UK Lipoedema’ Cohort
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Data
Figure 2S 4 7 A - C 080125 CSCs 080418 CSCs - + IFN-a 48 h + IFN-a 48 h + IFN-a 72 h 6 + IFN-a 72 h 3 5 MRFI 4 2 3 2 1 1 0 0 MHC I MHC II MICA MICB ULBP-1 ULBP-2 ULBP-3 ULBP-4 MHC I MHC II MICA MICB ULBP-1 ULBP-2 ULBP-3 ULBP-4 7 B 13 080125 FBS - D 080418 FBS - + IFN-a 48 h 12 + IFN-a 48 h + IFN-a 72 h + IFN-a 72 h 6 080125 FBS 11 10 5 9 8 4 7 6 3 MRFI 5 4 2 3 2 1 1 0 0 MHC I MHC II MICA MICB ULBP-1 ULBP-2 ULBP-3 ULBP-4 MHC I MHC II MICA MICB ULBP-1 ULBP-2 ULBP-3 ULBP-4 Molecule Molecule FIGURE 4S FIGURE 5S Panel A Panel B FIGURE 6S A B C D Supplemental Results Table 1S. Modulation by IFN-α of APM in GBM CSC and FBS tumor cell lines. Molecule * Cell line IFN-α‡ HLA β2-m# HLA LMP TAP1 TAP2 class II A A HC§ 2 7 10 080125 CSCs - 1∞ (1) 3 (65) 2 (91) 1 (2) 6 (47) 2 (61) 1 (3) 1 (2) 1 (3) + 2 (81) 11 (80) 13 (99) 1 (3) 8 (88) 4 (91) 1 (2) 1 (3) 2 (68) 080125 FBS - 2 (81) 4 (63) 4 (83) 1 (3) 6 (80) 3 (67) 2 (86) 1 (3) 2 (75) + 2 (99) 14 (90) 7 (97) 5 (75) 7 (100) 6 (98) 2 (90) 1 (4) 3 (87) 080418 CSCs - 2 (51) 1 (1) 1 (3) 2 (47) 2 (83) 2 (54) 1 (4) 1 (2) 1 (3) + 2 (81) 3 (76) 5 (75) 2 (50) 2 (83) 3 (71) 1 (3) 2 (87) 1 (2) 080418 FBS - 1 (3) 3 (70) 2 (88) 1 (4) 3 (87) 2 (76) 1 (3) 1 (3) 1 (2) + 2 (78) 7 (98) 5 (99) 2 (94) 5 (100) 3 (100) 1 (4) 2 (100) 1 (2) 070104 CSCs - 1 (2) 1 (3) 1 (3) 2 (78) 1 (3) 1 (2) 1 (3) 1 (3) 1 (2) + 2 (98) 8 (100) 10 (88) 4 (89) 3 (98) 3 (94) 1 (4) 2 (86) 2 (79) * expression of APM molecules was evaluated by intracellular staining and cytofluorimetric analysis; ‡ cells were treatead or not (+/-) for 72 h with 1000 IU/ml of IFN-α; # β-2 microglobulin; § β-2 microglobulin-free HLA-A heavy chain; ∞ values are indicated as ratio between the mean of fluorescence intensity of cells stained with the selected mAb and that of the negative control; bold values indicate significant MRFI (≥ 2). -

Gynoid Vs Android Fat Distribution
Gynoid vs android fat distribution Continue 20-09-2019Biology around the spread of android/ionoid On the DEXA scan you will see that it calculates the ratio of android gyoid. Android is described as the distribution of fat around the middle of the section, so around the waist (navel). Ginoid is the distribution of fat around the thighs, this region is located around the upper thighs. Where you store fat can help determine what type of shape you are and if you are more at risk of increasing visceral fat. If you store more fat around the android area (waist) it is considered the shape of an apple. Android/ginoid ratio of more than 1 will determine this, and you may be at greater risk of having high visceral fat (fat around the organs). If your A/G ratio is smaller than 1 you can see more fat stored around your hips. As a rule, ≤0.8, and males - 1. When a man's body fat % falls on some of the lower ranges it is common for the last bit of fat to be stored around the ginoid area. This ratio can be tracked over time to see if the fat is predominantly lost near one area or both. Where you store/distribute fat can also be transmitted through genetics, so it can be difficult to detect train certain areas. Biology! Android fat cells are predominantly visceral, they are large fat cells deposited under the skin and very metabolically active. The hormones they secrete have direct access to the liver, you may have heard of the term fatty liver. -

