Specific Secondary Genetic Alterations in Mantle Cell
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Title of the Article
Mechanism-Anchored Profiling Derived from Epigenetic Networks Predicts Outcome in Acute Lymphoblastic Leukemia Xinan Yang, PhD1, Yong Huang, MD1, James L Chen, MD1, Jianming Xie, MSc2, Xiao Sun, PhD2, Yves A Lussier, MD1,3,4§ 1Center for Biomedical Informatics and Section of Genetic Medicine, Department of Medicine, The University of Chicago, Chicago, IL 60637 USA 2State Key Laboratory of Bioelectronics, Southeast University, 210096 Nanjing, P.R.China 3The University of Chicago Cancer Research Center, and The Ludwig Center for Metastasis Research, The University of Chicago, Chicago, IL 60637 USA 4The Institute for Genomics and Systems Biology, and the Computational Institute, The University of Chicago, Chicago, IL 60637 USA §Corresponding author Email addresses: XY: [email protected] YH: [email protected] JC: [email protected] JX: [email protected] XS: [email protected] YL: [email protected] - 1 - Abstract Background Current outcome predictors based on “molecular profiling” rely on gene lists selected without consideration for their molecular mechanisms. This study was designed to demonstrate that we could learn about genes related to a specific mechanism and further use this knowledge to predict outcome in patients – a paradigm shift towards accurate “mechanism-anchored profiling”. We propose a novel algorithm, PGnet, which predicts a tripartite mechanism-anchored network associated to epigenetic regulation consisting of phenotypes, genes and mechanisms. Genes termed as GEMs in this network meet all of the following criteria: (i) they are co-expressed with genes known to be involved in the biological mechanism of interest, (ii) they are also differentially expressed between distinct phenotypes relevant to the study, and (iii) as a biomodule, genes correlate with both the mechanism and the phenotype. -

Download The
PROBING THE INTERACTION OF ASPERGILLUS FUMIGATUS CONIDIA AND HUMAN AIRWAY EPITHELIAL CELLS BY TRANSCRIPTIONAL PROFILING IN BOTH SPECIES by POL GOMEZ B.Sc., The University of British Columbia, 2002 A THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE in THE FACULTY OF GRADUATE STUDIES (Experimental Medicine) THE UNIVERSITY OF BRITISH COLUMBIA (Vancouver) January 2010 © Pol Gomez, 2010 ABSTRACT The cells of the airway epithelium play critical roles in host defense to inhaled irritants, and in asthma pathogenesis. These cells are constantly exposed to environmental factors, including the conidia of the ubiquitous mould Aspergillus fumigatus, which are small enough to reach the alveoli. A. fumigatus is associated with a spectrum of diseases ranging from asthma and allergic bronchopulmonary aspergillosis to aspergilloma and invasive aspergillosis. Airway epithelial cells have been shown to internalize A. fumigatus conidia in vitro, but the implications of this process for pathogenesis remain unclear. We have developed a cell culture model for this interaction using the human bronchial epithelium cell line 16HBE and a transgenic A. fumigatus strain expressing green fluorescent protein (GFP). Immunofluorescent staining and nystatin protection assays indicated that cells internalized upwards of 50% of bound conidia. Using fluorescence-activated cell sorting (FACS), cells directly interacting with conidia and cells not associated with any conidia were sorted into separate samples, with an overall accuracy of 75%. Genome-wide transcriptional profiling using microarrays revealed significant responses of 16HBE cells and conidia to each other. Significant changes in gene expression were identified between cells and conidia incubated alone versus together, as well as between GFP positive and negative sorted cells. -

Knowledge Management Enviroments for High Throughput Biology
Knowledge Management Enviroments for High Throughput Biology Abhey Shah A Thesis submitted for the degree of MPhil Biology Department University of York September 2007 Abstract With the growing complexity and scale of data sets in computational biology and chemoin- formatics, there is a need for novel knowledge processing tools and platforms. This thesis describes a newly developed knowledge processing platform that is different in its emphasis on architecture, flexibility, builtin facilities for datamining and easy cross platform usage. There exist thousands of bioinformatics and chemoinformatics databases, that are stored in many different forms with different access methods, this is a reflection of the range of data structures that make up complex biological and chemical data. Starting from a theoretical ba- sis, FCA (Formal Concept Analysis) an applied branch of lattice theory, is used in this thesis to develop a file system that automatically structures itself by it’s contents. The procedure of extracting concepts from data sets is examined. The system also finds appropriate labels for the discovered concepts by extracting data from ontological databases. A novel method for scaling non-binary data for use with the system is developed. Finally the future of integrative systems biology is discussed in the context of efficiently closed causal systems. Contents 1 Motivations and goals of the thesis 11 1.1 Conceptual frameworks . 11 1.2 Biological foundations . 12 1.2.1 Gene expression data . 13 1.2.2 Ontology . 14 1.3 Knowledge based computational environments . 15 1.3.1 Interfaces . 16 1.3.2 Databases and the character of biological data . -

