Severe Illness Management Support Final Report July 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 / 38 Presidential Elections, 2016
Tuesday, February 23, 2016 15:38:16 PM Received Station: 27881/28010 PRESIDENTIAL ELECTIONS, 2016 (Presidential Elections Act, 2005, Section 48) RESULTS TALLY SHEET DISTRICT: 015 KASESE CONSTITUENCY: 077 BUKONZO COUNTY EAST Parish Station Reg. ABED AMAMA BARYAMUREEB BENON BUTA KIZZA MABIRIZI MAUREEN YOWERI Valid Invalid Total Voters BWANIKA MBABAZI A VENANSIUS BIRAARO BESIGYE JOSEPH FAITH KYALYA KAGUTA Votes Votes Votes KIFEFE WALUUBE MUSEVENI Sub-county: 001 KISINGA 001 KAGANDO 01 KAGANDO II LCI OFFICE (A-L) 504 2 1 3 0 263 0 0 78 347 18 365 0.58% 0.29% 0.86% 0.00% 75.79% 0.00% 0.00% 22.48% 4.93% 72.42% 02 KAGANDO PARISH HQRS (A-L) 460 4 3 0 1 222 2 1 95 328 13 341 1.22% 0.91% 0.00% 0.30% 67.68% 0.61% 0.30% 28.96% 3.81% 74.13% 03 KAGANDO II LCI OFFICE (M -Z) 480 1 0 1 0 235 2 0 70 309 28 337 0.32% 0.00% 0.32% 0.00% 76.05% 0.65% 0.00% 22.65% 8.31% 70.21% 04 KIBURARA BAPTIST CHURCH 460 4 4 3 0 224 3 1 87 326 12 338 1.23% 1.23% 0.92% 0.00% 68.71% 0.92% 0.31% 26.69% 3.55% 73.48% 05 KIBURARA PR. SCH.[A-L] 606 1 3 0 0 285 1 0 87 377 54 431 0.27% 0.80% 0.00% 0.00% 75.60% 0.27% 0.00% 23.08% 12.53% 71.12% 06 KISANGA LCI OFFICE 279 5 1 0 1 111 0 0 67 185 10 195 2.70% 0.54% 0.00% 0.54% 60.00% 0.00% 0.00% 36.22% 5.13% 69.89% 07 NYAMUGASANI PARISH 776 3 2 4 0 428 0 2 112 551 17 568 HQRS. -

Chinese Consortium to Revive Uganda's Copper Mines
CHINESE CONSORTIUM TO REVIVE UGANDA’S COPPER MINES By Fredrick Mugira First published on People’s Daily Online on 17 March 2014 FREDRICK MUGIRA is a multiple award-winning Ugandan journal i st and development communicator who now works with Uganda’s leading multimedia house – Vision Group – as a radio editor. He has reported from various countries in Africa, Europe and most recently in Asia, where he observed African migrants struggling to make a living in Hong Kong as part of a Wits China-Africa Reporting Project tour. Fredrick has a Master’s Degree in Communication for Development from Malmo University in Sweden and has won various continental and national journalism awards including the prestigious CNN/Multichoice African Journali st award in 2009 and the UN Development Journalism Award in 2013. When a Chinese consortium won a concession to revive production at the Kilembe mines in south western Uganda, which had stopped operating in 1982, he applied for a Wits China-Africa Reporting Project grant to find out what the investment would mean for the locals and for Uganda. The knocked-knee driver of the Boda Boda motorcycle revive the mine, however, and clearly the locals are hopeful whistled as he rode. I was sure he heard my question that this could once again mean prosperity for the area. because he changed to a low tone and answered over his shoulder. “Of course we have already started benefiting Kilembe mines today from the resumption of Kilembe copper mines. We The abandoned and ghost-city-like Kilembe copper mines transport people from Kasese town to the mines. -

