Hand Hygiene Factfinder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
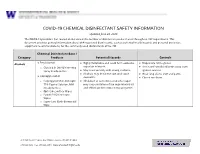
EH&S COVID-19 Chemical Disinfectant Safety Information
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -

Expert Consensus Guidelines for Stocking of Antidotes in Hospitals That Provide Emergency Care
TOXICOLOGY/CONCEPTS Expert Consensus Guidelines for Stocking of Antidotes in Hospitals That Provide Emergency Care Richard C. Dart, MD, PhD From the Rocky Mountain Poison & Drug Center - Denver Health, Denver, CO (Dart, Heard, Schaeffer, Stephen W. Borron, MD, MS Bogdan, Alhelail, Buchanan, Hoppe, Lavonas, Mlynarchek, Phua, Rhyee, Varney, Zosel); Department of E. Martin Caravati, MD, MPH Surgery, University of Texas Health Sciences Center, San Antonio, TX (Borron); Division of Emergency Daniel J. Cobaugh, PharmD Medicine, Utah Poison Control Center, University of Utah Health Sciences Center, Salt Lake City, UT Steven C. Curry, MD (Caravati); ASHP Research and Education Foundation, Bethesda, MD (Cobaugh); Department of Jay L. Falk, MD Medical Toxicology and Banner Poison Control Center, Banner Good Samaritan Medical Center, Lewis Goldfrank, MD Phoenix, AZ (Curry); Department of Emergency Medicine, Orlando Regional Medical Center, University of Susan E. Gorman, PharmD, MS Florida, Orlando, FL (Falk); New York City Poison Center; New York University School of Medicine, New Stephen Groft, PharmD York, NY (Goldfrank); Division of Strategic National Stockpile, Centers for Disease Control and Kennon Heard, MD Prevention, Atlanta, GA (Gorman); Office of Rare Diseases Research, Bethesda, MD (Groft); Division of Ken Miller, MD, PhD Emergency Medicine, School of Medicine (Dart, Heard, Lavonas, Schaeffer) and Department of Kent R. Olson, MD Pharmaceutical Sciences, School of Pharmacy (Bogdan), University of Colorado Denver, Aurora, CO; Gerald O’Malley, DO Orange County Fire Authority and Orange County Health Care Agency Emergency Medical Services, Donna Seger, MD Irvine, CA, and National Association of EMS Physicians, Lenexa, KS, (Miller); University of California, Steven A. Seifert, MD San Francisco, and San Francisco Division, California Poison Control System, San Francisco, CA Marco L. -

Reactions of Alcohols & Ethers 1
REACTIONS OF ALCOHOLS & ETHERS 1. Combustion (Extreme Oxidation) alcohol + oxygen carbon dioxide + water 2 CH3CH2OH + 6 O2 4 CO2 + 6 H2O 2. Elimination (Dehydration) ° alcohol H 2 S O 4/ 1 0 0 C alkene + water H2SO4/100 ° C CH3CH2CH2OH CH3CH=CH2 + H2O 3. Condensation ° excess alcohol H 2 S O 4 / 1 4 0 C ether + water H2SO4/140 ° C 2 CH3CH2OH CH3CH2OCH2CH3 + H2O 4. Substitution Lucas Reagent alcohol + hydrogen halide Z n C l2 alkyl halide + water ZnCl2 CH3CH2OH + HCl CH3CH2Cl + H2O • This reaction with the Lucas Reagent (ZnCl2) is a qualitative test for the different types of alcohols because the rate of the reaction differs greatly for a primary, secondary and tertiary alcohol. • The difference in rates is due to the solubility of the resulting alkyl halides • Tertiary Alcohol→ turns cloudy immediately (the alkyl halide is not soluble in water and precipitates out) • Secondary Alcohol → turns cloudy after 5 minutes • Primary Alcohol → takes much longer than 5 minutes to turn cloudy 5. Oxidation • Uses an oxidizing agent such as potassium permanganate (KMnO4) or potassium dichromate (K2Cr2O7). • This reaction can also be used as a qualitative test for the different types of alcohols because there is a distinct colour change. dichromate → chromium 3+ (orange) → (green) permanganate → manganese (IV) oxide (purple) → (brown) Tertiary Alcohol not oxidized under normal conditions CH3 KMnO4 H3C C OH NO REACTION K2Cr2O7 CH3 tertbutyl alcohol Secondary Alcohol ketone + hydrogen ions H O KMnO4 H3C C CH3 + K2Cr2O7 C + 2 H H3C CH3 OH propanone 2-propanol Primary Alcohol aldehyde + water carboxylic acid + hydrogen ions O KMnO4 O H H KMnO H H 4 + CH3CH2CH2OH C C C H C C C H + 2 H K2Cr2O7 + H2O K Cr O H H H 2 2 7 HO H H 1-propanol propanal propanoic acid 6. -

