A Dose-Response Meta-Analysis of the Impact of Body Mass Index on Stroke and All-Cause Mortality in Stroke Patients: a Paradox Within a Paradox
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Why Do We Get Fat?
Biology ︱ Professor John Speakman and Dr Sumei Hu One version of this framework states that animals have certain protein demands they need to meet. Consequently, Why do we get fat? if the protein content of the diet Evidence from a large diet trial in mice decreases, the animal must eat more to reach its protein goal and this then leads to overconsumption of energy. This is Professor John Speakman, besity is a global health issue. intake drives weight gain, then decreased called the ‘protein leverage hypothesis’. who is a 1000 talents ‘A’ A World Health Organization fat intake will increase weight loss. Fast The Atkin’s and ketogenic diets may professor at the Chinese Oreport in 2014 estimated there forward several years, into the 1980s and work because they provide high amounts Academy of Sciences, Institute were 1.9 billion overweight adults in the 90s, and the main culprit was claimed to of protein that mean individuals stop of Genetics and Developmental world, with 600 million of those having be refined carbohydrates and hence diets consuming food before their energy Biology,Beijing and a Professor obesity. It is well known that having focussing on fibre and low glycaemic requirements are met. An alternative at the University of Aberdeen, obesity is strongly associated with many index foods became the most popular idea is the energy regulation model. In UK, is interested in factors other health risks, such as cardiovascular methods to reverse obesity. Then in the this case, the suggestion is that animals Speakman (seated centre) with some of the research team that performed the large mouse diet study. -
6 Spring Resource 2010 Vickifinal:First Draft.Qxd
news THE ROYAL SOCIETY OF EDINBURGH ISSUE 27 SPRING 2010 RESOURCE THE NEWSLETTER OF SCOTLAND’ S NATIONAL ACADEMY RSE LAUNCHES BUSINESS INNOVATION FORUM The RSE launched its recently established Business Innovation Forum with a Reception in the Garden Lobby of the Scottish Parliament on 28 January 2010. The invitation list, numbering around 100, included leading figures from business, academia and the public sector, as well as members of the Forum itself. RSE President, Lord Wilson of Tillyorn KT GCMG, is pictured at the event with John Swinney MSP, Cabinet Secretary for Finance and Sustainable Growth. The Forum has been created with the objectives of identifying and stimulating processes that will increase business innovation investment and suggesting how appropriate strategies should be developed in Scotland. Further information about the forum and more photographs from the evening appear on the back page. International Links Education Outreach Climate Change Debate Election 2010 On 1 March 2010 the Society announced Once admitted to the RSE the election of 48 new UK and international Fellows are encouraged to HONORARY Fellows to its 1500-strong Fellowship of contribute to the aims experts in the sciences, arts, humanities, and objectives of the Society, FELLOWS the professions, industry and commerce. including the provision of The new Fellows were elected after a expert policy advice to HONORARY FELLOWS SHALL BE rigorous four-stage selection process Government and Parliament, MEMBERS OF THE ROYAL HOUSE, culminating in a ballot of the entire outreach education OR PERSONS EMINENTLY Fellowship. Each new Fellow of the RSE programmes for young people, DISTINGUISHED IN ANY SUBJECT is recognised within his or her peer group and public engagement WITHIN THE DISCIPLINARY as having achieved excellence within their events including conferences DOMAINS OF THE SOCIETY discipline or profession. -

Different Impacts of Resources on Opposite Sex Ratings of Physical Attractiveness by Males and Females
ENS-06173; No of Pages 6 Evolution and Human Behavior xxx (2018) xxx–xxx Contents lists available at ScienceDirect Evolution and Human Behavior journal homepage: www.ehbonline.org Different impacts of resources on opposite sex ratings of physical attractiveness by males and females Guanlin Wang a,b,c, Minxuan Cao d, Justina Sauciuvenaite c, Ruth Bissland c,MeganHackere, Catherine Hambly c, Lobke M. Vaanholt c, Chaoqun Niu a, Mark D. Faries f,g, John R. Speakman a,c,⁎ a State Key Laboratory of Molecular Developmental Biology, Institute of Genetics and Developmental Biology, Chinese Academy of Sciences, Beijing 100101, China b University of Chinese Academy of Sciences, Beijing 100049, China c Institute of Biological and Environmental Sciences, University of Aberdeen, Aberdeen AB24 2TZ, UK d Mount Holyoke College, South Hadley, MA, USA e Stephen F. Austin State University, Nacogdoches, TX, USA f Family and Community Health, Texas A&M AgriLife Extension Service, TX, USA g College of Medicine, Texas A&M Health Science Centre, TX, USA article info abstract Article history: Parental investment hypotheses regarding mate selection suggest that human males should seek partners fea- Initial receipt 11 October 2017 tured by youth and high fertility. However, females should be more sensitive to resources that can be invested Revised 21 December 2017 on themselves and their offspring. Previous studies indicate that economic status is indeed important in male Final revision received 22 December 2017 attractiveness. However, no previous study has quantified and compared the impact of equivalent resources Available online xxxx on male and female attractiveness. Annual salary is a direct way to evaluate economic status. -

