Doctors Opposed This Ambulance Service
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Minutes of Parliament Present
(Ninth Parliament - First Session) No. 62.] MINUTES OF PARLIAMENT Thursday, March 25, 2021 at 10.00 a.m. PRESENT : Hon. Mahinda Yapa Abeywardana, Speaker Hon. Angajan Ramanathan, Deputy Chairperson of Committees Hon. Mahinda Amaraweera, Minister of Environment Hon. Dullas Alahapperuma, Minister of Power Hon. Mahindananda Aluthgamage, Minister of Agriculture Hon. Udaya Gammanpila, Minister of Energy Hon. Dinesh Gunawardena, Minister of Foreign and Leader of the House of Parliament Hon. (Dr.) Bandula Gunawardana, Minister of Trade Hon. Janaka Bandara Thennakoon, Minister of Public Services, Provincial Councils & Local Government Hon. Nimal Siripala de Silva, Minister of Labour Hon. Vasudeva Nanayakkara, Minister of Water Supply Hon. (Dr.) Ramesh Pathirana, Minister of Plantation Hon. Johnston Fernando, Minister of Highways and Chief Government Whip Hon. Prasanna Ranatunga, Minister of Tourism Hon. C. B. Rathnayake, Minister of Wildlife & Forest Conservation Hon. Chamal Rajapaksa, Minister of Irrigation and State Minister of National Security & Disaster Management and State Minister of Home Affairs Hon. Gamini Lokuge, Minister of Transport Hon. Wimal Weerawansa, Minister of Industries Hon. (Dr.) Sarath Weerasekera, Minister of Public Security Hon. M .U. M. Ali Sabry, Minister of Justice Hon. (Dr.) (Mrs.) Seetha Arambepola, State Minister of Skills Development, Vocational Education, Research and Innovation Hon. Lasantha Alagiyawanna, State Minister of Co-operative Services, Marketing Development and Consumer Protection ( 2 ) M. No. 62 Hon. Ajith Nivard Cabraal, State Minister of Money & Capital Market and State Enterprise Reforms Hon. (Dr.) Nalaka Godahewa, State Minister of Urban Development, Coast Conservation, Waste Disposal and Community Cleanliness Hon. D. V. Chanaka, State Minister of Aviation and Export Zones Development Hon. Sisira Jayakody, State Minister of Indigenous Medicine Promotion, Rural and Ayurvedic Hospitals Development and Community Health Hon. -

Ranil Wickremesinghe Sworn in As Prime Minister
September 2015 NEWS SRI LANKA Embassy of Sri Lanka, Washington DC RANIL WICKREMESINGHE VISIT TO SRI LANKA BY SWORN IN AS U.S. ASSISTANT SECRETARIES OF STATE PRIME MINISTER February, this year, we agreed to rebuild our multifaceted bilateral relationship. Several new areas of cooperation were identified during the very successful visit of Secretary Kerry to Colombo in May this year. Our discussions today focused on follow-up on those understandings and on working towards even closer and tangible links. We discussed steps U.S. Assistant Secretary of State for taken by the Government of President South and Central Asian Affairs Nisha Maithripala Sirisena to promote recon- Biswal and U.S. Assistant Secretary of ciliation and to strengthen the rule of State for Democracy, Human Rights law as part of our Government’s overall Following the victory of the United National Front for and Labour Tom Malinowski under- objective of ensuring good governance, Good Governance at the general election on August took a visit to Sri Lanka in August. respect for human rights and strength- 17th, the leader of the United National Party Ranil During the visit they called on Presi- ening our economy. Wickremesinghe was sworn in as the Prime Minister of dent Maithirpala Sirisena, Prime Min- Sri Lanka on August 21. ister Ranil Wickremesinghe and also In keeping with the specific pledge in After Mr. Wickremesinghe took oaths as the new met with Minister of Foreign Affairs President Maithripala Sirisena’s mani- Prime Minister, a Memorandum of Understanding Mangala Samaraweera as well as other festo of January 2015, and now that (MoU) was signed between the Sri Lanka Freedom government leaders. -