Literature Mining Sustains and Enhances Knowledge Discovery from Omic Studies
LITERATURE MINING SUSTAINS AND ENHANCES KNOWLEDGE DISCOVERY FROM OMIC STUDIES by Rick Matthew Jordan B.S. Biology, University of Pittsburgh, 1996 M.S. Molecular Biology/Biotechnology, East Carolina University, 2001 M.S. Biomedical Informatics, University of Pittsburgh, 2005 Submitted to the Graduate Faculty of School of Medicine in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Pittsburgh 2016 UNIVERSITY OF PITTSBURGH SCHOOL OF MEDICINE This dissertation was presented by Rick Matthew Jordan It was defended on December 2, 2015 and approved by Shyam Visweswaran, M.D., Ph.D., Associate Professor Rebecca Jacobson, M.D., M.S., Professor Songjian Lu, Ph.D., Assistant Professor Dissertation Advisor: Vanathi Gopalakrishnan, Ph.D., Associate Professor ii Copyright © by Rick Matthew Jordan 2016 iii LITERATURE MINING SUSTAINS AND ENHANCES KNOWLEDGE DISCOVERY FROM OMIC STUDIES Rick Matthew Jordan, M.S. University of Pittsburgh, 2016 Genomic, proteomic and other experimentally generated data from studies of biological systems aiming to discover disease biomarkers are currently analyzed without sufficient supporting evidence from the literature due to complexities associated with automated processing. Extracting prior knowledge about markers associated with biological sample types and disease states from the literature is tedious, and little research has been performed to understand how to use this knowledge to inform the generation of classification models from ‘omic’ data. Using pathway analysis methods to better understand the underlying biology of complex diseases such as breast and lung cancers is state-of-the-art. However, the problem of how to combine literature- mining evidence with pathway analysis evidence is an open problem in biomedical informatics research. -

Table S4. Trophoblast Differentiation-Associated Genes
Table S4. Trophoblast differentiation-associated genes Gene Stem Chromosomal Affymetrix ID Gene Title Symbol Ave Dif Ave GenBank Location dif/ stem t-test 1390511_at LOC308394 Cgm4 10 1863 BI285801 1 193.51 0.006 1378534_at similar to brain carcinoembryonic antigen LOC308394 10 1746 NM_001025679 1q21 183.10 0.001 1388433_at keratin complex 1, acidic, gene 19 Krt1-19 53 7958 NM_199498 10q32.1 149.07 0.022 1369029_at phospholipid scramblase 1 Plscr1 20 2050 NM_057194 8q31 101.12 0.028 1389856_at carcinoembryonic antigen gene family 4 Cgm4 57 5073 NM_012525 1q21 89.73 0.001 carcinoembryonic antigen-related cell 1368996_at adhesion molecule 3 Ceacam3 202 17879 NM_012702 1q21 88.71 0.001 1392832_at similar to angiopoietin-like 1 LOC684489 17 1398 XM_001068284 --- 83.66 0.001 1377666_at choline dehydrogenase Chdh 26 1571 NM_198731 16p16 60.59 0.003 cytochrome P450, family 11, subfamily a, 1368468_at polypeptide 1 Cyp11a1 196 9216 NM_017286 8q24 47.11 0.000 1376934_x_at similar to brain carcinoembryonic antigen Cgm4 53 2146 BI285801 1 40.22 0.000 stimulated by retinoic acid gene 6 homolog 1390525_a_at (mouse) Stra6 28 1037 NM_001029924 8q24 37.44 0.001 1382690_at carcinoembryonic antigen gene family 4 Cgm4 81 2729 NM_012525 1q21 33.86 0.001 1367809_at prolactin family 4, subfamily a, member 1 Prl4a1 683 22573 NM_017036 17p11 33.05 0.004 calcium channel, voltage-dependent, L type, 1383458_at alpha 1D subunit Cacna1d 26 802 BF403759 16 30.89 0.001 1370852_at spleen protein 1 precursor LOC171573 692 20968 NM_138537 8q21 30.29 0.003 1376036_at transporter -