Chemical Disinfectants | Disinfection & Sterilization Guidelines | Guidelines Library | Infection Control | CDC 3/19/20, 14:52
Chemical Disinfectants | Disinfection & Sterilization Guidelines | Guidelines Library | Infection Control | CDC 3/19/20, 14:52 Infection Control Chemical Disinfectants Guideline for Disinfection and Sterilization in Healthcare Facilities (2008) Alcohol Overview. In the healthcare setting, “alcohol” refers to two water-soluble chemical compounds—ethyl alcohol and isopropyl alcohol —that have generally underrated germicidal characteristics 482. FDA has not cleared any liquid chemical sterilant or high- level disinfectant with alcohol as the main active ingredient. These alcohols are rapidly bactericidal rather than bacteriostatic against vegetative forms of bacteria; they also are tuberculocidal, fungicidal, and virucidal but do not destroy bacterial spores. Their cidal activity drops sharply when diluted below 50% concentration, and the optimum bactericidal concentration is 60%–90% solutions in water (volume/volume) 483, 484. Mode of Action. The most feasible explanation for the antimicrobial action of alcohol is denaturation of proteins. This mechanism is supported by the observation that absolute ethyl alcohol, a dehydrating agent, is less bactericidal than mixtures of alcohol and water because proteins are denatured more quickly in the presence of water 484, 485. Protein denaturation also is consistent with observations that alcohol destroys the dehydrogenases of Escherichia coli 486, and that ethyl alcohol increases the lag phase of Enterobacter aerogenes 487 and that the lag phase e!ect could be reversed by adding certain amino acids. The bacteriostatic action was believed caused by inhibition of the production of metabolites essential for rapid cell division. Microbicidal Activity. Methyl alcohol (methanol) has the weakest bactericidal action of the alcohols and thus seldom is used in healthcare 488. The bactericidal activity of various concentrations of ethyl alcohol (ethanol) was examined against a variety of microorganisms in exposure periods ranging from 10 seconds to 1 hour 483. -

Alcohols I 1400
ALCOHOLS I 1400 Table 1 MW: Table 1 CAS: Table 2 RTECS: Table 2 METHOD: 1400, Issue 2 EVALUATION: PARTIAL Issue 1: 15 February 1984 Issue 2: 15 August 1994 OSHA : Table 2 PROPERTIES: Table 1 NIOSH: Table 2 ACGIH: Table 2 COMPOUNDS AND SYNONYMS: (1) ethanol: ethyl alcohol. (2) isopropyl alcohol: 2-propanol. (3) tert-butyl alcohol: 2-methyl-2-propanol. SAMPLING MEASUREMENT SAMPLER: SOLID SORBENT TUBE TECHNIQUE: GAS CHROMATOGRAPHY, FID (coconut shell charcoal, 100 mg/50 mg) ANALYTE: compounds above FLOW RATE: 0.01 to 0.2 L/min (£0.05 L/min for ethyl alcohol) DESORPTION: 1 mL 1% 2-butanol in CS 2 (1) (2) (3) INJECTION VOL-MIN: 0.1 L 0.3 L 1.0 L VOLUME: 5 µL -MAX: 1 L 3 L 10 L TEMPERATURE-INJECTION: 200 °C SHIPMENT: cooled -DETECTOR: 250-300 °C -COLUMN: 65-70 °C SAMPLE STABILITY: unknown, store in freezer CARRIER GAS: N2 or He, 30 mL/min BLANKS: 2 to 10 field blanks per set COLUMN: glass, 2 m x 4-mm ID, 0.2% Carbowax 1500 on 60/80 Carbopack C or equivalent ACCURACY CALIBRATION: solutions of analyte in eluent (internal standard optional) RANGE STUDIED: see EVALUATION OF METHOD RANGE AND BIAS: not significant [1] PRECISION: see EVALUATION OF METHOD OVERALL PRECISION (S ˆ ): see EVALUATION OF METHOD rT ESTIMATED LOD: 0.01 mg per sample [2] ACCURACY: ± 14% APPLICABILITY: The working ranges are 16 to 1000 ppm ethanol (30 to 1900 mg/m 3) for a 1-L air sample; 4 to 400 ppm isopropyl alcohol (10 to 1000 mg/m 3) for a 3-L air sample; and 1 to 100 ppm t-butyl alcohol (3 to 300 mg/m 3) for a 10-L air sample. -

