Genes Covered and Disorders Detected by X-HR Microarray
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Moderate the MAOA-L Allele Expression with CRISPR/Cas9 System
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 23 April 2018 doi:10.20944/preprints201804.0275.v1 1 Review 2 Moderate the MAOA-L Allele Expression with CRISPR/Cas9 System 3 Martin L. Nelwan 4 Department of Animal Science – Other 5 Nelwan Institution for Human Resource Development 6 Jl. A. Yani No. 24 7 Palu, Sulawesi Tengah, Indonesia 8 Email: [email protected] 9 Abstract: Antisocial behavior is a behavior disorder inherited according to the inheritance of X-linked 10 chromosome. Mutations in the MAOA gene can cause different behaviors in humans. These can comprise 11 violent behavior or antisocial behavior. Low MAOA (MAOA-L) allele activity can cause antisocial 12 behavior in both healthy and unhealthy people. Antisocial from healthy males can originate from 13 maltreatment during childhood. There are no drugs for the treatment of antisocial behavior permanently 14 at this time. MAOA inhibitor can reverse antisocial behavior in animal models. To cure antisocial 15 behavior in the future, the CRISPR/Cas9 system in combination with iPSCs or ssODN methods for 16 instance can be used. This system has succeeded to correct erroneous segments in the F8 gene and F9 17 gene. Both genes occupy the X chromosome. The MAOA gene also occupies the X chromosome. It seems 18 that CRISPR/Cas9 system may be a beneficial tool to edit erroneous segments in the MAOA gene to treat 19 antisocial behavior. 20 Keywords: advanced therapy, aggressive, antisocial, behavior, MAOA. 21 22 1. Introduction 23 Antisocial behavior is a hereditary disorder inherited through an X-linked recessive inheritance 24 pattern. -

MR Imaging of Kallmann Syndrome, a Genetic Disorder of Neuronal Migration Affecting the Olfactory and Genital Systems
MR Imaging of Kallmann Syndrome, a Genetic Disorder of Neuronal Migration Affecting the Olfactory and Genital Systems 1 2 2 3 4 Charles L. Truwit, ' A. James Barkovich, Melvin M. Grumbach, and John J. Martini PURPOSE: We report the MR findings in nine patients with clinical and laboratory evidence of Kallmann syndrome (KS), a genetic disorder of olfactory and gonadal development. In patients with KS, cells that normally express luteinizing hormone-releasing hormone fail to migrate from the medial olfactory placode along the terminalis nerves into the forebrain. In addition, failed neuronal migration from the lateral olfactory placode along the olfactory fila to the forebrain results in aplasia or hypoplasia of the olfactory bulbs and tracts. Patients with KS, therefore, suffer both reproductive and olfactory dysfunction. METHODS: Nine patients with KS underwent direct coronal MR of their olfactory regions in order to assess the olfactory sulci, bulbs, and tracts. A lOth patient had MR findings of KS, although the diagnosis is not yet confirmed by laboratory tests. RESULTS: Abnormalities of the olfactory system were identified in all patients. In particular, the anterior portions of the olfactory sulci were uniformly hypoplastic. The olfactory bulbs and tracts appeared hypoplastic or aplastic in all patients in whom the bulb/ tract region was satisfactorily imaged. In two (possibly three) patients, prominent soft tissue in the region of the bulbs suggests radiographic evidence of neurons that have been arrested before migration. CONCLUSIONS: Previous investigators of patients with KS used axial MR images to demonstrate hypoplasia of the olfactory sulci but offered no assessment of the olfactory bulbs. -
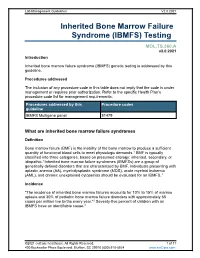
Inherited Bone Marrow Failure Syndrome (IBMFS) Testing
Lab Management Guidelines V2.0.2021 Inherited Bone Marrow Failure Syndrome (IBMFS) Testing MOL.TS.360.A v2.0.2021 Introduction Inherited bone marrow failure syndrome (IBMFS) genetic testing is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline IBMFS Multigene panel 81479 What are inherited bone marrow failure syndromes Definition Bone marrow failure (BMF) is the inability of the bone marrow to produce a sufficient quantity of functional blood cells to meet physiologic demands.1 BMF is typically classified into three categories, based on presumed etiology: inherited, secondary, or idiopathic.1 Inherited bone marrow failure syndromes (IBMFSs) are a group of genetically defined disorders that are characterized by BMF. Individuals presenting with aplastic anemia (AA), myelodysplastic syndrome (MDS), acute myeloid leukemia (AML), and chronic unexplained cytopenias should be evaluated for an IBMFS.1 Incidence "The incidence of inherited bone marrow failures accounts for 10% to 15% of marrow aplasia and 30% of pediatric bone marrow failure disorders with approximately 65 cases per million live births every year."2 Seventy-five percent of children with an IBMFS have an identifiable cause.2 ©2021 eviCore healthcare. All Rights Reserved. 1 of 17 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V2.0.2021 Symptoms While specific features may vary by each type of IBMFS, features that are present in most IBMFSs include bone marrow failure with single or multi-lineage cytopenia. -

