This Is My Thesis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
September 2008 You Can Only Imagine How Happy We Are to Bring the Latest Edition of LPSS Editor@ Lpssmatters .Com Matters to You
LPSS Matters Official Alumni Newsletter of Lorne Park Secondary School Volume 8, Issue 1 Dear Grads, September 2008 You can only imagine how happy we are to bring the latest edition of LPSS Editor@ LPSSMatters .com Matters to you. www. LPSSMatters .com Sorry that it has taken this long but we had a few changes at the ole newsletter and used this opportunity to ramp staff up and to collect all kinds of news and stories for you to read. In this issue: One of those ramping up was me. • Found - new Editor for LPSS Matters What a treat it has been to read your letters, comments and the contributions of our dedicated columnist staff. Thanks for making the effort to get them to us. I found myself rereading some of these several times both because they Reunion 2007 • were so interesting and because I fouled up while editing and learning how to Reflections pg2 use Publisher and so lost them in this process. Fortunately with this tool you never really lose anything it just disappears and so the game is more like hide and seek. My mother use to say I was slow but sure—slow to learn and sure to • Connections pg11 forget—she was apparently right I must reluctantly conclude! However I feel confident to now say we will not be so long bringing you the • LPSS Matters a next edition. In fact, make a note to be on the look out for our winter edition history pg12 sometime in early February. I know our team is chomping at the bit to make their respective contributions and so as the ink dries here preparations are already under way for our next edition. -

2018 06 28 Regional Council Minutes
-276- THE COUNCIL OF THE REGIONAL MUNICIPALITY OF PEEL June 28, 2018 Regional Chair Dale called the meeting of Regional Council to order at 9:31 a.m. in the Council Chamber, Regional Administrative Headquarters, 10 Peel Centre Drive, Suite A, Brampton. 1. ROLL CALL Members Present: G. Carlson M. Mahoney D. Cook S. McFadden ® B. Crombie M. Medeiros F. Dale E. Moore J. Downey M. Palleschi C. Fonseca K. Ras G. Gibson P. Saito A. Groves* B. Shaughnessy N. Iannicca J. Sprovieri J. Innis R. Starr ® L. Jeffrey A. Thompson* J. Kovac Members Absent: G. Mi les Due to illness C. Parrish Due to other municipal business Also Present: D. Szwarc, Chief Administrative Officer; M. Killeavy, Acting Commissioner of Corporate Services; S. VanOfwegen, Commissioner of Finance and Chief Financial Officer and Acting Commissioner of Digital and Information Services; P. O’Connor, Regional Solicitor; J. Smith, Commissioner of Public Works; J. Sheehy, Commissioner of Human Services; N. Polsinelli, Commissioner of Health Services; K. Bingham, Acting Medical Officer of Health; K. Lockyer, Regional Clerk and Director of Clerk’s; C. Thomson, Legislative Specialist; S. Valleau, Legislative Technical Coordinator; H. Gill, Legislative Technical Coordinator 2. DECLARATIONS OF CONFLICTS OF INTEREST Councillor Palleschi declared a conflict of interest with respect to Item 10.14, listed on the June 28, 2018 Regional Council agenda, as his residence is located in close proximity of the subject road. * See text for arrivals ® See text for departures Denotes alternate member Region of Peel -277- Council Minutes June 28, 2018 3. APPROVAL OF MINUTES 3.1. June 14, 2018 Regional Council meeting Moved by Councillor McFadden, Seconded by Councillor Kovac; That the minutes of the June 14, 2018 Regional Council meeting be approved; And further, that the June 14, 2018 Closed Session Report listed as Item 19.1 on the June 28, 2018 Regional Council agenda be amended to note the absence of Councillor Jeffrey as due to other municipal business. -
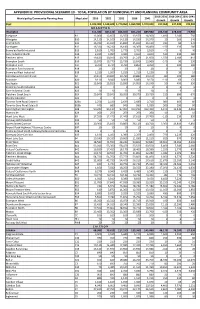
Appendix III: Provisional Scenario 10
APPENDIX III: PROVISIONAL SCENARIO 10 - TOTAL POPULATION BY MUNICIPALITY AND PLANNING COMMUNITY AREA 2016-2031 2016-2041 2031-2041 Municipality/Community Planning Area Map Label 2016 2021 2031 2036 2041 Growth Growth Growth Peel 1,433,000 1,538,600 1,770,060 1,869,990 1,970,040 337,060 537,040 199,980 B R A M P T O N Brampton 611,480 687,150 816,020 855,220 889,980 204,540 278,500 73,960 Snelgrove B1 12,060 12,650 13,550 13,970 14,300 1,490 2,240 750 Westgate B10 14,110 14,100 14,130 14,230 14,370 20 260 240 Central Park B11 16,030 15,910 15,840 15,960 16,110 -190 80 270 Northgate B12 16,330 16,230 16,180 16,300 16,460 -150 130 280 Bramalea North Industrial B13 2,810 2,780 2,770 2,790 2,810 -40 0 40 Gore Industrial North B14 2,910 3,090 3,440 3,660 3,820 530 910 380 Fletchers West B15 19,420 20,010 20,790 21,220 21,600 1,370 2,180 810 Brampton South B16 13,870 13,770 13,730 13,840 13,960 -140 90 230 Brampton East B17 9,760 9,730 9,760 9,850 9,950 0 190 190 Brampton East Industrial B18 20 20 20 20 20 0 0 0 Bramalea West Industrial B19 1,210 1,200 1,210 1,210 1,220 0 10 10 Sandalwood Industrial East B2 10,870 10,820 10,790 10,880 10,970 -80 100 180 Avondale B20 9,110 9,040 9,000 9,080 9,170 -110 60 170 Southgate B21 13,840 13,810 13,890 14,050 14,240 50 400 350 Bramalea South Industrial B22 0 0 0 0 0 0 0 0 Gore Industrial South B23 10 10 10 10 10 0 0 0 Fletchers Creek South B24 29,840 29,840 30,050 30,370 30,720 210 880 670 Steeles Industrial B25 0 0 0 0 0 0 0 0 Toronto Gore Rural Estate A B26a 2,250 2,430 2,630 2,680 2,710 380 460 80 Toronto -

