Long-Term Effects of Recombinant Human Insulin-Like Growth Factor I
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Repercussions of Inborn Errors of Immunity on Growth☆ Jornal De Pediatria, Vol
Jornal de Pediatria ISSN: 0021-7557 ISSN: 1678-4782 Sociedade Brasileira de Pediatria Goudouris, Ekaterini Simões; Segundo, Gesmar Rodrigues Silva; Poli, Cecilia Repercussions of inborn errors of immunity on growth☆ Jornal de Pediatria, vol. 95, no. 1, Suppl., 2019, pp. S49-S58 Sociedade Brasileira de Pediatria DOI: https://doi.org/10.1016/j.jped.2018.11.006 Available in: https://www.redalyc.org/articulo.oa?id=399759353007 How to cite Complete issue Scientific Information System Redalyc More information about this article Network of Scientific Journals from Latin America and the Caribbean, Spain and Journal's webpage in redalyc.org Portugal Project academic non-profit, developed under the open access initiative J Pediatr (Rio J). 2019;95(S1):S49---S58 www.jped.com.br REVIEW ARTICLE ଝ Repercussions of inborn errors of immunity on growth a,b,∗ c,d e Ekaterini Simões Goudouris , Gesmar Rodrigues Silva Segundo , Cecilia Poli a Universidade Federal do Rio de Janeiro (UFRJ), Faculdade de Medicina, Departamento de Pediatria, Rio de Janeiro, RJ, Brazil b Universidade Federal do Rio de Janeiro (UFRJ), Instituto de Puericultura e Pediatria Martagão Gesteira (IPPMG), Curso de Especializac¸ão em Alergia e Imunologia Clínica, Rio de Janeiro, RJ, Brazil c Universidade Federal de Uberlândia (UFU), Faculdade de Medicina, Departamento de Pediatria, Uberlândia, MG, Brazil d Universidade Federal de Uberlândia (UFU), Hospital das Clínicas, Programa de Residência Médica em Alergia e Imunologia Pediátrica, Uberlândia, MG, Brazil e Universidad del Desarrollo, -

Prevalence and Incidence of Rare Diseases: Bibliographic Data
Number 1 | January 2019 Prevalence and incidence of rare diseases: Bibliographic data Prevalence, incidence or number of published cases listed by diseases (in alphabetical order) www.orpha.net www.orphadata.org If a range of national data is available, the average is Methodology calculated to estimate the worldwide or European prevalence or incidence. When a range of data sources is available, the most Orphanet carries out a systematic survey of literature in recent data source that meets a certain number of quality order to estimate the prevalence and incidence of rare criteria is favoured (registries, meta-analyses, diseases. This study aims to collect new data regarding population-based studies, large cohorts studies). point prevalence, birth prevalence and incidence, and to update already published data according to new For congenital diseases, the prevalence is estimated, so scientific studies or other available data. that: Prevalence = birth prevalence x (patient life This data is presented in the following reports published expectancy/general population life expectancy). biannually: When only incidence data is documented, the prevalence is estimated when possible, so that : • Prevalence, incidence or number of published cases listed by diseases (in alphabetical order); Prevalence = incidence x disease mean duration. • Diseases listed by decreasing prevalence, incidence When neither prevalence nor incidence data is available, or number of published cases; which is the case for very rare diseases, the number of cases or families documented in the medical literature is Data collection provided. A number of different sources are used : Limitations of the study • Registries (RARECARE, EUROCAT, etc) ; The prevalence and incidence data presented in this report are only estimations and cannot be considered to • National/international health institutes and agencies be absolutely correct. -