Role and Regulation of the P53-Homolog P73 in the Transformation of Normal Human Fibroblasts
Role and regulation of the p53-homolog p73 in the transformation of normal human fibroblasts Dissertation zur Erlangung des naturwissenschaftlichen Doktorgrades der Bayerischen Julius-Maximilians-Universität Würzburg vorgelegt von Lars Hofmann aus Aschaffenburg Würzburg 2007 Eingereicht am Mitglieder der Promotionskommission: Vorsitzender: Prof. Dr. Dr. Martin J. Müller Gutachter: Prof. Dr. Michael P. Schön Gutachter : Prof. Dr. Georg Krohne Tag des Promotionskolloquiums: Doktorurkunde ausgehändigt am Erklärung Hiermit erkläre ich, dass ich die vorliegende Arbeit selbständig angefertigt und keine anderen als die angegebenen Hilfsmittel und Quellen verwendet habe. Diese Arbeit wurde weder in gleicher noch in ähnlicher Form in einem anderen Prüfungsverfahren vorgelegt. Ich habe früher, außer den mit dem Zulassungsgesuch urkundlichen Graden, keine weiteren akademischen Grade erworben und zu erwerben gesucht. Würzburg, Lars Hofmann Content SUMMARY ................................................................................................................ IV ZUSAMMENFASSUNG ............................................................................................. V 1. INTRODUCTION ................................................................................................. 1 1.1. Molecular basics of cancer .......................................................................................... 1 1.2. Early research on tumorigenesis ................................................................................. 3 1.3. Developing -

Identification of a Novel Deletion Region in 3Q29 Microdeletion Syndrome by Oligonucleotide Array Comparative Genomic Hybridization
Korean J Lab Med 2010;30:70-5 � Original Article∙Diagnostic Genetics � DOI 10.3343/kjlm.2010.30.1.70 Identification of a Novel Deletion Region in 3q29 Microdeletion Syndrome by Oligonucleotide Array Comparative Genomic Hybridization Eul-Ju Seo, M.D.1, Kyung Ran Jun, M.D.1, Han-Wook Yoo, M.D.2, Hanik K. Yoo, M.D.3, and Jin-Ok Lee, M.S.4 Departments of Laboratory Medicine1, Pediatrics2, and Psychiatry3, University of Ulsan College of Medicine and Asan Medical Center, Seoul; Asan Institute for Life Sciences4, Seoul, Korea Background : The 3q29 microdeletion syndrome is a genomic disorder characterized by mental retardation, developmental delay, microcephaly, and slight facial dysmorphism. In most cases, the microdeletion spans a 1.6-Mb region between low-copy repeats (LCRs). We identified a novel 4.0- Mb deletion using oligonucleotide array comparative genomic hybridization (array CGH) in monozy- gotic twin sisters. Methods : G-banded chromosome analysis was performed in the twins and their parents. High- resolution oligonucleotide array CGH was performed using the human whole genome 244K CGH microarray (Agilent Technologies, USA) followed by validation using FISH, and the obtained results were analyzed using the genome database resources. Results : G-banding revealed that the twins had de novo 46,XX,del(3)(q29) karyotype. Array CGH showed a 4.0-Mb interstitial deletion on 3q29, which contained 39 genes and no breakpoints flanked by LCRs. In addition to the typical characteristics of the 3q29 microdeletion syndrome, the twins had attention deficit-hyperactivity disorder, strabismus, congenital heart defect, and gray hair. Besides the p21-activated protein kinase (PAK2) and discs large homolog 1 (DLG1) genes, which are known to play a critical role in mental retardation, the hairy and enhancer of split 1 (HES1) and antigen p97 (melanoma associated; MFI2) genes might be possible candidate genes associated with strabis- mus, congenital heart defect, and gray hair. -