Function and Gene Expression of Circulating Neutrophils in Dairy Cows: Impact of Micronutrient Supplementation
FUNCTION AND GENE EXPRESSION OF CIRCULATING NEUTROPHILS IN DAIRY COWS: IMPACT OF MICRONUTRIENT SUPPLEMENTATION A Dissertation Presented to The Faculty of the Graduate School At The University of Missouri In Partial Fulfillment Of the Requirements for the Degree Doctor of Philosophy By Xavier S. Revelo Dr. Matthew R. Waldron, Dissertation Supervisor July, 2012 ©Copyright by Xavier S. Revelo 2012 All rights reserved The undersigned, appointed by the dean of the Graduate School, have examined the dissertation entitled: FUNCTION AND GENE EXPRESSION OF CIRCULATING NEUTROPHILS IN DAIRY COWS: IMPACT OF MICRONUTRIENT SUPPLEMENTATION Presented by Xavier Revelo A candidate for the degree of Doctor of Philosophy in Animal Sciences And hereby certify that, in their opinion, it is worthy of acceptance. Dissertation Examination Committee: ________________________ Advisor Matthew R. Waldron, Ph.D. ________________________ Kevin L. Fritsche, Ph.D. ________________________ Matthew C. Lucy, Ph.D. ________________________ James W. Perfield, Ph.D. ACKNOWLEDGEMENTS First of all, I would like to thank my family for their patience, love and inseparable support even after all the years that I have been away from home. Thanks to my mother Sonia for dedicating her life to the guidance, inspiration, and nurturance of our family. I have been blessed with a loving and devoted family who gave me the motivation I needed to pursue my professional goals. I would also like to offer my sincerest gratitude to the friends I made while pursuing my doctorate degree at the University of Missouri. Special thanks to Daniel Mathew, Brad Scharf, Ky Pohler, Eric Coate, and Emma Jinks for sharing their time and friendship. -
A Flexible Microfluidic System for Single-Cell Transcriptome Profiling
www.nature.com/scientificreports OPEN A fexible microfuidic system for single‑cell transcriptome profling elucidates phased transcriptional regulators of cell cycle Karen Davey1,7, Daniel Wong2,7, Filip Konopacki2, Eugene Kwa1, Tony Ly3, Heike Fiegler2 & Christopher R. Sibley 1,4,5,6* Single cell transcriptome profling has emerged as a breakthrough technology for the high‑resolution understanding of complex cellular systems. Here we report a fexible, cost‑efective and user‑ friendly droplet‑based microfuidics system, called the Nadia Instrument, that can allow 3′ mRNA capture of ~ 50,000 single cells or individual nuclei in a single run. The precise pressure‑based system demonstrates highly reproducible droplet size, low doublet rates and high mRNA capture efciencies that compare favorably in the feld. Moreover, when combined with the Nadia Innovate, the system can be transformed into an adaptable setup that enables use of diferent bufers and barcoded bead confgurations to facilitate diverse applications. Finally, by 3′ mRNA profling asynchronous human and mouse cells at diferent phases of the cell cycle, we demonstrate the system’s ability to readily distinguish distinct cell populations and infer underlying transcriptional regulatory networks. Notably this provided supportive evidence for multiple transcription factors that had little or no known link to the cell cycle (e.g. DRAP1, ZKSCAN1 and CEBPZ). In summary, the Nadia platform represents a promising and fexible technology for future transcriptomic studies, and other related applications, at cell resolution. Single cell transcriptome profling has recently emerged as a breakthrough technology for understanding how cellular heterogeneity contributes to complex biological systems. Indeed, cultured cells, microorganisms, biopsies, blood and other tissues can be rapidly profled for quantifcation of gene expression at cell resolution. -
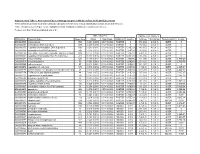
Association of Gene Ontology Categories with Decay Rate for Hepg2 Experiments These Tables Show Details for All Gene Ontology Categories
Supplementary Table 1: Association of Gene Ontology Categories with Decay Rate for HepG2 Experiments These tables show details for all Gene Ontology categories. Inferences for manual classification scheme shown at the bottom. Those categories used in Figure 1A are highlighted in bold. Standard Deviations are shown in parentheses. P-values less than 1E-20 are indicated with a "0". Rate r (hour^-1) Half-life < 2hr. Decay % GO Number Category Name Probe Sets Group Non-Group Distribution p-value In-Group Non-Group Representation p-value GO:0006350 transcription 1523 0.221 (0.009) 0.127 (0.002) FASTER 0 13.1 (0.4) 4.5 (0.1) OVER 0 GO:0006351 transcription, DNA-dependent 1498 0.220 (0.009) 0.127 (0.002) FASTER 0 13.0 (0.4) 4.5 (0.1) OVER 0 GO:0006355 regulation of transcription, DNA-dependent 1163 0.230 (0.011) 0.128 (0.002) FASTER 5.00E-21 14.2 (0.5) 4.6 (0.1) OVER 0 GO:0006366 transcription from Pol II promoter 845 0.225 (0.012) 0.130 (0.002) FASTER 1.88E-14 13.0 (0.5) 4.8 (0.1) OVER 0 GO:0006139 nucleobase, nucleoside, nucleotide and nucleic acid metabolism3004 0.173 (0.006) 0.127 (0.002) FASTER 1.28E-12 8.4 (0.2) 4.5 (0.1) OVER 0 GO:0006357 regulation of transcription from Pol II promoter 487 0.231 (0.016) 0.132 (0.002) FASTER 6.05E-10 13.5 (0.6) 4.9 (0.1) OVER 0 GO:0008283 cell proliferation 625 0.189 (0.014) 0.132 (0.002) FASTER 1.95E-05 10.1 (0.6) 5.0 (0.1) OVER 1.50E-20 GO:0006513 monoubiquitination 36 0.305 (0.049) 0.134 (0.002) FASTER 2.69E-04 25.4 (4.4) 5.1 (0.1) OVER 2.04E-06 GO:0007050 cell cycle arrest 57 0.311 (0.054) 0.133 (0.002) -