Churchill Meadows Community Profile
CITY OF MISSISSAUGA Planning and Building Department February, 2004 Churchill Meadows Community Profile History processing of development applications. mix of uses, a connected system of natural From 1987 to 1997 draft secondary plans features, parks, schools and stormwater The Churchill Meadows Residential District were prepared and the two areas were management facilities, a grid pattern of was originally part of the Town of Oakville combined into the Churchill Meadows streets and the creation of neighbourhood and designated for agricultural uses. With Planning District. During this time the last units. Lands in the north and south part of the advent of Regional Government in 1974, remaining greenfield was occupied by the planning district are under construction the City of Mississauga was established and several working farms, along with individual and applications for the central area are Churchill Meadows was incorporated residences along the east and west sides of currently being processed. through the extension of its westerly Tenth Line West and the east side Table 1 - 2001 Total Population boundary to Ninth Line. of Ninth Line. Churchill In 1997 urban design guidelines The Official (Primary) Plan of 1981 identified Churchill Meadows as the major land uses for this area as were prepared for the Churchill Mississauga Meadows a % of residential for the lands north of Eglinton Meadows Planning District Avenue West (Winston Churchill Residential providing direction to the public Mississauga District) and mixed industrial and commercial and private sectors with respect to Male 2,675 301,495 0.9% the design intent of the City in for the lands located south of Eglinton Fe m ale 2,770 309,235 0.9% Avenue West (Central Business District). -