MECHANISMS in ENDOCRINOLOGY: Novel Genetic Causes of Short Stature
J M Wit and others Genetics of short stature 174:4 R145–R173 Review MECHANISMS IN ENDOCRINOLOGY Novel genetic causes of short stature 1 1 2 2 Jan M Wit , Wilma Oostdijk , Monique Losekoot , Hermine A van Duyvenvoorde , Correspondence Claudia A L Ruivenkamp2 and Sarina G Kant2 should be addressed to J M Wit Departments of 1Paediatrics and 2Clinical Genetics, Leiden University Medical Center, PO Box 9600, 2300 RC Leiden, Email The Netherlands [email protected] Abstract The fast technological development, particularly single nucleotide polymorphism array, array-comparative genomic hybridization, and whole exome sequencing, has led to the discovery of many novel genetic causes of growth failure. In this review we discuss a selection of these, according to a diagnostic classification centred on the epiphyseal growth plate. We successively discuss disorders in hormone signalling, paracrine factors, matrix molecules, intracellular pathways, and fundamental cellular processes, followed by chromosomal aberrations including copy number variants (CNVs) and imprinting disorders associated with short stature. Many novel causes of GH deficiency (GHD) as part of combined pituitary hormone deficiency have been uncovered. The most frequent genetic causes of isolated GHD are GH1 and GHRHR defects, but several novel causes have recently been found, such as GHSR, RNPC3, and IFT172 mutations. Besides well-defined causes of GH insensitivity (GHR, STAT5B, IGFALS, IGF1 defects), disorders of NFkB signalling, STAT3 and IGF2 have recently been discovered. Heterozygous IGF1R defects are a relatively frequent cause of prenatal and postnatal growth retardation. TRHA mutations cause a syndromic form of short stature with elevated T3/T4 ratio. Disorders of signalling of various paracrine factors (FGFs, BMPs, WNTs, PTHrP/IHH, and CNP/NPR2) or genetic defects affecting cartilage extracellular matrix usually cause disproportionate short stature. -

Update on New GH-IGF Axis Genetic Defects
review Update on new GH-IGF axis genetic defects Gabriela A. Vasques1,2 1 Unidade de Endocrinologia https://orcid.org/0000-0002-6455-8682 Genética, Laboratório de Endocrinologia Celular e Nathalia L. M. Andrade1,2 https://orcid.org/0000-0002-1628-7881 Molecular (LIM25), Hospital das Clínicas, Faculdade de Fernanda A. Correa2 Medicina, Universidade de São https://orcid.org/0000-0003-2107-9494 Paulo, São Paulo, SP, Brasil 2 Alexander A. L. Jorge1,2 Unidade de Endocrinologia do https://orcid.org/0000-0003-2567-7360 Desenvolvimento, Laboratório de Hormônios e Genética Molecular (LIM42), Hospital das Clínicas, Faculdade de ABSTRACT Medicina, Universidade de São The somatotropic axis is the main hormonal regulator of growth. Growth hormone (GH), also known Paulo, São Paulo, SP, Brasil as somatotropin, and insulin-like growth factor 1 (IGF-1) are the key components of the somatotropic axis. This axis has been studied for a long time and the knowledge of how some molecules could Correspondence to: promote or impair hormones production and action has been growing over the last decade. The Alexander A. L. Jorge Laboratório de Endocrinologia enhancement of large-scale sequencing techniques has expanded the spectrum of known genes and Celular e Molecular (LIM25), several other candidate genes that could affect the GH-IGF1-bone pathway. To date, defects in more Faculdade de Medicina, than forty genes were associated with an impairment of the somatotropic axis. These defects can Universidade de São Paulo Av. Dr. Arnaldo, 455, affect from the secretion of GH to the bioavailability and action of IGF-1. Affected patients present a 5º andar, sala 5.340 large heterogeneous group of conditions associated with growth retardation. -

Genetic Disorder
Genetic disorder Single gene disorder Prevalence of some single gene disorders[citation needed] A single gene disorder is the result of a single mutated gene. Disorder Prevalence (approximate) There are estimated to be over 4000 human diseases caused Autosomal dominant by single gene defects. Single gene disorders can be passed Familial hypercholesterolemia 1 in 500 on to subsequent generations in several ways. Genomic Polycystic kidney disease 1 in 1250 imprinting and uniparental disomy, however, may affect Hereditary spherocytosis 1 in 5,000 inheritance patterns. The divisions between recessive [2] Marfan syndrome 1 in 4,000 and dominant types are not "hard and fast" although the [3] Huntington disease 1 in 15,000 divisions between autosomal and X-linked types are (since Autosomal recessive the latter types are distinguished purely based on 1 in 625 the chromosomal location of Sickle cell anemia the gene). For example, (African Americans) achondroplasia is typically 1 in 2,000 considered a dominant Cystic fibrosis disorder, but children with two (Caucasians) genes for achondroplasia have a severe skeletal disorder that 1 in 3,000 Tay-Sachs disease achondroplasics could be (American Jews) viewed as carriers of. Sickle- cell anemia is also considered a Phenylketonuria 1 in 12,000 recessive condition, but heterozygous carriers have Mucopolysaccharidoses 1 in 25,000 increased immunity to malaria in early childhood, which could Glycogen storage diseases 1 in 50,000 be described as a related [citation needed] dominant condition. Galactosemia -