Antiseptics in the Era of Bacterial Resistance: a Focus on Povidone Iodine
Therapeutic Perspective Antiseptics in the era of bacterial resistance: a focus on povidone iodine Jean-Marie Lachapelle*1, Olivier Castel2, Alejandro Fueyo Casado3, Bernard Leroy1, Giuseppe Micali4, Dominique Tennstedt1 & Julien Lambert5 Practice Points Increasing bacterial resistance to antibiotics makes the management of superficial skin infections a major medical challenge. Antiseptics have broader spectrums of antimicrobial activity and a reduced potential for selection of bacterial resistance, relative to antibiotics. Consequently, antiseptics are appropriate alternatives to antibiotics for the prevention and treatment of superficial skin infections. Of four widely used antiseptics (povidone iodine, polihexanide, chlorhexidine and octenidine), povidone iodine has a particularly broad spectrum of antimicrobial activity that includes Gram-positive and Gram-negative bacteria, bacterial spores, fungi, protozoa and viruses. Widespread and extended use of povidone iodine is not associated with the selection of resistant bacterial strains. In contrast, bacterial resistance to chlorhexidine, quaternary ammonium salts, silver and triclosan has been documented. Regarding duration of effect on healthy skin, chlorhexidine is active for 1–4 h, whereas solutions of povidone iodine are active for 12–14 h. Aqueous and hydroalcoholic formulations of povidone iodine have good skin tolerance. Povidone iodine scrub has better skin tolerance than soap formulations of chlorhexidine and quaternary ammonium compounds (e.g., benzalkonium chloride and -

Nature the Enzyme-Substrate Com- Pounds of Catalase and Peroxides
914 NATURE June 12, 1948 Vol. 161 These are valid equivalents ; but the important point is this-the agreed figure for the last two THE ENZYME-SUBSTRATE COM whaling seasons of 16,000 'blue whale units' for the POUNDS OF CATALASE AND contracting parties may well mean that a full catch involves the killing of many more than 16,000 PEROXIDES animals. For example, in 1945-46 the Antarctic catch was returned8 as 8,304·8 'blue whale units', By BRITTON CHANCE* but was, in fact, made up of 13,381 whales (3,604 blue, 9,184 fin, 238 humpback and 81 sei whales, as well Biochemical Department, Medical Nobel Institute, Stockholm, and Molteno Institute, University of as 239 sperm whales and 35 "sperm and others"). Cambridge This last might include some bottlenose or Berardius. The catch for 1946-47 has been returned7 as 15,230·7 'blue whale units'. This represents 8,870 blue, ATALASE is a hrematin enzyme found in 12,857 fin and 2 sei whales, a total of 21,729 C relatively large concentrations in erythrocytes, whales8 • liver, kidney, etc. Its extremely efficient catalysis There is obviously a serious danger of losing sight of the destruction of hydrogen peroxide and its of the reality of the position by continued contempla ability to catalyse the oxidation of alcohols by tion of the 'blue whale unit' value of a catch, since hydrogen peroxide have been recognized for some the number of animals killed will always be greater time, but very little direct evidence for the than the number of units allowed. -