Download the Trustees' Report and Financial Statements 2018-2019
Science is Global Trustees’ report and financial statements for the year ended 31 March 2019 The Royal Society’s fundamental purpose, reflected in its founding Charters of the 1660s, is to recognise, promote, and support excellence in science and to encourage the development and use of science for the benefit of humanity. The Society is a self-governing Fellowship of distinguished scientists drawn from all areas of science, technology, engineering, mathematics and medicine. The Society has played a part in some of the most fundamental, significant, and life-changing discoveries in scientific history and Royal Society scientists – our Fellows and those people we fund – continue to make outstanding contributions to science and help to shape the world we live in. Discover more online at: royalsociety.org BELGIUM AUSTRIA 3 1 NETHERLANDS GERMANY 5 12 CZECH REPUBLIC SWITZERLAND 3 2 CANADA POLAND 8 1 Charity Case study: Africa As a registered charity, the Royal Society Professor Cheikh Bécaye Gaye FRANCE undertakes a range of activities that from Cheikh Anta Diop University 25 provide public benefit either directly or in Senegal, Professor Daniel Olago from the University of indirectly. These include providing financial SPAIN UNITED STATES Nairobi in Kenya, Dr Michael OF AMERICA 18 support for scientists at various stages Owor from Makerere University of their careers, funding programmes 33 in Uganda and Professor Richard that advance understanding of our world, Taylor from University College organising scientific conferences to foster London are working on ways to discussion and collaboration, and publishing sustain low-cost, urban water supply and sanitation systems scientific journals. -
Speech on the PIFI Scheme and Experiences of Living in China
BCAS Vol.31 No.1 2017 Speech on the PIFI Scheme and Experiences of Living in China John Speakman Buckingham Palace, Feb 27, 2017 Your Royal Highness, President Bai, distinguished guests, It is an honour for me to address you today to introduce the PIFI scheme and just say a little bit about my own experiences living and working in China. How I ended up in China Maybe I should start by explaining how I ended up in China. Seven years ago, I was on an internal flight from the Tibetan Plateau back to Beijing with a colleague from CAS that I had been working with for a long time. At that point I was visiting China about four times per year for 3-4 weeks each time. He said to me, “You know, you don’t have to International Fellowship Initiative. The main part of keep visiting China like this.” I thought at first that he this scheme provides money for students and post docs was trying to hint that he didn’t want to work with me to come and work with PIs in the Chinese Academy of anymore. But then he went on, “instead, you could Sciences. Some of you may not be aware, but in China work here and visit the UK.” He then told me about there is a quota of PhD students for each PI, and the something called the Thousand Talents Program. benefit of this scheme is that it allows you to grow your This idea kind of obsessed me. I spoke to my group beyond the quota. -

UK Longevity Influencers LONGEVITY 938 UK Longevity Influencers INTERNATIONAL
UK Longevity Influencers LONGEVITY 938 UK Longevity Influencers INTERNATIONAL Baroness Sally David Sinclair Greengross OBE Eric Kihlstrom Helen Whately John Bell Matt Hancock Andrew Scott Dmitry Charles Alessi Aubrey de Grey Tina Woods Jim Mellon David Amess Kaminskiy UK Longevity Influencers LONGEVITY 939 INTERNATIONAL Top Longevity Scientists and Experts Malcolm Tom George P. Helen R. Anders Martin Green Tim Spector Jackson Kirkwood Willis Griffiths Sandberg Narendra Qing-Jun Ilora Gillian Leslie Arnold Dame Denise Philippa Ben Franklin Patel Meng Finlay Turnberg Platt Whitford Linda Paul Keith Julia John David Kipling Suzanne Wait Jon Date Partridge Potter Neuberger Speakman UK Longevity Influencers LONGEVITY 940 INTERNATIONAL Top Longevity Scientists and Experts Manlio Thomas von Paul Thornalley Janet Thornton William Bains Richard Barker Richard Faragher Vinciguerra Zglinicki J. P. de Robert Freitas David Gems Andrew Krentz Aisling Burnand Anne McArdle Cleo Bishop Magalhaes Sally-Marie Dr Richard Siow John Pattison Maggie Throup Peter Adams Janet M. Lord Colin Blakemore Bamford 941 David Sinclair Director of the International Longevity Centre – UK David has worked in policy and research on ageing and demographic change for 15 years. David has a particular interest in older consumers, adult vaccination, active ageing, financial services, and the role of technology in an ageing society. He has a strong knowledge of UK and global ageing society issues, from healthcare to pensions and from housing to transport. David has worked extensively on the issue of adult vaccination over the past eight years. He was a leading member of the SAATI coalition and is a board member of the Coalition for Life Course Immunisation. -
University of Groningen the Rate of Living in Mice Vaanholt, Lobke Maria
University of Groningen The rate of living in mice Vaanholt, Lobke Maria IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2007 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Vaanholt, L. M. (2007). The rate of living in mice: Impacts of activity and temperature on energy metabolism and longevity. s.n. Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). The publication may also be distributed here under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license. More information can be found on the University of Groningen website: https://www.rug.nl/library/open-access/self-archiving-pure/taverne- amendment. Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 06-10-2021 The Rate of Living in Mice: Impacts of activity and temperature on energy metabolism and longevity The research reported in this thesis was carried out at the Behavioural Biology Group at the University of Groningen, The Netherlands and at the Rowett Institute in Aberdeen, Scotland. -