Fight Against COVID-19
COMMUNITY NEWS Thursday, May 7, 2020 NV31 National COVID-19 fund gets more donations Former Lango Foundation PHOTO BY ABOU KISIGE prime minister sues boss CENTRAL NORTH By Nelson Kiva The Lango paramount chief, Yosam Ebii A day after the National Response Odur, has been dragged to court by to COVID-19 Fund made a his former prime minister, Dr Richard fresh appeal for support, several Nam, challenging him for appointing individuals and corporate Eng. James Ajal as the new premier. organisations flocked the Office Nam filed the notice to sue the of the Prime Minister (OPM) in Lango Cultural Foundation over Kampala to donate cash and non- irregularities in his dismissal from cash items. the position of prime minister by the “We remain committed to paramount chief. accord any necessary assistance Through his lawyer, Emmanuwel to fellow Ugandans and towards Egaru, Nam claims he was dismissed Government’s efforts to combat from office without following legal the coronavirus pandemic,” procedures. He argues that Chapter Sharon Kalakiire remarked while (4), Article 5 of the Lango Cultural handing over a consignment of Foundation constitution state that the items donated by SBC Uganda prime minister can only be dismissed if Limited to the Minister of General he is implicated in abuse of office or if Duties, Mary Karooro Okurut. he is mentally incapacitated. Karooro, who is also the political Minister Karooro Okurut (right) receiving relief items from employees of SBC Uganda advisor to the COVID-19 Fund, was accompanied by Dorothy Kisaka, the fund’s secretary and on Sunday indicated that they had chairperson of the fund, said. -

World Bank Document
Document of The World Bank FOR OFFICIAL USE ONLY Public Disclosure Authorized Report No: 82713-UG PROJECT APPRAISAL DOCUMENT ON A Public Disclosure Authorized PROPOSED SERIES OF IDA PARTIAL RISK GUARANTEES IN THE AMOUNT OF US$ 160 MILLION EQUIVALENT IN SUPPORT OF PROJECTS UNDER THE RENEWABLE ENERGY DEVELOPMENT PROGRAM IN THE REPUBLIC OF UGANDA February 20, 2014 Public Disclosure Authorized Africa Energy (AFTG1) Africa Region: Tanzania, Uganda and Burundi Country Unit (AFCE1) Public Disclosure Authorized This document has a restricted distribution and may be used by recipients only in the performance of their official duties. Its contents may not otherwise be disclosed without World Bank authorization. CURRENCY EQUIVALENTS (Exchange Rate Effective January 31, 2014) Currency Unit = Uganda Shilling (UGX) 2,475 UGX = US$ 1 FISCAL YEAR July 1 – June 30 ABBREVIATIONS AND ACRONYMS BP Bank Procedure BST Bulk Supply Tariff CAS Country Assistance Strategy COD Commercial Operation Date DEG Entrepreneurial Development Cooperation – German DFI Development Finance Institution EAPP Eastern Africa Power Pool DRC Democratic Republic of Congo EPC Engineering, Procurement and Construction ERA Electricity Regulatory Authority ESAP Environment and Social Action Plan ESDP Electricity Sector Development Project ESIA Environmental and Social Impact Assessment ESMP Environmental and Social Management Plan ESMS Environmental and Social Management System ESRS Environmental and Social Review Summary EU European Union EUR Euro FM Financial Management FMO Entrepreneurial -

Kilembe Hospital to Re-Open Today Rumours on ADF Lt
WESTERN NEWS NEW VISION, Tuesday, June 4, 2013 9 UPDF dismisses Kilembe Hospital to re-open today rumours on ADF Lt. Ninsima Rwemijuma, the By JOHN THAWITE He disclosed that the 84 nurses are homeless after the untreated water from Uganda People’s Defence hospital would start by offering their houses were washed the Kasese Cobalt Company Forces second divison Kilembe Mines Hospital in services such as anti-retroviral Faulty away by the floods. factory. We have to purify spokesperson, has warned Kasese district re-opens its therapy, eye treatment, dental He requested for cement, it before using and it is not politicians in the Rwenzori gates to out-patients today, care, orthopaedics and timber and paint to be used enough for a big patient region against spreading after a month’s closure. immunisation. Dr. Edward Wefula, in repairing the hospital’s population,” Wefula added. rumours that Allied Democratic The facility was closed after Wefula said the 200-bed the superintendent of infrastructure. The hospital is co-managed Forces(ADF) rebels have it was ravaged by floods that hospital was not yet ready for Kilembe Mines Hospital, Wefula said the break down by Kilembe Mines, the Catholic crossed into Uganda. He said hit the area on May 1. in-patient admissions and said the sewerage system in the facility’s sewerage Church and the health such people want to disrupt “The out-patient department major surgical operations in the facility was down system had resulted in the ministry. peace. Ninsiima said according is ready to resume services. because most of the essential contamination of water. -