Alcohols and Phenols (Pp. 591-600)
13.9 Reactions of Alcohols: Substitution and Elimination 591 MEDICALLYSPEAKING Phenols as Antifungal Agents >ÞÊ« iÃÊ>`ÊÌ iÀÊ`iÀÛ>ÌÛiÃÊiÝ LÌÊÌ«V>Ê>ÌvÕ}>Ê«À« / iÃiÊV«Õ`Ã]Ê>ÃÊÜiÊ>ÃÊ>ÞÊÌ iÀÃ]Ê>ÀiÊÕÃi`ÊÊ iÀÌiðÊ/ iÃiÊ>}iÌÃÊ>ÀiÊLiiÛi`ÊÌÊÌiÀviÀiÊÜÌ ÊÌ iÊViÊi Ì iÊÌÀi>ÌiÌÊvÊ>Ì iÌi½ÃÊvÌ]ÊVÊÌV ]Ê >`ÊÀ}ÜÀ°Ê LÀ>iÊvÕVÌÊvÊvÕ}°Ê/ iÊvÜ}Ê>ÀiÊÕÃÌÊ>ÊviÜÊiÝ>«ið />vÌ>ÌiÊ ÃÊ Ì iÊ >VÌÛiÊ }Ài`iÌÊ Ê />VÌ/]Ê "`ÀÊ >ÌiÀÃ/]Ê>`Ê iÃiiÝ/° OH O Cl Cl I S N O Cl I N Alcohols and Phenols Cl Cl OH para-Chloro- Haloprogin Clioquinol Tolnaftate meta-xylenol Klein, D. (2012). Alcohols and Phenols. En Organic Chemistry (pp. 591- 600). USA: Wiley. 13.9 Reactions of Alcohols: Substitution and Elimination SN1 Reactions with Alcohols !SSEENIN3ECTION TERTIARYALCOHOLSWILLUNDERGOASUBSTITUTIONREACTIONWHENTREATEDWITH a hydrogen halide. OH HX X ± H2O 7ESAWTHATTHISREACTIONPROCEEDSVIAAN3N1 mechanism. Proton transfer Loss of a leaving group Nucleophilic attack H + – – + OH H Br O H2O Br Br H Recall that an SN1 mechanism has two core steps (loss of leaving group and nucleophilic attack). 7HENTHESTARTINGMATERIALISANALCOHOL WESAWTHATANADDITIONALSTEPISREQUIREDINORDERTO PROTONATETHEHYDROXYLGROUPlRST4HISREACTIONPROCEEDSVIAACARBOCATIONINTERMEDIATEANDIS therefore most appropriate for tertiary alcohols. Secondary alcohols undergo SN1 more slowly, and primary alcohols will not undergo SNATANAPPRECIABLERATE7HENDEALINGWITHAPRIMARY alcohol, an SNPATHWAYISREQUIREDINORDERTOCONVERTANALCOHOLINTOANALKYLHALIDE SN2 Reactions with Alcohols Primary and secondary alcohols will undergo substitution reactions with -