China Previous Awards
UKRI - BBSRC CHINA PARTNERING AWARDS 2003 - 2019 China Partnering Awards BBSRC’s support for facilitating international collaborations with China BBSRC’s International Relations Unit (IRU) seeks to enhance BBSRC’s influence and involvement at the forefront of international science, through taking advantage of international funding opportunities and capitalising on international links, both at policy and scientific levels. The China Partnering Awards have been established by BBSRC to specifically support UK- China collaborative activity. China Partnering Awards provide resources to leading BBSRC- funded researchers and groups, so that they have the resources to establish long-term relationships with Chinese scientists in areas of research that are of direct relevance to BBSRC’s current scientific strategy. The first annual call for the China Partnering Awards scheme was announced by BBSRC in 2003. Awards of up to £30,000, covering a four-year period, have typically been awarded. Since 2010, BBSRC has funded 54 China Partnering Awards, providing a financial contribution of approximately £1.5M. Funding from China Partnering Awards can be used to support exchanges of personnel and to access facilities and workshops, although no prescribed mechanisms have been set concerning how the award should be used. However, priority is given to proposals that aim to provide exchange opportunities to early career researchers and access facilities and expertise not currently available in the UK. The expectation is that China Partnering Awards will enable researchers to establish collaborations that will lead to the submission of joint research proposals, either through UKRI or other funding organisations. A list of proposals that have been awarded by BBSRC since 2003 is shown below. -
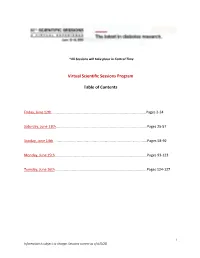
Virtual Scientific Sessions Program
*All Sessions will take place in Central Time Virtual Scientific Sessions Program Table of Contents Friday, June 12th……………………………………………………………………………………………Pages 2-24 Saturday, June 13th……………………………………………………………………….……………….Pages 25-57 Sunday, June 14th…………………………………………………………………………………………..Pages 58-92 Monday, June 15th………………………………………………………………………………………...Pages 93-123 Tuesday, June 16th…………………………………………………………………………………………Pages 124-127 1 Information is subject to change. Sessions current as of 6/5/20. FRIDAY, JUNE 12, 2020 Scientific Sessions 11:30 a.m.-12:30 p.m. Mini-Symposium Theme Area: Acute and Chronic Complications Debate—Technology Alone Can Solve the Problem of Hypoglycemia in Diabetes Chair: Belinda P. Childs, APRN, MN, BC-ADM, CDE 11:30 a.m.-12:00 p.m. For—Technology Alone Can Solve the Problem of Hypoglycemia Richard M. Bergenstal, MD 12:00 p.m.-12:30 p.m. Against—Technology Alone Can Solve the Problem of Hypoglycemia Emma G. Wilmot, MD Mini-Symposium Theme Area: Acute and Chronic Complications Is a Routine Lipid Panel Sufficient for Determining Cardiovascular Risk? Chair: Alan Chait, MD 11:30 a.m.-12:00 p.m. When Should You Order Advanced Lipoprotein Testing? Ronald M. Krauss, MD 12:00 p.m.-12:30 p.m. When Should You Order Coronary Calcium Scans? Matthew Budoff, MD Mini-Symposium Theme Area: Acute and Chronic Complications Sex Differences in Renal and Cardiovascular Disease in Diabetes Chair: Susanne Nicholas, MD, MPH, PhD 11:30 a.m.-12:00 p.m. Pathophysiology of Sex Differences in Micro- and Macrovascular Complications in Diabetes Mellitus Christine Maric-Bilkan, PhD 12:00 p.m.-12:30 p.m. Is There a Role of Sex in the Progression of Renal and Cardiovascular Disease in Diabetes? Joel Neugarten, MD, JD Mini-Symposium Theme Area: Behavioral Medicine, Clinical Nutrition, Education, and Exercise Improving Type 1 Diabetes Management in Young Adults—Time to (Re)Strategize? Chair: Jessica Pierce, PhD 11:30 a.m.-11:50 a.m. -