Body Fat Distribution As a Risk Factor for Osteoporosis
SAMJ I ARTICLES In the past, most epidemiological studies that examined Body fat distribution as a the association between obesity and disease considered only total adipose tissue and ignored its distribution. risk factor for osteoporosis Recently it has become apparent that it is not obesity per se, but the regional distribution of adipose tissue, that Renee Blaauw, Eisa C. Albertse, Stephen Hough correlates with many obesity-related morbidities including atherosclerosis, hypertension, hyperlipidaemias and 4 diabetes mellitus. -8 Objective. The aim of this study was to compare the body The anatomical distribution of adipose tissue differs fat distribution of patients with osteoporosis (GP) with that between men and women in both normal and obese of an appropriately matched non-GP control group. individuals, suggesting that sex hormones are involved in Design. Case control study. the regulation of adipose tissue metabolism.5--10 Upper body Setting. Department of Endocrinology and Metabolism, (android or waist) obesity, which is typically observed in men, is associated with hyperandrogenism, whereas lower Tygerberg Hospital. body (gynoid or hip) obesity is far more common in women, Participants. A total of 56 patients with histologicatly suggesting an oestrogenic influence.':>-12 Moreover, upper proven idiopathic GP, of whom 39 were women (mean age body obesity has been shown to be associated with 61 ± 11 years) and 17 men (49 ± 15 years), were compared hypercortisolism and classically occurs in patients with with 125 age- and sex-matched non-OP (confirmed by Cushing's syndrome. 13 Since hypogonadism and dual energy X-ray absorptiometry) subjects, 98 women hypercortisolaemia are well-known causes of GP, we questioned whether this disease was also associated with (60 ± 11 years) and 27 men (51 ± 16 years). -

HHS Public Access Author Manuscript
HHS Public Access Author manuscript Author Manuscript Author ManuscriptNature. Author ManuscriptAuthor manuscript; Author Manuscript available in PMC 2015 June 11. Published in final edited form as: Nature. 2014 December 11; 516(7530): 242–245. doi:10.1038/nature13760. An evolutionary arms race between KRAB zinc finger genes 91/93 and SVA/L1 retrotransposons Frank MJ Jacobs1,§,*, David Greenberg1,2,¶,*, Ngan Nguyen1,3, Maximilian Haeussler1, Adam D Ewing1,¥, Sol Katzman1, Benedict Paten1, Sofie R Salama1,4, and David Haussler1,4,# 1Center for Biomolecular Science and Engineering, University of California Santa Cruz, Santa Cruz, California, United States of America 2Molecular, Cell and Developmental Biology, of California Santa Cruz, Santa Cruz, California, United States of America 3Biomolecular Engineering, University of California Santa Cruz, Santa Cruz, California, United States of America 4Howard Hughes Medical Institute, University of California Santa Cruz, Santa Cruz, California, United States of America Summary Throughout evolution, primate genomes have been modified by waves of retrotransposon insertions1,2,3. For each wave, the host eventually finds a way to repress retrotransposon transcription and prevent further insertions. In mouse embryonic stem cells (mESCs), transcriptional silencing of retrotransposons requires TRIM28 (KAP1) and it’s repressive complex, which can be recruited to target sites by KRAB zinc finger proteins such as murine- specific ZFP809 which binds to integrated murine leukemia virus DNA elements and recruits -