Heritage Impact Assessment 1472 Indian Road, Mississauga
Appendix 1 8.1 VE GROUP PROJECT NUMBER: 201-10290-00 HERITAGE IMPACT ASSESSMENT 1472 INDIAN ROAD, MISSISSAUGA REVISED NOVEMBER 30, 2020 8.1 HERITAGE IMPACT ASSESSMENT 1472 INDIAN ROAD, MISSISSAUGA VE GROUP FINAL PROJECT NO.: 201-10290-00 DATE: REVISED NOVEMBER 30, 2020 WSP 582 LANCASTER STREET WEST KITCHENER, ON N2K 1M3 T: +1 519 743 8777 WSP.COM 8.1 SIGNATURES PREPARED BY November 30, 2020 Chelsey Tyers, BES, MCIP, RPP Date Cultural Heritage Specialist APPROVED1 BY November 30, 2020 Joel Konrad, PhD, CAHP, Date Cultural Heritage Lead - Ontario WSP Canada Inc. (“WSP”) prepared this report solely for the use of the intended recipient in accordance with the professional services agreement between the parties. In the event a contract has not been executed, the parties agree that the WSP General Terms for Consultant shall govern their business relationship which was provided to you prior to the preparation of this report. The report is intended to be used in its entirety. No excerpts may be taken to be representative of the findings in the assessment. The conclusions presented in this report are based on work performed by trained, professional and technical staff, in accordance with their reasonable interpretation of current and accepted engineering and scientific practices at the time the work was performed. The content and opinions contained in the present report are based on the observations and/or information available to WSP at the time of preparation, using investigation techniques and engineering analysis methods consistent with those ordinarily exercised by WSP and other engineering/scientific practitioners working under similar conditions, and subject to the same time, financial and physical constraints applicable to this project. -

Phase One Environmental Site Assessment Lakeshore Road West
REPORT Phase One Environmental Site Assessment Lakeshore Road West and Tennyson Avenue, Mississauga, ON - Manhole Location No.7 Location Front Street Station Wastewater Project 17-2415S Submitted to: Ajay Puri, M.E. (Env.), P.Eng. Project Manager, Capital Works Wastewater Division, Collection & Communal Treatment Region of Peel 10 Peel Centre Drive, Suite A, 1st Floor, Room 101 Brampton, Ontario Submitted by: Golder Associates Ltd. 6925 Century Avenue, Suite #100, Mississauga, Ontario, L5N 7K2, Canada +1 905 567 4444 1787556_PhaseOneESA_EMH_RevA May 3, 2019 May 3, 2019 1787556_PhaseOneESA_EMH_RevA Distribution List 1 e-copy: Region of Peel 1 e-copy: Golder Associates Ltd. i May 3, 2019 1787556_PhaseOneESA_EMH_RevA Table of Contents 1.0 EXECUTIVE SUMMARY.................................................................................................................................. 1 2.0 INTRODUCTION .............................................................................................................................................. 2 2.1 Phase One Property Information.......................................................................................................... 2 3.0 SCOPE OF INVESTIGATION .......................................................................................................................... 2 4.0 RECORDS REVIEW ........................................................................................................................................ 3 4.1 General ................................................................................................................................................ -

Andrew Tamburello, Director Humanity Mississauga Board Members and As a Driver Thorn Lodge Park for Meals on Wheels
President’s Message - Spring 2011 Hello Neighbours! Andrewndrrew TamburelloTTamburaambureello With spring in its early days I hope you enjoy our 8th issue of the Sheridan Times. SalesSales RepresentativeRepresentative 2010 was another busy year in the Homelands with the start of annual traditions and the continuation of established ones. Several streets - Barnstone and Belfast - had street parties with others now busy planning ones for 2011. If you’re interested on how to run your own street party, let us know. It’s easy and a great way to meet and re-connect with neighbours. office:officice:: 905 - 285 - 0343343 Shakespeare in the Park had its 2nd successful year performing in Thornlodge Park to a crowd of over 400 residents dirdirect:eect:: 647 - 281 - 3996996 and returned in the winter with the classic “A Christmas Carol” to entertain residents at Sheridan Park Public School. The Humber Valley Shakespeare troop is coming back this summer. Check for details in this issue. We are very excited about the re-opening of the David Ramsey Pool set for July 9th. The Mayor will be there and we are planning a special day for residents (details are on page 19 of this issue of Sheridan Times). Thornlodge Park is an integral part of our community and SHORA has been working with the City to maximize its potential for all residents. This year we installed an outdoor skating rink and, thanks to Board member Andrew Commissionsmissionsns as lowlow asas 1% Tamburello and his volunteers, it was a success in spite of the wonky weather and we received positive feedback. -