1 Novel Expression Signatures Identified by Transcriptional Analysis
ARD Online First, published on October 7, 2009 as 10.1136/ard.2009.108043 Ann Rheum Dis: first published as 10.1136/ard.2009.108043 on 7 October 2009. Downloaded from Novel expression signatures identified by transcriptional analysis of separated leukocyte subsets in SLE and vasculitis 1Paul A Lyons, 1Eoin F McKinney, 1Tim F Rayner, 1Alexander Hatton, 1Hayley B Woffendin, 1Maria Koukoulaki, 2Thomas C Freeman, 1David RW Jayne, 1Afzal N Chaudhry, and 1Kenneth GC Smith. 1Cambridge Institute for Medical Research and Department of Medicine, Addenbrooke’s Hospital, Hills Road, Cambridge, CB2 0XY, UK 2Roslin Institute, University of Edinburgh, Roslin, Midlothian, EH25 9PS, UK Correspondence should be addressed to Dr Paul Lyons or Prof Kenneth Smith, Department of Medicine, Cambridge Institute for Medical Research, Addenbrooke’s Hospital, Hills Road, Cambridge, CB2 0XY, UK. Telephone: +44 1223 762642, Fax: +44 1223 762640, E-mail: [email protected] or [email protected] Key words: Gene expression, autoimmune disease, SLE, vasculitis Word count: 2,906 The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non-exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article (if accepted) to be published in Annals of the Rheumatic Diseases and any other BMJPGL products to exploit all subsidiary rights, as set out in their licence (http://ard.bmj.com/ifora/licence.pdf). http://ard.bmj.com/ on September 29, 2021 by guest. Protected copyright. 1 Copyright Article author (or their employer) 2009. -

Table S3a Table
Table S3a C2 KEGG Geneset Genesets enriched and upregulated in responders (FDR <0.25) Genesets enriched and upregulated in non-responders (FDR <0.25) HSA04610_COMPLEMENT_AND_COAGULATION_CASCADES HSA00970_AMINOACYL_TRNA_BIOSYNTHESIS HSA04640_HEMATOPOIETIC_CELL_LINEAGE HSA05050_DENTATORUBROPALLIDOLUYSIAN_ATROPHY HSA04060_CYTOKINE_CYTOKINE_RECEPTOR_INTERACTION HSA04514_CELL_ADHESION_MOLECULES HSA04650_NATURAL_KILLER_CELL_MEDIATED_CYTOTOXICITY HSA04630_JAK_STAT_SIGNALING_PATHWAY HSA03320_PPAR_SIGNALING_PATHWAY HSA04080_NEUROACTIVE_LIGAND_RECEPTOR_INTERACTION HSA00980_METABOLISM_OF_XENOBIOTICS_BY_CYTOCHROME_P450 HSA00071_FATTY_ACID_METABOLISM HSA04660_T_CELL_RECEPTOR_SIGNALING_PATHWAY HSA04612_ANTIGEN_PROCESSING_AND_PRESENTATION HSA04662_B_CELL_RECEPTOR_SIGNALING_PATHWAY HSA04920_ADIPOCYTOKINE_SIGNALING_PATHWAY HSA00120_BILE_ACID_BIOSYNTHESIS HSA04670_LEUKOCYTE_TRANSENDOTHELIAL_MIGRATION HSA00641_3_CHLOROACRYLIC_ACID_DEGRADATION HSA04020_CALCIUM_SIGNALING_PATHWAY HSA04940_TYPE_I_DIABETES_MELLITUS HSA04512_ECM_RECEPTOR_INTERACTION HSA00010_GLYCOLYSIS_AND_GLUCONEOGENESIS HSA02010_ABC_TRANSPORTERS_GENERAL HSA04664_FC_EPSILON_RI_SIGNALING_PATHWAY HSA04710_CIRCADIAN_RHYTHM HSA04510_FOCAL_ADHESION HSA04810_REGULATION_OF_ACTIN_CYTOSKELETON HSA00410_BETA_ALANINE_METABOLISM HSA01040_POLYUNSATURATED_FATTY_ACID_BIOSYNTHESIS HSA00532_CHONDROITIN_SULFATE_BIOSYNTHESIS HSA04620_TOLL_LIKE_RECEPTOR_SIGNALING_PATHWAY HSA04010_MAPK_SIGNALING_PATHWAY HSA00561_GLYCEROLIPID_METABOLISM HSA00053_ASCORBATE_AND_ALDARATE_METABOLISM HSA00590_ARACHIDONIC_ACID_METABOLISM -