Open Full Page
CCR PEDIATRIC ONCOLOGY SERIES CCR Pediatric Oncology Series Recommendations for Childhood Cancer Screening and Surveillance in DNA Repair Disorders Michael F. Walsh1, Vivian Y. Chang2, Wendy K. Kohlmann3, Hamish S. Scott4, Christopher Cunniff5, Franck Bourdeaut6, Jan J. Molenaar7, Christopher C. Porter8, John T. Sandlund9, Sharon E. Plon10, Lisa L. Wang10, and Sharon A. Savage11 Abstract DNA repair syndromes are heterogeneous disorders caused by around the world to discuss and develop cancer surveillance pathogenic variants in genes encoding proteins key in DNA guidelines for children with cancer-prone disorders. Herein, replication and/or the cellular response to DNA damage. The we focus on the more common of the rare DNA repair dis- majority of these syndromes are inherited in an autosomal- orders: ataxia telangiectasia, Bloom syndrome, Fanconi ane- recessive manner, but autosomal-dominant and X-linked reces- mia, dyskeratosis congenita, Nijmegen breakage syndrome, sive disorders also exist. The clinical features of patients with DNA Rothmund–Thomson syndrome, and Xeroderma pigmento- repair syndromes are highly varied and dependent on the under- sum. Dedicated syndrome registries and a combination of lying genetic cause. Notably, all patients have elevated risks of basic science and clinical research have led to important in- syndrome-associated cancers, and many of these cancers present sights into the underlying biology of these disorders. Given the in childhood. Although it is clear that the risk of cancer is rarity of these disorders, it is recommended that centralized increased, there are limited data defining the true incidence of centers of excellence be involved directly or through consulta- cancer and almost no evidence-based approaches to cancer tion in caring for patients with heritable DNA repair syn- surveillance in patients with DNA repair disorders. -

Mcleod Neuroacanthocytosis Syndrome
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health. Pagon RA, Adam MP, Ardinger HH, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993- 2017. McLeod Neuroacanthocytosis Syndrome Hans H Jung, MD Department of Neurology University Hospital Zurich Zurich, Switzerland [email protected] Adrian Danek, MD Neurologische Klinik Ludwig-Maximilians-Universität München, Germany ed.uml@kenad Ruth H Walker, MD, MBBS, PhD Department of Neurology Veterans Affairs Medical Center Bronx, New York [email protected] Beat M Frey, MD Blood Transfusion Service Swiss Red Cross Schlieren/Zürich, Switzerland [email protected] Christoph Gassner, PhD Blood Transfusion Service Swiss Red Cross Schlieren/Zürich, Switzerland [email protected] Initial Posting: December 3, 2004; Last Update: May 17, 2012. Summary Clinical characteristics. McLeod neuroacanthocytosis syndrome (designated as MLS throughout this review) is a multisystem disorder with central nervous system (CNS), neuromuscular, and hematologic manifestations in males. CNS manifestations are a neurodegenerative basal ganglia disease including (1) movement disorders, (2) cognitive alterations, and (3) psychiatric symptoms. Neuromuscular manifestations include a (mostly subclinical) sensorimotor axonopathy and muscle weakness or atrophy of different degrees. Hematologically, MLS is defined as a specific blood group phenotype (named after the first proband, Hugh McLeod) that results from absent expression of the Kx erythrocyte antigen and weakened expression of Kell blood group antigens. The hematologic manifestations are red blood cell acanthocytosis and compensated hemolysis. Allo-antibodies in the Kell and Kx blood group system can cause strong reactions to transfusions of incompatible blood and severe anemia in newborns of Kell-negative mothers. -

The Counsyl Foresight™ Carrier Screen
The Counsyl Foresight™ Carrier Screen 180 Kimball Way | South San Francisco, CA 94080 www.counsyl.com | [email protected] | (888) COUNSYL The Counsyl Foresight Carrier Screen - Disease Reference Book 11-beta-hydroxylase-deficient Congenital Adrenal Hyperplasia .................................................................................................................................................................................... 8 21-hydroxylase-deficient Congenital Adrenal Hyperplasia ...........................................................................................................................................................................................10 6-pyruvoyl-tetrahydropterin Synthase Deficiency ..........................................................................................................................................................................................................12 ABCC8-related Hyperinsulinism........................................................................................................................................................................................................................................ 14 Adenosine Deaminase Deficiency .................................................................................................................................................................................................................................... 16 Alpha Thalassemia............................................................................................................................................................................................................................................................. -

Experiences of Rare Diseases: an Insight from Patients and Families
Experiences of Rare Diseases: An Insight from Patients and Families Unit 4D, Leroy House 436 Essex Road London N1 3QP tel: 02077043141 fax: 02073591447 [email protected] www.raredisease.org.uk By Lauren Limb, Stephen Nutt and Alev Sen - December 2010 Web and press design www.raredisease.org.uk WordsAndPeople.com About Rare Disease UK Rare Disease UK (RDUK) is the national alliance for people with rare diseases and all who support them. Our membership is open to all and includes patient organisations, clinicians, researchers, academics, industry and individuals with an interest in rare diseases. RDUK was established by Genetic RDUK is campaigning for a Alliance UK, the national charity strategy for integrated service of over 130 patient organisations delivery for rare diseases. This supporting all those affected by would coordinate: genetic conditions, in conjunction with other key stakeholders | Research in November 2008 following the European Commission’s | Prevention and diagnosis Communication on Rare Diseases: | Treatment and care Europe’s Challenges. | Information Subsequently RDUK successfully | Commissioning and planning campaigned for the adoption of the Council of the European into one cohesive strategy for all Union’s Recommendation on patients affected by rare disease in an action in the field of rare the UK. As well as securing better diseases. The Recommendation outcomes for patients, a strategy was adopted unanimously by each would enable the most effective Member State of the EU (including use of NHS resources. the -

Program Nr: 1 from the 2004 ASHG Annual Meeting Mutations in A
Program Nr: 1 from the 2004 ASHG Annual Meeting Mutations in a novel member of the chromodomain gene family cause CHARGE syndrome. L.E.L.M. Vissers1, C.M.A. van Ravenswaaij1, R. Admiraal2, J.A. Hurst3, B.B.A. de Vries1, I.M. Janssen1, W.A. van der Vliet1, E.H.L.P.G. Huys1, P.J. de Jong4, B.C.J. Hamel1, E.F.P.M. Schoenmakers1, H.G. Brunner1, A. Geurts van Kessel1, J.A. Veltman1. 1) Dept Human Genetics, UMC Nijmegen, Nijmegen, Netherlands; 2) Dept Otorhinolaryngology, UMC Nijmegen, Nijmegen, Netherlands; 3) Dept Clinical Genetics, The Churchill Hospital, Oxford, United Kingdom; 4) Children's Hospital Oakland Research Institute, BACPAC Resources, Oakland, CA. CHARGE association denotes the non-random occurrence of ocular coloboma, heart defects, choanal atresia, retarded growth and development, genital hypoplasia, ear anomalies and deafness (OMIM #214800). Almost all patients with CHARGE association are sporadic and its cause was unknown. We and others hypothesized that CHARGE association is due to a genomic microdeletion or to a mutation in a gene affecting early embryonic development. In this study array- based comparative genomic hybridization (array CGH) was used to screen patients with CHARGE association for submicroscopic DNA copy number alterations. De novo overlapping microdeletions in 8q12 were identified in two patients on a genome-wide 1 Mb resolution BAC array. A 2.3 Mb region of deletion overlap was defined using a tiling resolution chromosome 8 microarray. Sequence analysis of genes residing within this critical region revealed mutations in the CHD7 gene in 10 of the 17 CHARGE patients without microdeletions, including 7 heterozygous stop-codon mutations. -

Peripheral Neuropathy in Complex Inherited Diseases: an Approach To
PERIPHERAL NEUROPATHY IN COMPLEX INHERITED DISEASES: AN APPROACH TO DIAGNOSIS Rossor AM1*, Carr AS1*, Devine H1, Chandrashekar H2, Pelayo-Negro AL1, Pareyson D3, Shy ME4, Scherer SS5, Reilly MM1. 1. MRC Centre for Neuromuscular Diseases, UCL Institute of Neurology and National Hospital for Neurology and Neurosurgery, London, WC1N 3BG, UK. 2. Lysholm Department of Neuroradiology, National Hospital for Neurology and Neurosurgery, London, WC1N 3BG, UK. 3. Unit of Neurological Rare Diseases of Adulthood, Carlo Besta Neurological Institute IRCCS Foundation, Milan, Italy. 4. Department of Neurology, University of Iowa, 200 Hawkins Drive, Iowa City, IA 52242, USA 5. Department of Neurology, University of Pennsylvania, Philadelphia, PA 19014, USA. * These authors contributed equally to this work Corresponding author: Mary M Reilly Address: MRC Centre for Neuromuscular Diseases, 8-11 Queen Square, London, WC1N 3BG, UK. Email: [email protected] Telephone: 0044 (0) 203 456 7890 Word count: 4825 ABSTRACT Peripheral neuropathy is a common finding in patients with complex inherited neurological diseases and may be subclinical or a major component of the phenotype. This review aims to provide a clinical approach to the diagnosis of this complex group of patients by addressing key questions including the predominant neurological syndrome associated with the neuropathy e.g. spasticity, the type of neuropathy, and the other neurological and non- neurological features of the syndrome. Priority is given to the diagnosis of treatable conditions. Using this approach, we associated neuropathy with one of three major syndromic categories - 1) ataxia, 2) spasticity, and 3) global neurodevelopmental impairment. Syndromes that do not fall easily into one of these three categories can be grouped according to the predominant system involved in addition to the neuropathy e.g. -

Disease Reference Book
The Counsyl Foresight™ Carrier Screen 180 Kimball Way | South San Francisco, CA 94080 www.counsyl.com | [email protected] | (888) COUNSYL The Counsyl Foresight Carrier Screen - Disease Reference Book 11-beta-hydroxylase-deficient Congenital Adrenal Hyperplasia .................................................................................................................................................................................... 8 21-hydroxylase-deficient Congenital Adrenal Hyperplasia ...........................................................................................................................................................................................10 6-pyruvoyl-tetrahydropterin Synthase Deficiency ..........................................................................................................................................................................................................12 ABCC8-related Hyperinsulinism........................................................................................................................................................................................................................................ 14 Adenosine Deaminase Deficiency .................................................................................................................................................................................................................................... 16 Alpha Thalassemia............................................................................................................................................................................................................................................................. -

Opsoclonus-Myoclonus Syndrome
OMS Opsoclonus-Myoclonus Syndrome REGISTRY POWERED BY NORD 10 11 Tr io Health © 2019 Trio Health Advisory Group, Inc.; NORD - National Organization for Rare Disorders, Inc. | All rights reserved. © 2019 Trio Health Advisory Group, Inc.; NORD - National Organization for Rare Disorders, Inc. | All rights reserved. Tr io Health Meet OMS Warrior ALEXA What is OMS? OPSOCLONUS-MYOCLONUS SYNDROME General Discussion Opsoclonus-myoclonus syndrome (OMS) is an inflammatory neurological disorder, often occurring as a paraneoplastic syndrome with neurological symptoms being the first sign of an occult tumor. It is characterized by associated ocular, motor, behavioral, sleep, and language disturbances. The onset is oftentimes abrupt and can be relatively severe, with the potential to become chronic unless the appropriate diagnosis and treatment are reached in a timely manner. Signs and Symptoms The component features of OMS include the presence of rapid, seemingly random eye movements in the horizontal, vertical, and diagonal directions (opsoclonus); an unsteady gait or inability to walk or stand (ataxia); and brief, repetitive, shock-like muscle spasms or tremors within the arms, legs, or hands interfering with normal use (myoclonus). Behavioral and sleep disturbances, including extreme irritability, inconsolable crying, reduced or fragmented sleep (insomnia), and rage attacks are common. Difficulty articulating speech (dysarthria), sometimes with complete loss of speech and language, may occur. Additional symptoms, such as decreased muscle tone (hypotonia) and vomiting, have also been noted. Causes The most common cause of OMS in young children is an occult (ie, a small, often hidden) tumor. The symptoms of OMS, as a paraneoplastic syndrome, presumably stem from the immune system attacking the tumor, leading to secondary inflammatory effects on the central nervous system. -

Genes in Eyecare Geneseyedoc 3 W.M
Genes in Eyecare geneseyedoc 3 W.M. Lyle and T.D. Williams 15 Mar 04 This information has been gathered from several sources; however, the principal source is V. A. McKusick’s Mendelian Inheritance in Man on CD-ROM. Baltimore, Johns Hopkins University Press, 1998. Other sources include McKusick’s, Mendelian Inheritance in Man. Catalogs of Human Genes and Genetic Disorders. Baltimore. Johns Hopkins University Press 1998 (12th edition). http://www.ncbi.nlm.nih.gov/Omim See also S.P.Daiger, L.S. Sullivan, and B.J.F. Rossiter Ret Net http://www.sph.uth.tmc.edu/Retnet disease.htm/. Also E.I. Traboulsi’s, Genetic Diseases of the Eye, New York, Oxford University Press, 1998. And Genetics in Primary Eyecare and Clinical Medicine by M.R. Seashore and R.S.Wappner, Appleton and Lange 1996. M. Ridley’s book Genome published in 2000 by Perennial provides additional information. Ridley estimates that we have 60,000 to 80,000 genes. See also R.M. Henig’s book The Monk in the Garden: The Lost and Found Genius of Gregor Mendel, published by Houghton Mifflin in 2001 which tells about the Father of Genetics. The 3rd edition of F. H. Roy’s book Ocular Syndromes and Systemic Diseases published by Lippincott Williams & Wilkins in 2002 facilitates differential diagnosis. Additional information is provided in D. Pavan-Langston’s Manual of Ocular Diagnosis and Therapy (5th edition) published by Lippincott Williams & Wilkins in 2002. M.A. Foote wrote Basic Human Genetics for Medical Writers in the AMWA Journal 2002;17:7-17. A compilation such as this might suggest that one gene = one disease.