School/Library Name | Nom De L'école/De La Bibliothèque City/Town
LOOK WHO WAS SIGNED UP FOR I READ CANADIAN DAY IN 2020? Province/Territory School/Library Name | Nom de l'école/de la City/Town | Ville | Province / bibliothèque Territoire A. B. Lucas S.S. London Ontario Abbotsford Traditional Middle School Abbotsford British Columbia Abraar Elementary School Ottawa Ontario Abraham Erb Public School Waterloo Ontario Adam Beck Ps Toeonto Ontario Adelaide W.G. MacDonald Strathroy Ontario Admaston/Bromley Public Library Douglas Ontario Agincourt Road Public School Ottawa Ontario Ajax Public Library Ajax Ontario Alcona Glen Innisfil Ontario Alcona Glen Elementary School Innisfil Ontario Aldershot High School Burlington Ontario Alexander von Humboldt German International Baie D Urfé Quebec School Alf Cuthbert School Moosehorn Manitoba Algonquin P.S Woodstock Ontario Algonquin P.S Woodstock Ontario All Saints School Mississauga Ontario Allan A. Martin Sr. Public School Mississauga Ontario Allan Drive Middle School Bolton Ontario Allan Drive Middle School Bolton Ontario Allandale Heights P.S. Barrie Ontario Alliance Public School 700 Stones St., North Bay Ontario Alliance Public School North Bay Ontario Allion Elementary LaSalle Quebec Alliston Union PS Alliston Ontario Alloa Public School - Caledon Caledon Ontario Almaguin Highlands Secondary School Library South River Ontario Alpha Secondary Burnaby British Columbia Alton Public School Mississauga/Brampton Area Ontario Alvin Curling PS Toronto Ontario Annandale School Tillsonburg Ontario Annandale School Tillsonburg Ontario Annapolis Valley Regional Library -

Lakeview: Journey from Yesterday Kathleen A
Lakeview: Journey From Yesterday Kathleen A. Hicks LAKEVIEW: JOURNEY FROM YESTERDAY is published by The Friends of the Mississauga Library System 301 Burnhamthorpe Road, West, Mississauga, Ontario, L5B 3Y3 Copyright © 2005 by the Mississauga Library System All rights reserved Lakeview: Journey From Yesterday ISBN 0-9697873-6-7 II Written by Kathleen A. Hicks Cover design by Stephen Wahl Graphic layout by Joe and Joyce Melito Lakeview Sign by Stephen Wahl Back Cover photo by Stephen Wahl No part of this publication may be produced in any form without the written permission of the Mississauga Library System. Brief passages may be quoted for books, newspaper or magazine articles, crediting the author and title. For photographs contact the source. Extreme care has been taken where copyright of pictures is concerned and if any errors have occurred, the author extends her utmost apology. Care also has been taken with research material. If anyone encounters any discrepancy with the facts contained herein, (Region of Peel Archives) please send your written information to the author in care of the Mississauga Library System. Lakeview: Journey From Yesterday Other Books By Kathleen A. Hicks (Stephen Wahl) III The Silverthorns: Ten Generations in America Kathleen Hicks’ V.I.P.s of Mississauga The Life & Times of the Silverthorns of Cherry Hill Clarkson and its Many Corners Meadowvale: Mills to Millennium VIDEO Riverwood: The Estate Dreams are Made of IV Dedication dedicate this book to my family, the Groveses of Lakeview, where I was born. My grandfather, Thomas Jordan, and my father, Thomas Henry, were instrumental in building many houses and office buildings across southern Ontario. -
Table of Contents
: : TABLE OF CONTENTS Acknowledgements i Executive Summary and Recommendations ii 1. Introduction 1 2. Literature Review 3 3. Methodology 8 4. Findings and Discussion: Primary Sources 10 4.1 Respondents’ Characteristics 11 4.2 Diabetes in the South Asian Population in Peel 17 4.3 Resources and Prevention Programming 33 4.4 Gaps and Barriers 45 4.5 Recommendations 49 5. Findings and Discussion: Secondary Sources 54 5.1 Socio-Economic Status of South Asians in Peel 55 5.2 Neighbourhood Characteristics by Diabetes Services 69 6. Conclusions and Recommendations 72 References 75 Appendices 78 Appendix 1: Qualitative Studies from 2005-2014 78 Appendix 2: Organizations of Key Informants 81 Appendix 3: Background on Socio-Economic Status & Related Indicators 82 3.1 Description and Size of the South Asian Population in Peel Neighbourhoods, 2006 82 3.2 Technical Notes 83 3.3 Definitions 85 3.4 Fact Sheet for the South Asian Population in Peel Region 87 Appendix 4: Potential Priority Peel Neighbourhoods by South Asian Population, Socio- 88 Economic Status of South Asians and Number of Diabetes Related Services Appendix 5: Research Team 89 ACKNOWLEDGMENTS St. Michael’s Hospital wishes to acknowledge the funding support of the Canadian Institute of Health Research (CIHR) for the production of this report. St. Michael’s Hospital thanks all the organizations, service providers, and community members who participated in and supported this important research study. Special thanks to Dr. Aisha Lofters, Scientist, Li Ka Shing Knowledge Institute, St. Michael's -