Laron Syndrome
Laron syndrome Description Laron syndrome is a rare form of short stature that results from the body's inability to use growth hormone, a substance produced by the brain's pituitary gland that helps promote growth. Affected individuals are close to normal size at birth, but they experience slow growth from early childhood that results in very short stature. If the condition is not treated, adult males typically reach a maximum height of about 4.5 feet; adult females may be just over 4 feet tall. Other features of untreated Laron syndrome include reduced muscle strength and endurance, low blood sugar levels (hypoglycemia) in infancy, small genitals and delayed puberty, hair that is thin and fragile, and dental abnormalities. Many affected individuals have a distinctive facial appearance, including a protruding forehead, a sunken bridge of the nose (saddle nose), and a blue tint to the whites of the eyes (blue sclerae). Affected individuals have short limbs compared to the size of their torso, as well as small hands and feet. Adults with this condition tend to develop obesity. However, the signs and symptoms of Laron syndrome vary, even among affected members of the same family. Studies suggest that people with Laron syndrome have a significantly reduced risk of cancer and type 2 diabetes. Affected individuals appear to develop these common diseases much less frequently than their unaffected relatives, despite having obesity (a risk factor for both cancer and type 2 diabetes). However, people with Laron syndrome do not seem to have an increased lifespan compared with their unaffected relatives. Frequency Laron syndrome is a rare disorder. -

Blueprint Genetics Comprehensive Growth Disorders / Skeletal
Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders Panel Test code: MA4301 Is a 374 gene panel that includes assessment of non-coding variants. This panel covers the majority of the genes listed in the Nosology 2015 (PMID: 26394607) and all genes in our Malformation category that cause growth retardation, short stature or skeletal dysplasia and is therefore a powerful diagnostic tool. It is ideal for patients suspected to have a syndromic or an isolated growth disorder or a skeletal dysplasia. About Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders This panel covers a broad spectrum of diseases associated with growth retardation, short stature or skeletal dysplasia. Many of these conditions have overlapping features which can make clinical diagnosis a challenge. Genetic diagnostics is therefore the most efficient way to subtype the diseases and enable individualized treatment and management decisions. Moreover, detection of causative mutations establishes the mode of inheritance in the family which is essential for informed genetic counseling. For additional information regarding the conditions tested on this panel, please refer to the National Organization for Rare Disorders and / or GeneReviews. Availability 4 weeks Gene Set Description Genes in the Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ACAN# Spondyloepimetaphyseal dysplasia, aggrecan type, AD/AR 20 56 Spondyloepiphyseal dysplasia, Kimberley -
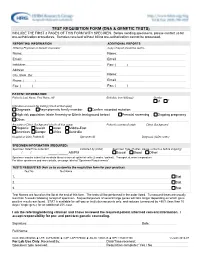
Test Requisition Form (Dna & Genetic Tests)
TEST REQUISITION FORM (DNA & GENETIC TESTS) INCLUDE THE FIRST 3 PAGES OF THIS FORM WITH SPECIMEN. Before sending specimens, please contact us for pre-authorization procedures. Samples received without billing pre-authorization cannot be processed. REPORTING INFORMATION ADDITIONAL REPORTS Ordering Physician or Genetic Counselor Copy of report should be sent to Name: Name: Email: Email: Institution: Fax: ( ) Address: City, State, Zip: Name: Phone: ( ) Email: Fax: ( ) Fax: ( ) PATIENT INFORMATION Patient's Last Name, First Name, MI Birthdate (mm/dd/yyyy) Gender M F Indication or reason for testing (check all that apply) Diagnosis Asymptomatic family member Confirm recorded mutation: High risk population (state Ancestry or Ethnic background below) Prenatal screening Ongoing pregnancy Other: Ancestry or Ethnic Background (check all that apply) Patient's country of origin Ethnic Background Hispanic Jewish Asian Middle-East Americas Europe Africa Australia Hospital or Clinic Patient ID Specimen ID Diagnosis (ICD9 codes) SPECIMEN INFORMATION (REQUIRED) Specimen Date/Time Collected Collected by (initial) Specimen Type (If other, please contact us before shipping) / / _____:_____ AM/PM Buccal Blood Other: Specimen may be submitted as whole blood or buccal epithelial cells (2 swabs / patient). Transport at room temperature. For other specimens and more details, see page labeled "Specimen Requirements". TESTS REQUESTED (Ask us to customize the requisition form for your practice) Test No. Test Name 1. Stat 2. Stat 3. Stat Test Names are found on the list at the end of this form. The tests will be performed in the order listed. Turnaround times are usually less than 5 weeks following receipt of specimen. Sequential panels of several large genes will take longer depending on which gene positive results are found. -