Ministry of Health
UGANDA PROTECTORATE Annual Report of the MINISTRY OF HEALTH For the Year from 1st July, 1960 to 30th June, 1961 Published by Command of His Excellency the Governor CONTENTS Page I. ... ... General ... Review ... 1 Staff ... ... ... ... ... 3 ... ... Visitors ... ... ... 4 ... ... Finance ... ... ... 4 II. Vital ... ... Statistics ... ... 5 III. Public Health— A. General ... ... ... ... 7 B. Food and nutrition ... ... ... 7 C. Communicable diseases ... ... ... 8 (1) Arthropod-borne diseases ... ... 8 (2) Helminthic diseases ... ... ... 10 (3) Direct infections ... ... ... 11 D. Health education ... ... ... 16 E. ... Maternal and child welfare ... 17 F. School hygiene ... ... ... ... 18 G. Environmental hygiene ... ... ... 18 H. Health and welfare of employed persons ... 21 I. International and port hygiene ... ... 21 J. Health of prisoners ... ... ... 22 K. African local governments and municipalities 23 L. Relations with the Buganda Government ... 23 M. Statutory boards and committees ... ... 23 N. Registration of professional persons ... 24 IV. Curative Services— A. Hospitals ... ... ... ... 24 B. Rural medical and health services ... ... 31 C. Ambulances and transport ... ... 33 á UGANDA PROTECTORATE MINISTRY OF HEALTH Annual Report For the year from 1st July, 1960 to 30th June, 1961 I.—GENERAL REVIEW The last report for the Ministry of Health was for an 18-month period. This report, for the first time, coincides with the Government financial year. 2. From the financial point of view the year has again been one of considerable difficulty since, as a result of the Economy Commission Report, it was necessary to restrict the money available for recurrent expenditure to the same level as the previous year. Although an additional sum was available to cover normal increases in salaries, the general effect was that many economies had to in all be made grades of staff; some important vacancies could not be filled, and expansion was out of the question. -

Highlights of the Ebola Virus Disease Preparedness in Uganda
HIGHLIGHTS OF THE EBOLA VIRUS DISEASE PREPAREDNESS IN UGANDA 21st MAY 2019 (12:00 HRS) – UPDATE NO 118 SITUATION UPDATE FROM DEMOCRATIC REPUBLIC OF CONGO FOR 20th MAY 2019 WITH DATA UP TO 19th MAY 2019 Cumulative cases: 1,826 Confirmed cases: 1,738 Probable: 88 Total deaths: 1,218 a) EVD SITUATIONAL UPDATE IN UGANDA There is NO confirmed EVD case in Uganda. Active case search continues in all communities, health facilities and on formal and informal border crossing in all districts especially in the high-risk ones. Alert cases continue to be picked, isolated, treated and blood samples picked for testing by the Uganda Virus Research Institute (UVRI). The alerts are highlighted in the specific district reports below under the Surveillance section. b) PREPAREDNESS IN THE FIELD (PROGRESS AND GAPS) COORDINATION SURVEILLANCE ACTIVITIES Kasese District Achievements Two (2) suspected cases from Kyaka II Camp were detected, samples were picked and taken to Uganda Virus Research Institute (UVRI) for testing. 32 school zonal leaders were trained on chlorine preparation at the district headquarters. Gaps and Challenges 1 There is lack of EVD logistics such as gloves, infrared thermometers, batteries, triple packing etc. Ntoroko District Achievements Support supervision was conducted at PoEs in the district. Surveillance team visited Stella Maris HCIII and MTI facilities where they updated staff and volunteers on EVD. Number of people screened at PoEs in Ntoroko District on 20th May 2019. No PoE site No of persons screened 1 Kigungu 34 2 Ntoroko Main 67 3 Fridge 0 4 Transami 153 5 Kanara 0 6 Rwagara 258 7 Katanga 56 8 Kamuga 99 9 Katolingo 24 10 Mulango 43 11 Rwentuhi 65 12 Haibale South 57 13 Kabimbiri 0 14 Kyapa 53 15 Kayanja I 31 16 Kayanja II 69 17 Budiba 0 2 Total 1,009 Gaps and Challenges Some PoEs have no tents. -