A Large-Scale Genome-Wide Interaction Study Llida Barata Washington University School of Medicine in St
Washington University School of Medicine Digital Commons@Becker Open Access Publications 2015 The influence of age and sex on genetic associations with adult body size and shape: A large-scale genome-wide interaction study Llida Barata Washington University School of Medicine in St. Louis Mary F. Feitosa Washington University School of Medicine in St. Louis Jacek Czajkowski Washington University School of Medicine in St. Louis Jeannette Simino Washington University School of Medicine in St. Louis Pamela A. F. Madden Washington University School of Medicine in St. Louis See next page for additional authors Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Recommended Citation Barata, Llida; Feitosa, Mary F.; Czajkowski, Jacek; Simino, Jeannette; Madden, Pamela A. F.; Sung, Yun Ju; Heath, Andrew C.; Rice, Treva K.; Rao, D. C.; and et al., ,"The influence of age and sex on genetic associations with adult body size and shape: A large-scale genome-wide interaction study." PLoS Genetics.11,10. e1005378. (2015). https://digitalcommons.wustl.edu/open_access_pubs/4605 This Open Access Publication is brought to you for free and open access by Digital Commons@Becker. It has been accepted for inclusion in Open Access Publications by an authorized administrator of Digital Commons@Becker. For more information, please contact [email protected]. Authors Llida Barata, Mary F. Feitosa, Jacek Czajkowski, Jeannette Simino, Pamela A. F. Madden, Yun Ju Sung, Andrew C. Heath, Treva K. Rice, D. C. Rao, and et al. This open access publication is available at Digital Commons@Becker: https://digitalcommons.wustl.edu/open_access_pubs/4605 RESEARCH ARTICLE The Influence of Age and Sex on Genetic Associations with Adult Body Size and Shape: A Large-Scale Genome-Wide Interaction Study Thomas W. -

The Function and Evolution of C2H2 Zinc Finger Proteins and Transposons
The function and evolution of C2H2 zinc finger proteins and transposons by Laura Francesca Campitelli A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy Department of Molecular Genetics University of Toronto © Copyright by Laura Francesca Campitelli 2020 The function and evolution of C2H2 zinc finger proteins and transposons Laura Francesca Campitelli Doctor of Philosophy Department of Molecular Genetics University of Toronto 2020 Abstract Transcription factors (TFs) confer specificity to transcriptional regulation by binding specific DNA sequences and ultimately affecting the ability of RNA polymerase to transcribe a locus. The C2H2 zinc finger proteins (C2H2 ZFPs) are a TF class with the unique ability to diversify their DNA-binding specificities in a short evolutionary time. C2H2 ZFPs comprise the largest class of TFs in Mammalian genomes, including nearly half of all Human TFs (747/1,639). Positive selection on the DNA-binding specificities of C2H2 ZFPs is explained by an evolutionary arms race with endogenous retroelements (EREs; copy-and-paste transposable elements), where the C2H2 ZFPs containing a KRAB repressor domain (KZFPs; 344/747 Human C2H2 ZFPs) are thought to diversify to bind new EREs and repress deleterious transposition events. However, evidence of the gain and loss of KZFP binding sites on the ERE sequence is sparse due to poor resolution of ERE sequence evolution, despite the recent publication of binding preferences for 242/344 Human KZFPs. The goal of my doctoral work has been to characterize the Human C2H2 ZFPs, with specific interest in their evolutionary history, functional diversity, and coevolution with LINE EREs. -

N22252 Natazia Clinical PREA
CLINICAL REVIEW Application Type NDA Application Number 22-252 Priority or Standard Standard Submit Date July 6, 2009 PDUFA Goal Date May 6, 2010 Division / Office Division of Reproductive and Urologic Products (DRUP) / Office of Drug Evaluation III (ODE III) Reviewer Name Gerald Willett M.D. Review Completion Date April 28, 2010 Established Name Estradiol valerate / Dienogest (EV/DNG) Trade Name To be determined Therapeutic Class Combination oral contraceptive Applicant Bayer HealthCare Pharmaceuticals Inc. Formulation Oral tablets Dosing Regimen - Days 1-2 (3.0 mg EV) Cycle Days (dose) Days 3-7 (2.0 mg EV + 2.0 mg DNG) Days 8-24 (2.0 mg EV + 3.0 mg DNG) Days 25-26 (1.0 mg EV) Days 27-28 (placebo) Indication Contraception (primary) Heavy and/or prolonged menstrual bleeding (secondary) Intended Population Women of childbearing age Clinical Review Gerald Willett, M.D. NDA 22-252 (EV/DNG) Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT....................................... 11 1.1 Recommendation on Regulatory Action ........................................................... 11 1.2 Risk Benefit Assessment.................................................................................. 11 1.3 Recommendations for Postmarket Risk Evaluation and Mitigation Strategies... 14 1.4 Recommendations for Postmarket Requirements and Commitments .............. 14 2 INTRODUCTION AND REGULATORY BACKGROUND ...................................... 15 2.1 Product Information ......................................................................................... -