E-Chapter 2.P65
Chapter 2 / hGH Axis Molecular Mutations 41 II GROWTH 42 Part II / Growth Chapter 2 / hGH Axis Molecular Mutations 43 2 Molecular Mutations in the Human Growth Hormone Axis Zvi Laron, MD CONTENTS INTRODUCTION GROWTH HORMONE RELEASING HORMONE (GHRH) THE GHRH-RECEPTOR (GHRH-R) CONCLUSIONS HUMAN PITUITARY GROWTH HORMONE (hGH) MOLECULAR DEFECTS IN THE HUMAN GH GENE AND HORMONE CONCLUSION THE GROWTH HORMONE RECEPTOR GROWTH HORMONE BINDING PROTEIN (GHBP) MOLECULAR DEFECTS OF THE HUMAN GH RECEPTOR (LARON SYNDROME) DEFECTS OF THE GH-RECEPTOR (GH-R) PARTIAL GROWTH HORMONE INSENSITIVITY (GHI) INSULIN-LIKE GROWTH FACTOR-1 (IGF-1) INSULIN-LIKE GROWTH FACTOR BINDING PROTEINS (IGFBPS) DEFECTS OF THE IGF-1 GENE AND RECEPTOR GENOTYPE-PHENOTYPE RELATIONSHIP ACKNOWLEDGMENT REFERENCES INTRODUCTION Human growth hormone (hGH) is secreted from somatomammotrophic cells in the anterior pituitary in a pulsatile pattern that results from a diurnal rhythmically changing disequilibrium between two hypothalamic hormones: GHRH (GH-releasing hormone) and SMS (somatostatin = GH secretion inhibiting hormone) (1). GHRH induces hGH synthesis and secretion whenever the somatostatinergic tone is low (2). It is thus evident that SMS plays a central role in the regulation of GH secretion. The actions of SMS are not restricted to GH alone, but also affect other hormones, as seen in Fig. 1, which illu- strates the GH cascade. Not illustrated is the inhibitory effect of somatostatin on TSH, From: Contemporary Endocrinology: Developmental Endocrinology: From Research to Clinical Practice Edited by: E. A. Eugster and O. H. Pescovitz © Humana Press Inc., Totowa, NJ 43 44 Part II / Growth Fig. 1. The growth hormone axis. GH, growth hormone; GH-S, GH secretagog; GHRH, GH-releas- ing hormone; IGF-1, insulin-like growth factor-1; GHBP, GH binding protein; IGFBP, insulin-like growth factor; binding proteins; +, stimulates; −, inhibits. -

Laron Syndrome- a Disorder Associated with a Reduced Risk of Cancer: a Review on the Molecular Aspects
International Journal of Innovative Medicine and Health Science, Volume 12, 2020, 123-132 Laron Syndrome- A Disorder Associated with a Reduced Risk of Cancer: A Review on the Molecular Aspects Ksheera Karumbaiah1, Gopenath TS2, Raghu Nataraj1 and Kanthesh M. Basalingappa1* *1Division of Molecular Biology, Faculty of Life Sciences, JSS Academy of Higher Education and Research, SS Nagara, Mysuru, Karnataka, Pin code: 570015, India 2Division of Biotechnology, Faculty of Life Sciences, JSS Academy of Higher Education and Research, SS Nagara, Mysuru, Karnataka, Pin code: 570015, India ABSTRACT Laron syndrome (LS) or primary growth hormone insensitivity is a genetic disorder known for a type of dwarfism characterized by short stature, facial phenotype, obesity and unexpected high serum GH levels. The disorder is caused due to the mutation of Growth Hormone receptor (GHR) gene whose inability to synthesize IGF-I and other related molecules leads to insulin-like growth factor-1 (IGF-1) deficiency and was first described by Zvi Laron et al., in 1966 as a new type of dwarfism and has garnered interest among genetics and medical fraternities where the LS patients are known to have a lower cancer risk. The review presents the baseline clinical and genetic aspects of the condition along with a broader overview of hypothesized disease presentations of possible protective mechanisms against cancer induction. Keywords: Laron syndrome, Growth hormone receptor, Insulin-like growth factor-1, Dwarfism, Cancer protection Introduction Laron syndrome (LS) or Primary Growth Hormone Insensitivity is a form of genetic syndrome caused by the mutation of Growth Hormone receptor (GHR) gene leading to insulin-like growth factor-1 (IGF-1) deficiency [2]. -