Kasese District Profile.Indd
THE REPUBLIC OF UGANDA Kasese District Hazard, Risk and Vulnerability Profi le 2016 Kasese District Hazard, Risk and Vulnerability Profi le a b Kasese District Hazard, Risk and Vulnerability Profile Contents List of Tables.........................................................................................................................ii List of Figures......................................................................................................................... ii Acknowledgment .................................................................................................................. iii Executive Summary ............................................................................................................. iv Acronyms ............................................................................................................................ vi Definition of Terms .............................................................................................................. vii Introduction .......................................................................................................................... 1 Objectives ............................................................................................................................ 1 Methodology ........................................................................................................................ 1 District Overview ................................................................................................................. -

Abbreviated Resettlement and Compensation Action Plan
ABBREVIATED Public Disclosure Authorized RESETTLEMENT AND COMPENSATION ACTION PLAN Public Disclosure Authorized Public Disclosure Authorized NYAMWAMBA HYDROPOWER PROJECT KILEMBE SUB-COUNTY KASESE DISTRICT Public Disclosure Authorized SOUTH ASIA ENERGY VS HYDRO (PVT) LIMITED MANAGEMENT SYSTEMS CACL CONSULT LTD DECEMBER 2010 Resettlement Action Plan for Nyamwamba Small Hydro Power Project THE RAP STUDY TEAM This is to certify that the Resettlement and Compensation Action Plan for the proposed Nyamwamba small hydro power project in Kilembe Sub‐county was conducted under our direct supervision and the information provided in this report is correct to the best of our knowledge. Name Responsibility Signature Mr. Ochola Bernard Lead Sociologist Mr. Tumusiime Alfred Environment Systems Analyst Ms. Aisu Elizabeth Sociologist Mr. Balinda S. Birungi Valuer Mr. Otwane Ben Land Surveyor South Asia Energy Management Systems VS Hydro (pvt) Ltd / CaCl Consulting Ltd ii Resettlement Action Plan for Nyamwamba Small Hydro Power Project TABLE OF CONTENTS THE RAP STUDY TEAM ........................................................................................................................ ii LIST OF ACRONYMS ........................................................................................................................... vi KEY DEFINITIONS .............................................................................................................................. vii EXECUTIVE SUMMARY ...................................................................................................................... -