Continuing Its Long History of Influential Scientific Publishing, Phil
SUBSCRIPTIONS In 2019 Phil. Trans. R. Soc. B (ISSN 0962-8436) will be published Continuing its long history of infl uential scientifi c publishing, Phil. Trans. R. Soc. B 26 times a year. For more details of publishes high quality theme issues on topics of current importance and general subscriptions and single issue sales interest within the life sciences, guest-edited by leading authorities and comprising please contact our fulfi lment agent: new research, reviews and opinions from prominent researchers. Each issue Turpin Distribution aims to create an original and authoritative synthesis, often bridging traditional The Royal Society Customer Services Pegasus Drive disciplines, which showcases current developments and provides a foundation for Stratton Business Park future research, applications and policy decisions. Biggleswade SG18 8TQ United Kingdom royalsocietypublishing.org/journal/rstb T +44 1767 604951 F +44 1767 601640 E [email protected] EDITOR Karen Liu Alternatively, please contact our customer John Pickett Satyajit Mayor service team at: Ewa Paluch E [email protected] SENIOR COMMISSIONING EDITOR Jean-Paul Vincent Helen Eaton Roland Wedlich-Söldner PRICES FOR 2019 PRODUCTION EDITOR Neuroscience and cognition Online Online Simon Clackson Anna Borghi only and print Nicole Creanza EDITORIAL BOARD Andreas Engel £ UK/rest of World £2649 £3708 Organismal, environmental Barry Everitt and evolutionary biology Kristine Krug € Europe €3444 €4821 Tim Benton William Marslen-Wilson $ US/Canada $5014 $7019 Dora Biro -

China Partnering Awards 2003 - 2020
UKRI - BBSRC CHINA PARTNERING AWARDS 2003 - 2020 China Partnering Awards BBSRC’s support for facilitating international collaborations with China BBSRC’s International Relations Unit (IRU) seeks to enhance BBSRC’s influence and involvement at the forefront of international science, through taking advantage of international funding opportunities and capitalising on international links, both at policy and scientific levels. The China Partnering Awards have been established by BBSRC to specifically support UK- China collaborative activity. China Partnering Awards provide resources to leading BBSRC- funded researchers and groups, so that they have the resources to establish long-term relationships with Chinese scientists in areas of research that are of direct relevance to BBSRC’s current scientific strategy. The first annual call for the China Partnering Awards scheme was announced by BBSRC in 2003. Awards of up to £30,000, covering a four-year period, have typically been awarded. Since 2010, BBSRC has funded 54 China Partnering Awards, providing a financial contribution of approximately £1.5M. Funding from China Partnering Awards can be used to support exchanges of personnel and to access facilities and workshops, although no prescribed mechanisms have been set concerning how the award should be used. However, priority is given to proposals that aim to provide exchange opportunities to early career researchers and access facilities and expertise not currently available in the UK. The expectation is that China Partnering Awards will enable researchers to establish collaborations that will lead to the submission of joint research proposals, either through UKRI or other funding organisations. A list of proposals that have been awarded by BBSRC since 2003 is shown below. -

Physiologist a Publication of the American Physiological Society Volume 45, Number 4 Integrating the Life Sciences from Molecule to Organism August 2002
The Physiologist A Publication of The American Physiological Society Volume 45, Number 4 Integrating the Life Sciences from Molecule to Organism August 2002 The Power of Comparative Physiology: Evolution, Integration, and Application San Diego, California August 24-28, 2002 A Publication of The American Physiological Society Integrating the Life Sciences from Molecule to Organism THE Volume 45, Number 4 Physiologist August 2002 The Status of Physiologists and Physiology at US Medical Schools Martin Frank and Marsha Lakes Matyas The status of physiology in academic medical schools has areas, increases in the numbers of graduate students enrolled been a concern of the American Physiological Society for over 50 in physiology degree programs and PhDs awarded in physiolo- years, starting in 1945 with a study chaired by E. F. Adolph (1) gy would be evident. Is this the case? If not, what would lead to and followed in 1958 by a study chaired by R. W. Gerard (11). a disparity between physiology and many other life sciences The APS has undertaken similar studies in the last two decades fields? Furthermore, numerous discussions and reports have as part of its efforts to define the future of the Society and the focused on the status of postdoctoral fellows in the US. What discipline. The most compelling was the study developed by the are the trends for postdoctoral fellows in physiology? Are they Long Range Planning Committee chaired by Ernst Knobil and comparable to other fields? What implications does the status of published by the Society in 1990 (10). It explored the status of postdoctoral fellows in physiology have for the field as a whole? the science of physiology, departments of physiology, and the American Physiological Society.