00-J99),” an instructional note states, “When a respiratory condition is Asthma ICD-10-CM description described as occurring in more than one site and Category J45 Asthma is not specifically indexed, it should be classified Includes: to the lower anatomic site.” For example, Allergic: tracheobronchitis is classified to bronchitis with Asthma code J40. -

Acute Chest Syndrome
CLINICAL PATHWAY PEDIATRIC ACUTE CHEST SYNDROME (ACS) Patients with sickle cell disease presenting with 1) a new pulmonary infiltrate on chest radiography AND 2) evidence of lower airway disease (e.g. cough, shortness of breath, retractions, rales, etc.) TABLE OF CONTENTS Algorithm- N/A Target Population Background | Definitions Initial Evaluation-N/A Clinical Management Diagnostic Tests Fluids | Nutrition Respiratory Therapy Table 1. Pediatric Asthma Score Treatment Table 2. Antimicrobial Medication Table 3. Pain Medication Table 4. Respiratory Medication Discharge Criteria Related Children’s Hospital Colorado Documents References Clinical Improvement Team TARGET POPULATION Inclusion Criteria • Patients with sickle cell disease (SS, SC, Sβ0 thalassemia, Sβ+ thalassemia) • Patients of all ages • Patients treated year round Exclusion Criteria • Patients without infiltrate on chest radiograph (e.g. asthma exacerbation) • Patients with severe pulmonary hypertension • Patients post bone marrow transplant • Well children with pneumonia Page 1 of 10 CLINICAL PATHWAY BACKGROUND | DEFINITIONS Acute chest syndrome (ACS) is the second most common reason for hospitalization in children with sickle cell disease and a leading cause of mortality. ACS is defined as a new pulmonary infiltrate on chest radiograph in the presence of evidence of lower respiratory tract disease (e.g. some combination of cough, shortness of breath, retractions, rales, etc.). In the majority of cases of ACS, an etiology is unable to be identified. The most common identified etiology of ACS is infection but it may also result from pulmonary vaso-occlusion, pulmonary infarction or fat embolism. The primary infectious agents implicated in ACS include: Chlamydia pneumoniae, Mycoplasma pneumoniae, Streptococcus pneumoniae, and viruses. Risk factors for ACS include vaso-occlusive pain crisis, anesthesia, and surgery. -

Changes Seen on Computed Tomography of the Chest In
Alves UD et al.Original / CT of the Article chest in sickle cell disease Changes seen on computed tomography of the chest in mildly symptomatic adult patients with sickle cell disease* Alterações na tomografia computadorizada do tórax em pacientes adultos oligossintomáticos com doença falciforme Ursula David Alves1, Agnaldo José Lopes2, Maria Christina Paixão Maioli3, Andrea Ribeiro Soares3, Pedro Lopes de Melo4, Roberto Mogami5 Alves UD, Lopes AJ, Maioli MCP, Soares AR, Melo PL, Mogami R. Changes seen on computed tomography of the chest in mildly symptomatic adult patients with sickle cell disease. Radiol Bras. 2016 Jul/Ago;49(4):214–219. Abstract Objective: To describe and quantify the main changes seen on computed tomography of the chest in mildly symptomatic adult patients with sickle cell disease, as well as to evaluate the radiologist accuracy in determining the type of hemoglobinopathy. Materials and Methods: A prospective study involving 44 adult patients with sickle cell disease who underwent inspiration and expiration computed tomography of the chest. The frequency of tomography findings and the extent of involvement are reported. We also calculated radiologist accuracy in determining the type of hemoglobinopathy by analyzing the pulmonary alterations and morphology of the spleen. Results: The changes found on computed tomography scans, in descending order of frequency, were as follows: fibrotic opacities (81.8%); mosaic attenuation (56.8%); architectural distortion (31.8%); cardiomegaly (25.0%); lobar volume reduction (18.2%); and increased caliber of peripheral pulmonary arteries (9.1%). For most of the findings, the involvement was considered mild, five or fewer lung segments being affected. The accuracy in determining the type of hemoglobinopathy (HbSS group versus not HbSS group) was 72.7%. -

Predictors of Impending Acute Chest Syndrome in Patients with Sickle Cell
www.nature.com/scientificreports OPEN Predictors of impending acute chest syndrome in patients with sickle cell anaemia Salam Alkindi1,2*, Ikhlas Al-Busaidi1, Bushra Al-Salami1, Samir Raniga3, Anil Pathare 1 & Samir K. Ballas4 Acute chest syndrome (ACS) is a major complication of sickle cell anaemia (SCA) and a leading cause for hospital admissions and death. We aimed to study the spectrum of clinical and laboratory features of ACS and to assess the predisposing factors and predictors of severity. A retrospective case-control cohort was studied by retrieving patient information from electronic medical records after ethical approval. One hundred adolescents and adults with SCA and hospital admissions for ACS were identifed through the discharge summaries, along with 20 additional patients presenting with VOC, but without ACS (controls). Among the patients with ACS, fever (>38.5 °C), reduced oxygen saturation (<95) and asplenia signifcantly difered when compared to those of controls (p < 0.05, chi-squared test). The degree of severity was refected in the use of non-invasive ventilation (NIV), simple and exchange transfusions, and the presence of bilateral pleural efusions and multi-lobar atelectasis/consolidation, which were signifcantly higher in the cases with ACS than in the controls. Lower haemoglobin (Hb) and high WBC counts were also signifcantly diferent between the two groups (p < 0.05, Student’s t test). Using logistic regression, our study further demonstrated that asplenia, fever, and reduced O2 saturation, along with low Hb and leukocytosis, were important predictors for the development of ACS. Sickle cell anaemia (SCA) is an autosomal recessive disorder characterized by a point mutation in codon 6 of the beta globin chain, where glutamic acid is replaced by valine, resulting in the formation of HbS with varied clinical 1 manifestations . -