Ebola Virus Disease in Uganda
EBOLA VIRUS DISEASE IN UGANDA Situation Report 15 Jun 2019 SitRep #04 Deaths 03 Cases 1. Situation update 03 Key Highlights 03 cumulative cases (00 probable 03 confirmed) All (03) confirmed cases have died (CFR =100%) There are 96 contacts under follow up o None has developed symptoms to date Active case search and death surveillance are ongoing in the health facilities and the communities as the district response team continue to investigate all alerts The burial of the Queen Mother tomorrow has been moved to Bundibugyo. Several interventions have been put in place; hand washing facilities, screening of all people attending the burial, securing of all entrances, footbaths set up and education of the masses about EVD Background On 11th June 2019, the Ministry of Health of Uganda declared the 6th outbreak of Ebola Virus Disease (EVD) in the country affecting Kasese district in South Western Uganda. The first case was a five-year-old child with a recent history of travel to the Democratic Republic of Congo (DRC). This child was one of 6 people that travelled from the DRC while still being monitored as suspect cases following a burial of the grandfather who succumbed to EVD. The child was ill by the time he crossed into Uganda and the mother took him for medical care at Kagando hospital in Kasese district with symptoms of vomiting blood, bloody diarrhea, muscle pain, headache, fatigue and abdominal pain. The child tested positive for Ebola Zaire by 1 PCR and he later died on 11th June 2019. Two other members of the family, a grandmother and 3-year-old brother also tested positive for Ebola on 12 June 2019 and the grandmother died later the same day. -
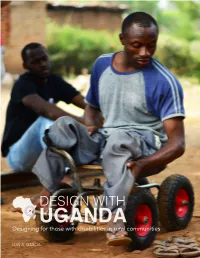
UGANDA for Those with Disabilities in Rural Communities
DESIGN WITH DesigningUGANDA for those with disabilities in rural communities LUIS A. GARCIA Acknowledgements: Special thanks to: Jim Dewar Nelson Mukiika Kio Bjarki Hallgrimsson Jennifer Vandermeer Walter Zanneti Ramathan Kavuma Navin Parekh Zoe Krug Jennifer Tataryn Kisembo Salim Amanda Cox Charles Williams Andrew Dewar Moses Lena Sitnikova Joseph Nate Williams Bja My amazing classmates. i 1 Table of Contents Executive Summary 1 Research 3 Ideation 13 Preliminary Design Development 19 Definitive Design Development 27 Final Design Development 37 Appendix A 45 Appendix B 47 Appendix C Executive Summary This project started through a collaboration Having done much research the ideation between the READ Initiative at Carleton phase was started first by the development of University and CanUgan, a non-for-profit a mindmap. This mindmap helped understand organization found in Ottawa, Canada by the many complex problems and, how they Navin Parekh. CanUgan works closely with are related, surrounding the focus of the KADUPEDI, The Kasese District Union of research. This mindmap also helped attain a Persons with Disabilities, in Uganda. Both deeper understanding of each problem and CanUgan and KADUPEDI focus on providing the root source of them. Ideation followed by support through assistive devices to people the development of concepts dealing with in need. CanUgan’s proposal to the School of water management, either water collection Industrial Design at Carleton University was or water distribution. This process proved to design innovative devices for people with helpful but the best solution evetually found disabilities in Uganda. was a very complex system of creating a water source and a pump. -

2017 Statistical Abstract – Ministry of Energy and Mineral Development
THE REPUBLIC OF UGANDA MINISTRY OF ENERGY AND MINERAL DEVELOPMENT 2017 STATISTICAL ABSTRACT 2017 Statistical Abstract – Ministry of Energy and Mineral Development i FOREWORD The Energy and Mineral Development Statistics Abstract 2017 is the eighth of its kind to be produced by the Ministry. It consolidates all the Ministry’s statistical data produced during the calendar year 2017 and also contains data dating five years back for comparison purposes. The data produced in this Abstract provides progress of the Ministry’s contribution towards the attainment of the commitments in the National Development Plan II and the Ministry’s Sector Development Plan FY2015/16 – 2019/20. The Ministry’s Statistical Abstract is a vital document for dissemination of statistics on Energy, Minerals and Petroleum from all key sector players. It provides a vital source of evidence to inform policy formulation and further strengthens and ensures the impartiality, credibility of data/information collected. The Ministry is grateful to all its stakeholders most especially the data producers for their continued support and active participation in the compilation of this Abstract. I wish also to thank the Energy and Mineral Development Statistics Committee for the dedicated effort in compilation of this document. The Ministry welcomes any contributions and suggestions aimed at improving the quality of the subsequent versions of this publication. I therefore encourage you to access copies of this Abstract from the Ministry’s Head Office at Amber House or visit the Ministry’s website: www. energyandminerals.go.ug. Robert Kasande PERMANENT SECRETARY 2017 Statistical Abstract – Ministry of Energy and Mineral Development ii TABLE OF CONTENTS FOREWORD .....................................................................................................................................................