POISONS LIST APPENDIX Amoebicides: Carbarsone
POISONS LIST APPENDIX Amoebicides: Carbarsone Clioquinol and other halogenated hydroxyquinoline compounds Dehydroemetine; its salts Diloxanide; its compounds Dimetridazole Emetine Ipronidazole Metronidazole Pentamidine; its salts Ronidazole Anaesthetics: Alphadolone acetate Alphaxolone Desflurane Disoprofol Enflurane Ethyl ether Etomidate; its salts Halothane Isoflurane Ketamine; its salts Local anaesthetics, the following: their salts; their homologues and analogues; their molecular compounds Amino-alcohols esterified with benzoic acid, phenylacetic acid, phenylpropionic acid, cinnamic acid or the derivatives of these acids; their salts Benzocaine Bupivacaine Butyl aminobenzoate Cinchocaine Diperodon Etidocaine Levobupivacaine Lignocaine Mepivacaine Orthocaine Oxethazaine Phenacaine Phenodianisyl Prilocaine Ropivacaine Phencyclidine; its salts Propanidid Sevoflurane Tiletamine; its salts Tribromoethanol Analeptics and Central Stimulants: Amiphenazole; its salts Amphetamine (DD) Bemegride Cathine Cathinone (DD) Dimethoxybromoamphetamine (DOB) (DD) 2, 5-Dimethoxyamphetamine (DMA) (DD) 2, 5-Dimethoxy-4-ethylamphetamine (DOET) (DD) Ethamivan N-Ethylamphetamine; its salts N-Ethyl MDA (DD) N-Hydroxy MDA (DD) Etryptamine (DD) Fencamfamine Fenetylline Lefetamine or SPA or (-)-1-dimethylamino-1, 2-diphenylethane Leptazol Lobelia, alkaloids of Meclofenoxate; its salts Methamphetamine (DD) Methcathinone (DD) 5-Methoxy-3, 4-methylenedioxyamphetamine (MMDA) (DD) Methylenedioxyamphetamine (MDA) (DD) 3, 4-Methylenedioxymetamphetamine (MDMA) (DD) Methylphenidate; -

Version 4.1, 02/2020 SUMMARY of PRODUCT CHARACTERISTICS
Version 4.1, 02/2020 SUMMARY OF PRODUCT CHARACTERISTICS, LABELLING AND PACKAGE LEAFLET 1 SUMMARY OF PRODUCT CHARACTERISTICS 2 1. NAME OF THE MEDICINAL PRODUCT [Nationally completed name], plaster for provocation test 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Active substance microgram/cm2 microgram/patch Panel 1 1. Nickel sulphate 200 162 2. Wool alcohols 1000 810 3. Neomycin sulphate 600 486 4. Potassium dichromate 54 44 5. Caine mixa) 630 510 6. Fragrance mixb) 430 348 7. Colophony 1200 972 8. Paraben mixc) 1000 810 9. Blank patch - - 10. Balsam of Peru 800 648 11. Ethylenediamine dihydrochloride 50 41 12. Cobalt chloride 20 16 Panel 2 13. p-tert Butylphenol formaldehyde resin 45 36 14. Epoxy resin 50 41 15. Carba mixd) 250 203 16. Black rubber mixe) 75 61 17. Cl+Me-Isothiazolinone 4 3 18. Quaternium-15 100 81 19. Methyldibromoglutaronitrile 5.0 4.1 20. p-Phenylenediamine 80 65 21. Formaldehydef) 180 146 22. Mercapto mixg) 75 61 23. Thiomersal 7 6 24. Thiuram mixh) 27 22 Panel 3 25. Diazolidinyl urea 550 450 26. Quinoline mixi) 190 154 27. Tixocortol-21-pivalate 3.0 2.4 28. Gold sodium thiosulfate 75 61 29. Imidazolidinyl urea 600 490 30. Budesonide 1.0 0.81 31. Hydrocortisone-17-butyrate 20 16 32. Mercaptobenzothiazole 75 61 33. Bacitracin 600 490 3 34. Parthenolide 3.0 2.4 35. Disperse blue 106 50 41 36. 2-bromo-2-nitropropane-1,3-diol 250 200 a) Five parts of benzocaine, one part of cinchocaine hydrochloride and tetracaine hydrochloride. b) Five parts of geraniol and oak moss, four parts of hydroxycitronellal and cinnamylalcohol, two parts of cinnamaldehyde and eugenol and one part of isoeugenol and α-amylcinnamaldehyde. -