THE SOCIAL MARKET ECONOMY MODEL - Economic Research CAN IT BE EMULATED in the GLOBAL Volume 4 (1) December 2016 SLJER.04.01.P2: Pp
PERSPECTIVES Sri Lanka Journal of THE SOCIAL MARKET ECONOMY MODEL - Economic Research CAN IT BE EMULATED IN THE GLOBAL Volume 4 (1) December 2016 SLJER.04.01.P2: pp. 123-134 SOUTH? Sri Lanka Forum of University Economists Sumanasiri Liyanage S L J E R Dean, Faculty of Management and Finance, SANASA Campus Ltd., Sri Lanka Chamari Jayani Wijayawardane Assistant Lecturer, SANASA Campus Ltd., Sri Lanka INTRODUCTION The concept of a social market economy (SME) came to play a significant role in Sri Lankan development discourse when it was revealed in late-2014 at the height of the presidential election, that the new government under Maithreepala Sirisena and- Ranil Wickramasinghe would follow the SME model in articulating its economic policies: likely the first time such an idea had surfaced in a Sri Lankan election campaign. Karu Jayasuriya, the Speaker of Parliament, stated at the time that an SME would contribute to achieving the fivefold development strategy suggested by Prime Minister Ranil Wickramasinghe, so that it would uplift the economic standards of the people and create an equitable society (Sri Lanka putting together Social Market Economy Model, 2015). The fivefold development plan titled ‘Our Solutions to Your Problems’ has been formulated targeting five main areas: (economy, infrastructure facilities, prevention of frauds and malpractices as well as freedom and education). According to the Prime Minister, it will give priority to improving the economy such that more youth may be employed and the incomes of people may increase within a period of 60 months. The plan will next address the improvement of people's general welfare and infrastructure facilities. -

Global Tamil Forum
Global Tamil Forum உலக தமிழ ேபரைவ GTF News Update 17th to 19 th October 2015 --GTF IN THE MEDIA— THE SUNDAY LEADER **COMMENTS CAN BE POSTED** Mending Broken Hearts < http://www.thesundayleader.lk/2015/10/18/mending-broken-hearts/ > --NEWS— THE HINDU **COMMENTS CAN BE POSTED** Sirisena has agreed to release prisoners: TNA < http://www.thehindu.com/news/international/sirisena-has-agreed-to-release-prisoners- tna/article7770989.ece > COLOMBO GAZETTE **COMMENTS CAN BE POSTED** TNA will stage fast if President makes u-turn < http://colombogazette.com/2015/10/18/tna-will-stage-fast-if-president-makes-u-turn/ > THE NATION **COMMENTS CAN BE POSTED** President pledges to resolve Tamil prisoners’ issue by Nov 7 < http://nation.lk/online/2015/10/17/president-pledges-to-resolve-tamil-prisoners-issue-by-nov-7/ > THE SUNDAY TIMES **COMMENTS CAN BE POSTED** Detainees call off fast; Govt. assures speedy solution < http://www.sundaytimes.lk/151018/news/detainees-call-off-fast-govt-assures-speedy-solution- 168310.html > THE SUNDAY LEADER **COMMENTS CAN BE POSTED** No One Within TNA Opposes The Resolution – Dharmalingam Siddharthan < http://www.thesundayleader.lk/2015/10/18/no-one-within-tna-opposes-the-resolution- dharmalingam-siddharthan/ > THE HINDU **COMMENTS CAN BE POSTED** Death toll in last stage of Eelam War uncertain: Ranil Wickremesinghe < http://www.thehindu.com/news/international/death-toll-in-last-stage-of-eelam-war-uncertain- ranil-wickremesinghe/article7777623.ece > COLOMBO GAZETTE **COMMENTS CAN BE POSTED** Government strongly defends resolution -

Minutes of Parliament Present
(Eighth Parliament - First Session) No. 134. ] MINUTES OF PARLIAMENT Tuesday, December 06, 2016 at 9.30 a. m. PRESENT : Hon. Karu Jayasuriya, Speaker Hon. Thilanga Sumathipala, Deputy Speaker and Chairman of Committees Hon. Ranil Wickremesinghe, Prime Minister and Minister of National Policies and Economic Affairs Hon. (Mrs.) Thalatha Atukorale, Minister of Foreign Employment Hon. Wajira Abeywardana, Minister of Home Affairs Hon. John Amaratunga, Minister of Tourism Development and Christian Religious Affairs and Minister of Lands Hon. Mahinda Amaraweera, Minister of Fisheries and Aquatic Resources Development Hon. (Dr.) Sarath Amunugama, Minister of Special Assignment Hon. Gayantha Karunatileka, Minister of Parliamentary Reforms and Mass Media and Chief Government Whip Hon. Ravi Karunanayake, Minister of Finance Hon. Akila Viraj Kariyawasam, Minister of Education Hon. Lakshman Kiriella, Minister of Higher Education and Highways and Leader of the House of Parliament Hon. Mano Ganesan, Minister of National Co-existence, Dialogue and Official Languages Hon. Daya Gamage, Minister of Primary Industries Hon. Dayasiri Jayasekara, Minister of Sports Hon. Nimal Siripala de Silva, Minister of Transport and Civil Aviation Hon. Palany Thigambaram, Minister of Hill Country New Villages, Infrastructure and Community Development Hon. Duminda Dissanayake, Minister of Agriculture Hon. Navin Dissanayake, Minister of Plantation Industries Hon. S. B. Dissanayake, Minister of Social Empowerment and Welfare ( 2 ) M. No. 134 Hon. S. B. Nawinne, Minister of Internal Affairs, Wayamba Development and Cultural Affairs Hon. Gamini Jayawickrama Perera, Minister of Sustainable Development and Wildlife Hon. Harin Fernando, Minister of Telecommunication and Digital Infrastructure Hon. A. D. Susil Premajayantha, Minister of Science, Technology and Research Hon. Sajith Premadasa, Minister of Housing and Construction Hon. -