A Case with Laron Syndrome
Case Report DOI: 10.14235/bas.galenos.2018.2385 Bezmialem Science 2019;7(3):251-4 A Case with Laron Syndrome İlker Tolga ÖZGEN1, Esra KUTLU1, Yaşar CESUR1, Gözde YEŞİL2 1Bezmialem Vakıf University Faculty of Medicine, Department of Pediatric Endocrinology, İstanbul, Turkey 2Bezmialem Vakıf University Faculty of Medicine, Department of Medical Genetics, İstanbul, Turkey ABSTRACT Laron syndrome (LS) is a rare disorder leading to short stature as a result of growth hormone (GH) insensitivity. It is caused by mutations in GH receptor gene and characterized by post-natal growth retardation, craniofacial abnormalities, high serum GH and low insulin-like growth factor-I (IGF-I) levels. Several different genetic mutations have been documented up to date. In this article, a patient with LS is reported. A 2-year-old female patient was admitted to the hospital with the complaint of short stature. Her height and weight was 71.7 cm [<3 p., -4.09 standard deviations (SDS)] and 9.7 kg (<3 p., -2.2 SDS) respectively. She had dysmorphic features such as maxillary hypoplasia, blue sclera, small hands and feet, and extreme proportionate shortness. She had a high basal serum GH level (61.879 ng/mL), whereas serum IGF-I (<10 ng/mL) and IGF-binding protein 3 (<0.54 ng/mL) concentrations were significantly low. Both clinical and laboratory measurements were consistent with LS. A missense variation leading to a stop codon (W182X) was determined in GH receptor gene. Recombinant IGF-I therapy improved height z-score from -4.09 to -3.4 SDS after 24-month treatment. In this report, we presented a case with LS. -

Genetic Testing Medical Policy – Genetics
Genetic Testing Medical Policy – Genetics Please complete all appropriate questions fully. Suggested medical record documentation: • Current History & Physical • Progress Notes • Family Genetic History • Genetic Counseling Evaluation *Failure to include suggested medical record documentation may result in delay or possible denial of request. PATIENT INFORMATION Name: Member ID: Group ID: PROCEDURE INFORMATION Genetic Counseling performed: c Yes c No **Please check the requested analyte(s), identify number of units requested, and provide indication/rationale for testing. 81400 Molecular Pathology Level 1 Units _____ c ACADM (acyl-CoA dehydrogenase, C-4 to C-12 straight chain, MCAD) (e.g., medium chain acyl dehydrogenase deficiency), K304E variant _____ c ACE (angiotensin converting enzyme) (e.g., hereditary blood pressure regulation), insertion/deletion variant _____ c AGTR1 (angiotensin II receptor, type 1) (e.g., essential hypertension), 1166A>C variant _____ c BCKDHA (branched chain keto acid dehydrogenase E1, alpha polypeptide) (e.g., maple syrup urine disease, type 1A), Y438N variant _____ c CCR5 (chemokine C-C motif receptor 5) (e.g., HIV resistance), 32-bp deletion mutation/794 825del32 deletion _____ c CLRN1 (clarin 1) (e.g., Usher syndrome, type 3), N48K variant _____ c DPYD (dihydropyrimidine dehydrogenase) (e.g., 5-fluorouracil/5-FU and capecitabine drug metabolism), IVS14+1G>A variant _____ c F13B (coagulation factor XIII, B polypeptide) (e.g., hereditary hypercoagulability), V34L variant _____ c F2 (coagulation factor 2) (e.g.,