(12) Patent Application Publication (10) Pub. No.: US 2016/0319266A1 Kolkman Et Al
US 201603 19266A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2016/0319266A1 Kolkman et al. (43) Pub. Date: Nov. 3, 2016 (54) SERINE PROTEASES OF THE BACILLUS Related U.S. Application Data GIBSONI-CLADE (60) Provisional application No. 61/915,737, filed on Dec. (71) Applicant: DANISCO US INC., Palo Alto, CA 13, 2013, provisional application No. 62/069,200, (US) filed on Oct. 27, 2014. (72) Inventors: Marc Kolkman, Oegstgeest (NL); Rie Publication Classification Mejldal, Ostbirk (DK); Frits Goedegebuur, Vlaardingen (NL); Lilia (51) Int. Cl. Maria Babe, Emerald Hills, CA (US); CI2N 9/54 (2006.01) Anja Hemmingsen Kellett-Smith, A47L I3/00 (2006.01) Arhuc (DK); Harm Mulder. Oegstgeest CLID 3/386 (2006.01) (NL); Richard R. Bott, Burlingame, (52) U.S. Cl. CA (US); Miles Christopher Scotcher, CPC ............... CI2N 9/54 (2013.01): CI2Y 304/21 Hayward, CA (US) (2013.01): CIID 3/386 (2013.01); A47L (73) Assignee: Danisco US Inc., Palo Alto, CA (US) 15/0002 (2013.01); A47L 2601/20 (2013.01) (21) Appl. No.: 15/104,219 (57) ABSTRACT (22) PCT Filed: Dec. 12, 2014 The present disclosure relates to serine proteases cloned from Bacillus gibsonii, and variants thereof. Compositions (86). PCT No.: PCT/US1.4/70 107 containing the serine proteases are Suitable for use in clean 371 C)(1),1 1nging fabriTabr1cS andd hardnard SurTaces,Surf as wellll as i1n a Var1elyiety ofo (2) Date: Jun. 13, 2016 industrial applications. Patent Application Publication Nov. 3, 2016 Sheet 1 of 18 US 2016/0319266 A1 eft - iambda apfs promoter region signai peptide apt Tet R. -

Oxidation of Organic Compounds with Peroxides Catalyzed by Polynuclear Metal Compounds
catalysts Review Oxidation of Organic Compounds with Peroxides Catalyzed by Polynuclear Metal Compounds Georgiy B. Shul’pin 1,* and Lidia S. Shul’pina 2 1 Federal Research Center for Chemical Physics, N.N. Semenov Russian Academy of Sciences, Ulitsa Kosygina 4, 119991 Moscow, Russia 2 A.N. Nesmeyanov Institute of Organoelement Compounds, Russian Academy of Sciences, Ulitsa Vavilova 28, 119991 Moscow, Russia; [email protected] * Correspondence: [email protected] or [email protected]; Tel.: +7-916-384-7912 Abstract: The review describes articles that provide data on the synthesis and study of the proper- ties of catalysts for the oxidation of alkanes, olefins, and alcohols. These catalysts are polynuclear complexes of iron, copper, osmium, nickel, manganese, cobalt, vanadium. Such complexes for exam- 1 ple are: [Fe2(HPTB)(m-OH)(NO3)2](NO3)2·CH3OH·2H2O, where HPTB- 4 N,N,N0,N0-tetrakis(2- benzimidazolylmethyl)-2-hydroxo-1,3-diaminopropane; complex [(PhSiO1,5)6]2[CuO]4[NaO0.5]4 [dppmO2]2, where dppm-1,1-bis(diphenylphosphino)methane; (2,3-η-1,4- diphenylbut-2-en-1,4- dione)undecacarbonyl triangulotriosmium; phenylsilsesquioxane [(PhSiO1.5)10(CoO)5(NaOH)]; bi- 2 3 and tri-nuclear oxidovanadium(V) complexes [{VO(OEt)(EtOH)}2(L )] and [{VO(OMe)(H2O)}3(L )]· 2 3 2H2O (L = bis(2-hydroxybenzylidene)terephthalohydrazide and L = tris(2-hydroxybenzylidene) benzene-1,3,5-tricarbohydrazide); [Mn2L2O3][PF6]2 (L = 1,4,7-trimethyl-1,4,7-triazacyclononane). For comparison, articles are introduced describing catalysts for the oxidation of alkanes and alcohols with peroxides, which are simple metal salts or mononuclear metal complexes.