Your Team Scene by Scotiabank MHL Office 3065 Ridgeway Dr., Unit 34 Mississauga, Ontario L5L 5M6 Phone: (905) 607-1118
YOUR TEAM SCENE by Scotiabank MHL Office 3065 Ridgeway Dr., Unit 34 Mississauga, Ontario L5L 5M6 Phone: (905) 607-1118 What’s Inside • MHL Golf Tournament............................ 1 MHL GOLF • LPHA “Big Score”................................... 2 MHL GOLF • Mississauga Sport Council Awards.........3 TTOURNAMENOURNAMENTT • MHL Referral Program.......................... 3 • Equipment Exchange - Save money!.......3 Ninety-three golfers teed off on a cool May 5th for the 13th Annual MHL Golf Tournament at Eagle Ridge Golf Club in • MHL Awards Night.................................4 Georgetown. This event raised $4000 for the MHL Play More • MHL Awards Night - Special Awards......5 Program, which helps reduce the cost of playing hockey for financially challenged families. Thanks to the many golfers who enjoyed a round of golf and dinner – MHL Directors, Association Directors, Coaches, Mississauga Sports Council, MHL sponsors Boston Pizza and Scotiabank, the GTHL, Missis- sauga Steelheads and seven foursomes of MHL referees who REGISTRATION are the biggest supporters of this event. Congratulations to is NOW OPEN for 2015/16 all the prize winners and many thanks to Dave Newsome and Don’t Be Dissappointed! the Eagle Ridge staff for hosting this great day! Low gross winners, Mark Registration for the 2015-16 hockey season Zizek (President, Applewood is open! Hockey), Brett Webster (former MHL player, referee Registration information is posted on all Associa- and timekeeper}, Paul Yager tions’ websites. (Mississauga Steelheads, Man- ager Sales and Minor Hockey We encourage you to register early. Remember many Asso- Relations) and Scott Rogers ciations offer discounts for early registration. Also all (Mississauga Steelheads, Vice- President Business Operations) Associations are currently planning for the new season ordering uniforms, organizing coaches and arranging practice ice. -

Reeve Robert Speck at the Opening of the Clarkson Lorne Park Branch
243 Part Four 1951-2002 Part Four 1951 - 2000 244 Previous page: Reeve Robert Speck at the opening of the Clarkson Lorne Park Branch Library, with Michael and Julie Giguerre, 15 October 1967 (Mississsauga Library System) Clarkson and its Many Corners The First Dentist – 1953 HE STARTED HIS PRACTICE IN A TWO STOREY, BRICK building at 1651 Lakeshore Road West that Phyllis’ father, William H. Trenwith, and brother, Bill, constructed on property grandfather William 245 Dr. John Williams (Phyllis Williams) larkson’s first dentist was John Williams, who took his dentistry degree at the Uni- versity of Toronto and graduated in 1951. After practising in Beamsville for a year, he moved to Clarkson, where he Cmarried Phyllis Trenwith in May, 1952. Site of the Trenwill Building, 1950 (Phyllis Williams) Part Four 1951 - 2000 D. and John purchased from Louisa Fitzgerald on July 7, 1953. It became the Trenwill Building, and it is still there today housing the Canadian Sportrent and Pandora’s Box, a florist and gift shop, with apartments on the second floor. John had three generations of Clarksonites as patients. When the Rotary Club of Clarkson was founded in 1965, he was the first president. Although the Trenwill Building was sold in May, 1968, to Douglas Stanton and has changed owners several times over the years, John practised there for 36 years. In 1989, he sold his practice to Dr. Gabriel Bako and worked with him at the Turtle Creek Dental Offices in Clarkson Village, until his retirement in 1995. Phyllis, her father, and her children, Michael, Pamela and Dale, were born and raised on Trenwith property.