Ministry of Foreign Affairs Sri Lanka Annual Performance
MINISTRY OF FOREIGN AFFAIRS SRI LANKA ANNUAL PERFORMANCE REPORT 2017 MINISTRY OF FOREIGN AFFAIRS Contents Page No 1. Mission, Subjects and Functions of the Ministry of Foreign 1 Affairs 2. Preface 3 - 5 3. Organizational Chart of the Ministry 7 4. Progress Report of the Divisions - Africa Division 9 - 27 - Consular Affairs Division 29 - 35 - East Asia and Pacific Division 37 - 80 - Economic Affairs and Trade Division 81 - 88 - European Union, Multilateral Treaties and Commonwealth 89 - 95 Division - Finance Division 97 - 102 - General Administration Division 103 - 106 - Legal Division 107 - 112 - Middle East 113 - 134 - Ocean Affairs and Climate Change Division 135 - 142 - Overseas Administration Division 143 - 149 - Overseas Sri Lankan Division 151 - 154 - Policy Planning Division 155 - 157 - Protocol Division 159 - 167 - Public Communications Division 169 - 172 - South Asia and SAARC Division 173 - 184 - United Nations and Human Rights Division 185 - 192 - United States of America and Canada Division 193 - 201 - West Division 203 - 229 5. Network of Diplomatic Missions Abroad 231 6. Revenue collected by Sri Lanka Missions Abroad in 2017 233 - 235 7. Consular activities carried out by Sri Lanka Missions Abroad - 236 - 238 2017 Vision To be a responsible nation within the international community and to maintain friendly relations with all countries. Mission The Promotion, Projection and Protection of Sri Lanka’s national interests internationally, in accordance with the foreign policy of the Government and to advise the Government on managing foreign relations in keeping with Sri Lanka’s national interests. Subjects and Functions of the Ministry of Foreign Affairs Implementation of political plans and programmes in respect of Foreign Affairs; Representation of Sri Lanka abroad; International Agreements and Treaties; Foreign Government and international organization’s representation in Sri Lanka; External publicity; Diplomatic immunities and privileges and Consular functions. -

STS Forum 2016 Sri Lanka – Final Report
Science and Technology for Society Forum Sri Lanka 2016 Ministry of Science Technology and Research i Science and Technology for Society Forum Sri Lanka 2016 REPORT SCIENCE AND TECHNOLOGY FOR SOCIETY FORUM SRI LANKA 2016 07 September 2016 NELUM POKUNA MAHINDA RAJAPAKSA THEATRE 08 -10 September 2016 WATERS EDGE Ministry of Science Technology & Research 3rd Floor, Sethsiripaya, Battaramulla Sri Lanka Ministry of Science Technology and Research ii Science and Technology for Society Forum Sri Lanka 2016 ACKNOWLEDGEMENTS We wish to acknowledge Hon. Susil Premajayantha, Minister of Science Technology and Research for his vision in introducing the concept of the STS Forum to Sri Lanka and the leadership given towards executing this very productive Forum. Our sincere thanks and appreciation also goes to him for placing his trust and confidence in Team COSTI for Coordinating the Technical component of this National Forum. Special thanks are due to Hon. Lakshman Senewiratne, State Minister of Science Technology and Research, Ms. R Wijialudchumi, Secretary, Ministry of Science Technology and Research and all other staff members of the Ministry for their unstinted support in organizing the Forum, from the time of planning to the final day of the Forum. We also wish to thank most sincerely members of staff of other S&T Institutions coming under the purview of the Ministry of Science Technology and Research; the NSF, ITI, ACCIMT, SLSI, NRC, SLAB, NASTEC, NERDC, NIFS, Planetarium, SLINTEC and SLIC, who gave their fullest support and coorporation towards the organization of the Forum. We appreciate the generous support given to us by both local and expatriate Sri Lankan scientists and other foreign delegates in making this Forum a success. -