Editor's Pick
EDITOR’S PICK In women of reproductive age, polycystic ovary syndrome (PCOS) is one of the most common abnormalities, and obesity is observed in about 80% of these patients. The relationship between PCOS and obesity is complex, and therefore the study “Selection of Appropriate Tools for Evaluating Obesity in Polycystic Ovary Syndrome Patients” is very welcome. The author concludes that using BMI to diagnose and classify obesity, a high fat content, or fat distribution of android type in PCOS patients with normal weight can be overlooked. Prof Joep Geraedts SELECTION OF APPROPRIATE TOOLS FOR EVALUATING OBESITY IN POLYCYSTIC OVARY SYNDROME PATIENTS *Yang Xu Reproductive and Genetic Medical Center, Peking University First Hospital; OB/GYN Department, Peking University First Hospital, Beijing, China *Correspondence to [email protected] Disclosure: The author has declared no conflicts of interest. Received: 02.05.17 Accepted: 06.07.17 Citation: EMJ Repro Health. 2017;3[1]:48-52. ABSTRACT Patients with polycystic ovary syndrome (PCOS) have unique endocrine and metabolic characteristics, whereby the incidence and potentiality of obesity, as well as the accompanying risk of metabolic and cardiovascular diseases, are significantly increased. Currently, BMI is widely used to diagnose and classify obesity. However, body fat is not accounted for in BMI calculations, and the missed diagnosis rate of obesity is nearly 50%. Since PCOS patients with normal weight are also characterised by a high content of fat or fat distribution of android type, some of these patients are often overlooked if an inappropriate diagnostic tool for obesity is selected, which affects the therapeutic effect. Herein, we have reviewed the mechanism and diagnostic methods of PCOS-related obesity and suggested that not only body weight and circumference alone, but also the body fat percentage and fat distribution, should be considered for the evaluation of obesity in PCOS patients. -

Effective Measures of Weight Gain Five Years Post-Kidney Transplantation
University of Tennessee Health Science Center UTHSC Digital Commons Theses and Dissertations (ETD) College of Graduate Health Sciences 12-2018 Effective Measures of Weight Gain Five Years Post- Kidney Transplantation Tara Calico Cherry University of Tennessee Health Science Center Follow this and additional works at: https://dc.uthsc.edu/dissertations Part of the Cardiovascular Diseases Commons, Endocrine System Diseases Commons, Investigative Techniques Commons, Nutritional and Metabolic Diseases Commons, Other Analytical, Diagnostic and Therapeutic Techniques and Equipment Commons, and the Other Nursing Commons Recommended Citation Cherry, Tara Calico (http://orcid.org/ https://orcid.org/0000-0002-2069-1836), "Effective Measures of Weight Gain Five Years Post- Kidney Transplantation" (2018). Theses and Dissertations (ETD). Paper 468. http://dx.doi.org/10.21007/etd.cghs.2018.0471. This Dissertation is brought to you for free and open access by the College of Graduate Health Sciences at UTHSC Digital Commons. It has been accepted for inclusion in Theses and Dissertations (ETD) by an authorized administrator of UTHSC Digital Commons. For more information, please contact [email protected]. Effective Measures of Weight Gain Five Years Post-Kidney Transplantation Document Type Dissertation Degree Name Doctor of Philosophy (PhD) Program Nursing Science Research Advisor Donna K. Hathaway Ph.D Committee Carolyn J. Graff, Ph.D. Carrie Harvey, Ph.D. Tara O’Brien, Ph.D. George E. Relyea, MS ORCID http://orcid.org/ https://orcid.org/0000-0002-2069-1836 DOI 10.21007/etd.cghs.2018.0471 This dissertation is available at UTHSC Digital Commons: https://dc.uthsc.edu/dissertations/468 Effective Measures of Weight Gain Five Years Post-Kidney Transplantation A Dissertation Presented for The Graduate Studies Council The University of Tennessee Health Science Center In Partial Fulfillment Of the Requirements for the Degree Doctor of Philosophy From The University of Tennessee By Tara Calico Cherry December 2018 Copyright © 2018 by Tara Calico Cherry.