Epigenetic Mechanisms of Gene Regulation in Human Breast Cancer
EPIGENETIC MECHANISMS OF GENE REGULATION IN HUMAN BREAST CANCER Ashley Garrett Rivenbark A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Curriculum of Toxicology. Chapel Hill 2007 Approved by: William B. Coleman, Ph.D. Channing J. Der, Ph.D. William K. Funkhouser, M.D., Ph.D. Wendell D. Jones, Ph.D. William K. Kaufmann, Ph.D. © 2007 Ashley Garrett Rivenbark ALL RIGHTS RESERVED ii ABSTRACT Ashley Garrett Rivenbark: Epigenetic Mechanisms of Gene Regulation in Human Breast Cancer (Under the direction of William B. Coleman, Ph.D.) Breast cancer represents a significant health problem and improvements in our ability to prevent, diagnose, and treat the disease requires a greater understanding of the molecular basis of breast carcinogenesis. Epigenetic mechanisms play a major role in breast carcinogenesis, with DNA methylation accounting for most epigenetic gene silencing, affecting a number of different gene targets. However, mechanisms of DNA methylation- dependent silencing are poorly understood. To identify epigenetically-regulated genes in breast cancer, MCF-7 breast cancer cells were exposed to demethylating treatment and gene expression patterns were examined by microarray analysis. Genes with increased expression after demethylation treatment that returned to control levels after treatment withdrawal were directly assessed for DNA methylation by bisulfite sequencing. A group of 20 putative methylation-sensitive genes were identified that could be classified into three groups based upon their promoter CpG features. The majority of these methylation-sensitive genes lacked a conventional DNA methylation target (CpG island), resulting in an expanded model for epigenetic regulation of gene expression that recognizes the importance of all promoter CpGs. -
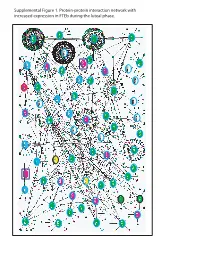
Supplemental Figure 1. Protein-Protein Interaction Network with Increased Expression in Fteb During the Luteal Phase
Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during luteal phase. LEGENDS TO SUPPLEMENTAL FIGURES Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with increased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. Genes encoding proteins shown as large ovals highlighted in blue were exclusively found in the first comparison (Manuscript Figure 2), whereas those highlighted in red were only found in the second comparison (Manuscript Figure 3). Genes encoding proteins shown as large ovals highlighted in black were found in both comparisons. The color of each node indicates the ontology of the corresponding protein as determined by the Online Predicted Human Interaction Database (OPHID) link with the NAViGaTOR software. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with decreased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. -

ARF Gtpases and Their Gefs and Gaps: Concepts and Challenges Elizabeth Sztul, University of Alabama Birmingham Pei-Wen Chen, Williams College James E
ARF GTPases and their GEFs and GAPs: concepts and challenges Elizabeth Sztul, University of Alabama Birmingham Pei-Wen Chen, Williams College James E. Casanova, University of Virginia Jacqueline Cherfils, CNRS and Ecole Normale Supérieure Paris-Saclay Joel B. Decks, University of Alberta David G. Lambright, University of Massachusetts Fang-Jen S. Lee, National Taiwan University Paul A. Randazzo, National Cancer Institute Lorraine C. Santy, Pennsylvania State University Annette Schuermann, German Institute of Human Nutrition Only first 10 authors above; see publication for full author list. Journal Title: Molecular Biology of the Cell Volume: Volume 30, Number 11 Publisher: American Society for Cell Biology | 2019-05-15, Pages 1249-1271 Type of Work: Article | Final Publisher PDF Publisher DOI: 10.1091/mbc.E18-12-0820 Permanent URL: https://pid.emory.edu/ark:/25593/v4999 Final published version: http://dx.doi.org/10.1091/mbc.E18-12-0820 Copyright information: German Institute of Human Nutrition This is an Open Access work distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License (http://creativecommons.org/licenses/by-nc-sa/3.0/). Accessed September 27, 2021 10:10 AM EDT M BoC | PERSPECTIVE ARF GTPases and their GEFs and GAPs: concepts and challenges Elizabeth Sztula,†, Pei-Wen Chenb, James E. Casanovac, Jacqueline Cherfilsd, Joel B. Dackse, David G. Lambrightf, Fang-Jen S. Leeg, Paul A. Randazzoh, Lorraine C. Santyi, Annette Schürmannj, Ilka Wilhelmij, Marielle E. Yohek, and Richard A.