Sickle Cell Pathway V2.1: Suspected Acute Chest Syndrome Table of Contents
Sickle Cell Pathway v2.1: Suspected Acute Chest Syndrome Table of Contents Inclusion Criteria · New, non-atelactatic, pulmonary infiltrate in patient with a Stop and sickle cell hemoglobinopathy Review Exclusion Criteria · O2 need related to opiate use with no infiltrate on CXR Sickle Cell Care Suspected Acute Chest Syndrome Appendix Summary of Version Changes Approval & Citation Evidence Ratings For questions concerning this pathway, contact: Last Updated: October 2020 [email protected] Next Expected Review: October 2025 If you are a patient with questions contact your medical provider, Medical Disclaimer © 2020 Seattle Children’s Hospital, all rights reserved Sickle Cell Pathway v2.1: Suspected Acute Chest Syndrome Inclusion Criteria · New, non-atelactatic, pulmonary infiltrate in patient with a Stop and sickle cell hemoglobinopathy Review Exclusion Criteria · O2 need related to opiate use with no infiltrate on CXR Evaluations for Acute Chest · Physical Exam · CXR · O2 sats · Consider viral studies · Blood & Urine Cx · CBC, diff, retic and type and cross Admit if not already admitted Standard Conservative Therapy · Aggressive pain management · Incentive spirometry q 1 hrs while awake, 10 breaths every hour from 0800 to 2200 and with vital signs while awake from 2200 to 0800, as well as with every "as needed" IV bolus of pain medication, and prior to chest x-rays · Oxygen to maintain O2 saturation >93% · Ceftriaxone q 24 hours IV (Ciprofloxacin and Clindamycin if allergic to Ceftriaxone) ! · Azithromycin or other -
Right Heart Pressures in Bronchial Asthma
Thorax: first published as 10.1136/thx.26.1.39 on 1 January 1971. Downloaded from Thorax (1971), 26, 39. Right heart pressures in bronchial asthma R. F. GUNSTONE St. George's Hospital, London S.W.1 Right heart pressures, electrocardiograms, blood gases, and peak expiratory flow rates were measured in nine patients admitted to hospital with severe bronchial asthma. Low or normal right heart pressures were found despite electrocardiographic changes in five patients consisting of right atrial P waves, abnormal right axis deviation, and in one patient T-wave changes in pre- cordial leads. These electrocardiographic changes reverted towards normal on recovery of the patient from the asthmatic attack. Electrocardiographic changes suggestive of right The procedure was carried out in the general ward heart embarrassment have been noted in acute with the patient in the sitting position supported at 60 bronchial asthma, particularly right atrial P waves to 90 degrees to the horizontal because orthopnoea (P and abnormal right axis deviation was always present. Immediately after catheterization pulmonale) the peak expiratory flow rate was measured with a (Harkavy and Romanoff, 1942; Miyamato, Wright peak flow meter (Wright and McKerrow, Bastaroli, and Hoffman, 1961; Ambiavagar, 1959) and blood (capillary or arterial) was taken for Jones and Roberts, 1967). These observations measurement of pH, Pco2, and standard bicarbonate raise the possibility that death in bronchial asthma by the Astrup method (Astrup, J0rgensen, Andersen, may be due to acute cor pulmonale although and Engel, 1960). The peak flow rate and electro- copyright. necropsy evidence is against this suggestion (Earle, cardiogram were repeated after recovery. -

Severe Asthma Is Associated with a Remodeling of the Pulmonary Arteries in Horses
bioRxiv preprint doi: https://doi.org/10.1101/2020.04.15.042903; this version posted April 17, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Severe asthma is associated with a remodeling of the pulmonary arteries in horses Remodeling of pulmonary arteries in severe equine asthma Serena Ceriotti1,2, Michela Bullone1, Mathilde Leclere1, Francesco Ferrucci2, Jean-Pierre Lavoie1* 1 Department of Clinical Sciences, Faculty of Veterinary Medicine, University of Montreal, Saint- Hyacinthe, Quebec, Canada 2 Department of Health, Animal Science and Food Safety, Università degli Studi di Milano, Milano, Italy Dr. Ceriotti current address is Department of Clinical Sciences, College of Veterinary Medicine, Auburn University, Auburn, Alabama, USA Dr. Bullone current address is Department of Veterinary Science, Università degli Studi di Torino, Grugliasco, Italy *Corresponding author: [email protected] Serena Ceriotti and Jean-Pierre Lavoie conceived and designed the work. Serena Ceriotti, Michela Bullone and Mathilde Leclere acquired clinical data, collected, processed and prepared histological and immunostained samples. Serena Ceriotti performed histomorphometric studies and statistical analysis. Serena Ceriotti, Jean-Pierre Lavoie and Francesco Ferrucci prepared and edited the manuscript prior to submission. Michela Bullone and Mathilde Leclere edited the manuscript prior to submission. 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.04.15.042903; this version posted April 17, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity.