Cognitive-Behavioral Therapy for Managing Pain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

How Do Children Cope with Global Climate Change? Coping Strategies, Engagement, and Well-Being
Journal of Environmental Psychology 32 (2012) 225e233 Contents lists available at SciVerse ScienceDirect Journal of Environmental Psychology journal homepage: www.elsevier.com/locate/jep How do children cope with global climate change? Coping strategies, engagement, and well-being Maria Ojala a,b,* a Department of Education, Box 2136, Uppsala University, 750 02 Uppsala, Sweden b Youth & Society, Örebro University, Örebro, Sweden article info abstract Article history: The aim of this questionnaire study was to explore how Swedish 12-year-olds (n ¼ 293) cope with Available online 8 March 2012 climate change, and how different coping strategies relate to environmental engagement and well-being. Three coping strategies were identified: problem-focused coping, de-emphasizing the seriousness of Keywords: climate change, and meaning-focused coping. Problem-focused and meaning-focused coping had posi- Climate change skepticism tive associations with measures of environmental engagement, while de-emphasizing the threat had Problem-focused coping negative associations with engagement. Problem-focused coping was positively related to general Meaning-focused coping negative affect, which was explained by the tendency for highly problem-focused children to worry more Optimism Negative affect about climate change. In contrast, the more meaning-focused coping the children used the less they Pro-environmental behavior experienced negative affect, and the more they experienced life satisfaction, general positive affect, purpose, and optimism. Finally, moderation analyses revealed that for children high on problem-focused coping; meaning-focused coping, purpose, and optimism worked as buffers against negative affect. The importance of positive emotions for constructive coping is discussed. Ó 2012 Elsevier Ltd. All rights reserved. -

Intravenous Iron Replacement Therapy (Feraheme®, Injectafer®, & Monoferric®)
UnitedHealthcare® Commercial Medical Benefit Drug Policy Intravenous Iron Replacement Therapy (Feraheme®, Injectafer®, & Monoferric®) Policy Number: 2021D0088F Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Community Plan Policy Coverage Rationale ....................................................................... 1 • Intravenous Iron Replacement Therapy (Feraheme®, Definitions ...................................................................................... 3 Injectafer®, & Monoferric®) Applicable Codes .......................................................................... 3 Background.................................................................................... 4 Benefit Considerations .................................................................. 4 Clinical Evidence ........................................................................... 5 U.S. Food and Drug Administration ............................................. 7 Centers for Medicare and Medicaid Services ............................. 8 References ..................................................................................... 8 Policy History/Revision Information ............................................. 9 Instructions for Use ....................................................................... 9 Coverage Rationale See Benefit Considerations This policy refers to the following intravenous iron replacements: Feraheme® (ferumoxytol) Injectafer® (ferric carboxymaltose) Monoferric® (ferric derisomaltose)* The following -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Cognitive Patterns and Coping Mechanisms in the Context of Internet Use
applied sciences Article Cognitive Patterns and Coping Mechanisms in the Context of Internet Use 1 1 1 2,3, 4 Cristina Costescu , Iulia Chelba , Adrian Ros, an , Attila Kovari * and Jozsef Katona 1 Special Education Department, Faculty of Psychology and Educational Sciences, Babes-Bolyai University, Sindicatelor Street no 7, 400029 Cluj-Napoca, Romania; [email protected] (C.C.); [email protected] (I.C.); [email protected] (A.R.) 2 Department of Natural Sciences and Environmental Protection, Institute of Engineering, University of Dunaujvaros, Tancsics M 1/A, 2400 Dunaujvaros, Hungary 3 Alba Regia Technical Faculty, Obuda University, Budai u 45., 8000 Szekesfehervar, Hungary 4 Institute of Computer Engineering, University of Dunaujvaros, Tancsics M 1/A, 2400 Dunaujvaros, Hungary; [email protected] * Correspondence: [email protected]; Tel.: +36-25-551-635 Abstract: Recent research indicates there are different cognitive patterns and coping mechanisms related to increased levels of Internet use and emotional distress in adolescents. This study aims to investigate the relationship between coping mechanisms, dysfunctional negative emotions, and Internet use. A total of 54 participants aged between 14 and 19 years old completed a questionnaire containing several measures and demographics information. We measured participants’ coping strategies, emotional distress, social and emotional loneliness, and their online behavior and Internet addiction using self-report questionnaires. In order to identify the relation between the investigated variables, we used correlation analysis and regression, and we tested one mediation model. The results showed that maladaptive coping strategies and Internet use were significant predictors of dysfunctional negative emotions. Moreover, passive wishful thinking, as a pattern of thinking, was Citation: Costescu, C.; Chelba, I.; associated with anxious and depressed feelings. -

Mir-205: a Potential Biomedicine for Cancer Therapy
cells Review miR-205: A Potential Biomedicine for Cancer Therapy Neeraj Chauhan 1,2 , Anupam Dhasmana 1,2, Meena Jaggi 1,2, Subhash C. Chauhan 1,2 and Murali M. Yallapu 1,2,* 1 Department of Immunology and Microbiology, School of Medicine, University of Texas Rio Grande Valley, McAllen, TX 78504, USA; [email protected] (N.C.); [email protected] (A.D.); [email protected] (M.J.); [email protected] (S.C.C.) 2 South Texas Center of Excellence in Cancer Research, School of Medicine, University of Texas Rio Grande Valley, McAllen, TX 78504, USA * Correspondence: [email protected]; Tel.: +1-(956)-296-1734 Received: 3 June 2020; Accepted: 21 August 2020; Published: 25 August 2020 Abstract: microRNAs (miRNAs) are a class of small non-coding RNAs that regulate the expression of their target mRNAs post transcriptionally. miRNAs are known to regulate not just a gene but the whole gene network (signaling pathways). Accumulating evidence(s) suggests that miRNAs can work either as oncogenes or tumor suppressors, but some miRNAs have a dual nature since they can act as both. miRNA 205 (miR-205) is one such highly conserved miRNA that can act as both, oncomiRNA and tumor suppressor. However, most reports confirm its emerging role as a tumor suppressor in many cancers. This review focuses on the downregulated expression of miR-205 and discusses its dysregulation in breast, prostate, skin, liver, gliomas, pancreatic, colorectal and renal cancers. This review also confers its role in tumor initiation, progression, cell proliferation, epithelial to mesenchymal transition, and tumor metastasis. -

Mental Wellness Statement Coping Cards
Mental Wellness Coping Statement Cards Coping Statements for Anxiety Coping Statements for Fear Coping Statements for Feeling Overwhelmed Coping Statements for Phobias Coping Statements for Panic Coping Statements for Pain Management Coping Statements for Disordered Eating Coping Statements for Anger Management Source: Lee, J. (n.d.). Use Coping Cards and Coping Statements to Improve Mental Health. Retrieved March 7, 2016, from http://www.choosehelp.com/topics/mental-health/rehab-for-patients-with-mental-health-challenges Coping Statements for Anxiety • Fighting this doesn’t help – so I’ll just relax and breathe deeply and let it float away. • This feeling isn’t comfortable, but I can handle it. • By relaxing through these feelings I learn to face my fears. • I can feel anxious and still deal with this situation. • This is not a real emergency. I can slow down and think about what I need to do. • This feeling will go away.1 • By staying present and focused on my task my anxiety will decrease. • These are just thoughts – not reality. • Anxiety won’t hurt me. • Feeling tense is natural. It tells me it’s time to use coping strategies. • Things are not as bad I am making them out to be. • Don’t discount the positives.2 Coping Statements for Fear • I’ve done this before so I can do it again. • I’ll be glad I did it when this is over.3 • I’ll feel better when I am actually in the situation. • I’ll just do the best I can. • By facing my fears I can overcome them. -

Allied Health Professionals Consumer Fact Sheet Board of Registration of Allied Health Professionals
Allied Health Professionals Consumer Fact Sheet Board of Registration of Allied Health Professionals The Board of Registration in Allied Health evaluates the qualifications of applicants for licensure and grants licenses to those who qualify. It establishes rules and regulations to ensure the integrity and competence of licensees. The Board is the link between the consumer and the allied health professional and, as such, promotes the public health, welfare and safety. Allied health professionals are occupational therapists and assistants, athletic trainers, and physical therapists and assistants. Occupational Therapists/Occupational Therapist Assistants Occupational therapists are health professionals who use occupational activities with specific goals in helping people of all ages to prevent, lessen or overcome physical, psychological or developmental disabilities. Occupational Therapists and Occupational Therapist Assistants help people with physical, psychological, or developmental problems regain abilities or adjust to handicaps. They work with physicians, physical and speech therapists, nurses, social workers, psychologists, teachers and other specialists. Patients may face handicaps, injuries, illness, psychological or social problems, or barriers due to age, economic, and cultural factors. Occupational Therapists: Consult with treatment teams to develop individualized treatment programs. Select and teach activities based on the needs and capabilities of each patient Evaluate each patient's progress, attitude and behavior. Design special equipment to aid patients with disabilities. Teach patients how to adjust to home, work, and social environments. Test and evaluate patients' physical and mental abilities. Educate others about occupational therapy. The goal of occupational therapy (OT) is for persons to achieve the highest level of independence after an injury or illness. OT addresses the whole person - cognitive, physical and emotional status. -

Massage Therapy Admission Packet
Caldwell Community College and Technical Institute Welcome to Caldwell Community College and Technical Institute. In this packet, you will find information about our Massage Therapy Program including costs, requirements, and details on how to prepare for your new career. Caldwell Campus 2855 Hickory Blvd Hudson, NC 28638 828.726.2200 Watauga Campus 372 Community College Drive Boone, NC 28607 828.297.8120 Amy Swink Massage Therapy Program Coordinator Watauga Campus E-mail: [email protected] Phone: (828)726-2242 and (828) 297-3811 MASSAGE THERAPY COURSE HEA 3021 This course is designed to prepare the student for the certification examination required for the North Carolina licensure application process. Through class work and practical “hands-on” training, students obtain a solid foundation for professional practice as a Massage Therapist. Upon successful completion of the course, the student is eligible to sit for the state exam and apply for state licensure in North Carolina. Competitive Admissions: Students, who successfully complete Massage Therapy training at CCC&TI, will receive two (2) points toward admission into the Physical Therapy Assistant program at CCC&TI Educational Pathway Example: Massage Therapy training > Licensure by examination > Licensed Massage and Bodywork Therapist Estimated Hourly Earnings: According to the Bureau of Labor Statistics website ( www.bls.gov/oes/current/oes319011.htm), current mean annual wage is $44,950. Employment Opportunities: • Chiropractic offices • Home care agencies • Hospice • Hospitals • Medical offices • Retirement homes • Self-employment • Spas FAQs • Is massage therapy training required to become licensed in North Carolina? o Yes. The North Carolina Board of Massage and Bodywork Therapy (NCBMBT) requires an applicant to successfully complete a state approved training program consisting of a minimum 500 in-class training hours. -
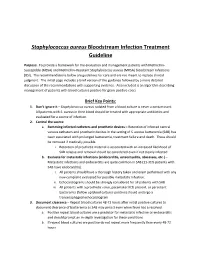
Staphylococcus Aureus Bloodstream Infection Treatment Guideline
Staphylococcus aureus Bloodstream Infection Treatment Guideline Purpose: To provide a framework for the evaluation and management patients with Methicillin- Susceptible (MSSA) and Methicillin-Resistant Staphylococcus aureus (MRSA) bloodstream infections (BSI). The recommendations below are guidelines for care and are not meant to replace clinical judgment. The initial page includes a brief version of the guidance followed by a more detailed discussion of the recommendations with supporting evidence. Also included is an algorithm describing management of patients with blood cultures positive for gram-positive cocci. Brief Key Points: 1. Don’t ignore it – Staphylococcus aureus isolated from a blood culture is never a contaminant. All patients with S. aureus in their blood should be treated with appropriate antibiotics and evaluated for a source of infection. 2. Control the source a. Removing infected catheters and prosthetic devices – Retention of infected central venous catheters and prosthetic devices in the setting of S. aureus bacteremia (SAB) has been associated with prolonged bacteremia, treatment failure and death. These should be removed if medically possible. i. Retention of prosthetic material is associated with an increased likelihood of SAB relapse and removal should be considered even if not clearly infected b. Evaluate for metastatic infections (endocarditis, osteomyelitis, abscesses, etc.) – Metastatic infections and endocarditis are quite common in SAB (11-31% patients with SAB have endocarditis). i. All patients should have a thorough history taken and exam performed with any new complaint evaluated for possible metastatic infection. ii. Echocardiograms should be strongly considered for all patients with SAB iii. All patients with a prosthetic valve, pacemaker/ICD present, or persistent bacteremia (follow up blood cultures positive) should undergo a transesophageal echocardiogram 3. -

Trauma-2020.Pdf
© Mind 2020 Trauma Explains what trauma is and how it affects your mental health, including how you can help yourself, what treatments are available and how to overcome barriers to getting the right support. Also includes tips for people who want to support someone who has gone through trauma. If you require this information in Word document format for compatibility with screen readers, please email: [email protected] Contents What is trauma? ................................................................................................................... 2 How could trauma affect me? .............................................................................................. 4 How can I cope right now? .................................................................................................. 8 How can I cope in the long term? ....................................................................................... 10 What treatments could help? ............................................................................................... 14 How can I overcome barriers? ............................................................................................ 17 How can other people help? ............................................................................................... 19 Useful contacts ................................................................................................................... 23 1 © Mind 2020 What is trauma? Going through very stressful, frightening or distressing events is sometimes -
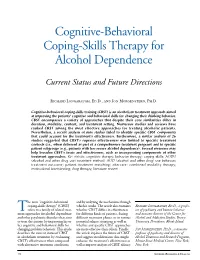
Cognitive-Behavioral Coping-Skills Therapy for Alcohol Dependence
Cognitive-Behavioral Coping-Skills Therapy for Alcohol Dependence Current Status and Future Directions Richard Longabaugh, Ed.D., and Jon Morgenstern, Ph.D. Cognitive-behavioral coping-skills training (CBST) is an alcoholism treatment approach aimed at improving the patients’ cognitive and behavioral skills for changing their drinking behavior. CBST encompasses a variety of approaches that despite their core similarities differ in duration, modality, content, and treatment setting. Numerous studies and reviews have ranked CBST among the most effective approaches for treating alcoholic patients. Nevertheless, a recent analysis of nine studies failed to identify specific CBST components that could account for the treatment’s effectiveness. Furthermore, a similar analysis of 26 studies suggested that CBST’s superior effectiveness was limited to specific treatment contexts (i.e., when delivered as part of a comprehensive treatment program) and to specific patient subgroups (e.g., patients with less severe alcohol dependence). Several measures may help broaden CBST’s focus and effectiveness, such as incorporating components of other treatment approaches. KEY WORDS: cognitive therapy; behavior therapy; coping skills; AODU (alcohol and other drug use) treatment method; AOD (alcohol and other drug) use behavior; treatment outcome; patient-treatment matching; aftercare; combined modality therapy; motivational interviewing; drug therapy; literature review he term “cognitive-behavioral and by analyzing the mechanisms through coping-skills therapy” -
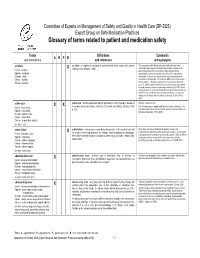
Glossary of Terms Related to Patient and Medication Safety
Committee of Experts on Management of Safety and Quality in Health Care (SP-SQS) Expert Group on Safe Medication Practices Glossary of terms related to patient and medication safety Terms Definitions Comments A R P B and translations and references and synonyms accident accident : an unplanned, unexpected, and undesired event, usually with adverse “For many years safety officials and public health authorities have Xconsequences (Senders, 1994). discouraged use of the word "accident" when it refers to injuries or the French : accident events that produce them. An accident is often understood to be Spanish : accidente unpredictable -a chance occurrence or an "act of God"- and therefore German : Unfall unavoidable. However, most injuries and their precipitating events are Italiano : incidente predictable and preventable. That is why the BMJ has decided to ban the Slovene : nesreča word accident. (…) Purging a common term from our lexicon will not be easy. "Accident" remains entrenched in lay and medical discourse and will no doubt continue to appear in manuscripts submitted to the BMJ. We are asking our editors to be vigilant in detecting and rejecting inappropriate use of the "A" word, and we trust that our readers will keep us on our toes by alerting us to instances when "accidents" slip through.” (Davis & Pless, 2001) active error X X active error : an error associated with the performance of the ‘front-line’ operator of Synonym : sharp-end error French : erreur active a complex system and whose effects are felt almost immediately. (Reason, 1990, This definition has been slightly modified by the Institute of Medicine : “an p.173) error that occurs at the level of the frontline operator and whose effects are Spanish : error activo felt almost immediately.” (Kohn, 2000) German : aktiver Fehler Italiano : errore attivo Slovene : neposredna napaka see also : error active failure active failures : actions or processes during the provision of direct patient care that Since failure is a term not defined in the glossary, its use is not X recommended.