Preferential Votes
DN page 6 SATURDAY, AUGUST 8, 2020 GENERAL ELECTION PREFERENTIAL VOTES Samagi Jana Balawegaya (SJB) Duminda Dissanayake 75,535 COLOMBO DISTRICT H. Nandasena 53,618 Rohini Kumari Kavirathna 27,587 K.P.S Kumarasiri 49,030 Sri Lanka Podujana Peramuna (SLPP) Rajitha Aluvihare 27,171 Wasantha Aluwihare 25,989 Samagi Jana Balawegaya (SJB) Dhaya Nandasiri 17,216 Ibrahim Mohammed Shifnas 13,518 Ishaq Rahman 49,290 Sarath Weerasekara Thissa Bandara Herath 9,224 Rohana Bandara Wijesundara 39,520 328,092 Maithiri Dosan 5,856 Suppaiya Yogaraj 4,900 Wimal Weerawansa 267, 084 DIGAMADULLA DISTRICT Udaya Gammanpila 136, 331 Sri Lanka Podujana Peramuna (SLPP) Wijeyadasa Rajapakshe 120, 626 PUTTALAM DISTRICT Bandula Gunawardena 101, 644 Pradeep Undugoda 91, 958 Sri Lanka Podujana Peramuna (SLPP) Wimalaweera Dissanayake 63,594 Samagi Jana Balawegaya (SJB) Sanath Nishantha Perera Sajith Premadasa 305, 744 80,082 S.M. Marikkar 96,916 D. Weerasinghe 56,006 Mujibur Rahman 87, 589 Thilak Rajapaksha 54,203 Harsha de Silva 82, 845 Piyankara Jayaratne 74,425 Patali Champika Ranawaka 65, 574 Arundika Fernando 70,892 Mano Ganesan 62, 091 Chinthaka Amal Mayadunne 46,058 Samagi Jana Balawegaya (SJB) Ashoka Priyantha 41,612 Mohomed Haris 36,850 Mohomed Faizal 29,423 BADULLA DISTRICT Samagi Jana Balawegaya (SJB) Sri Lanka Podujana Peramuna (SLPP) Hector Appuhamy 34,127 National Congress (NC) Niroshan Perera 31,636 Athaulla Ahamed 35,697 Nimal Siripala de Silva Muslim National Alliance (MNA) All Ceylon Makkal Congress (ACMC) 141, 901 Abdul Ali Sabry 33,509 Mohomed Mushraf -

Minutes of Parliament Present
(Eighth Parliament - First Session) No. 95. ] MINUTES OF PARLIAMENT Friday, August 26, 2016 at 10.30 a. m. PRESENT : Hon. Karu Jayasuriya, Speaker Hon. Thilanga Sumathipala, Deputy Speaker and Chairman of Committees Hon. Selvam Adaikkalanathan, Deputy Chairman of Committees His Excellency Maithripala Sirisena, President of the Democratic Socialist Republic of Sri Lanka, Minister of Defence, Minister of Mahaweli Development and Environment and Minister of National Integration and Reconciliation Hon. Ranil Wickremesinghe, Prime Minister and Minister of National Policies and Economic Affairs Hon. (Mrs.) Thalatha Atukorale, Minister of Foreign Employment Hon. Wajira Abeywardana, Minister of Home Affairs Hon. John Amaratunga, Minister of Tourism Development and Christian Religious Affairs and Minister of Lands Hon. Akila Viraj Kariyawasam, Minister of Education Hon. Lakshman Kiriella, Minister of Higher Education and Highways and the Leader of the House of Parliament Hon. Dayasiri Jayasekara, Minister of Sports Hon. Nimal Siripala de Silva, Minister of Transport and Civil Aviation Hon. Navin Dissanayake, Minister of Plantation Industries Hon. S. B. Dissanayake, Minister of Social Empowerment and Welfare Hon. S. B. Nawinne, Minister of Internal Affairs, Wayamba Development and Cultural Affairs Hon. Gamini Jayawickrama Perera, Minister of Sustainable Development and Wildlife Hon. A. D. Susil Premajayantha, Minister of Science, Technology and Research Hon. R. M. Ranjith Madduma Bandara, Minister of Public Administration and Management Hon. Sagala Ratnayaka, Minister of Law and Order and Southern Development ( 2 ) M. No. 95 Hon. Arjuna Ranatunga, Minister of Ports and Shipping Hon. (Dr.) Wijeyadasa Rajapakshe, Minister of Justice and Minister of Buddhasasana Hon. Chandima Weerakkody, Minister of Petroleum Resources Development Hon. Mahinda Samarasinghe, Minister of Skills Development and Vocational Training Hon. -
Evalcolombo2018
EvalColombo2018 Responsible Parliaments: Embracing Evaluation for Agenda 2030 17 to 19 September 2018 • Colombo, Sri Lanka Report Report compiled by Kieron Crawley Photo credit: EvalColombo2018 EvalColombo2018 Responsible Parliaments: Embracing Evaluation for Agenda 2030 17 to 19 September 2018 • Colombo, Sri Lanka Report Special appreciation to for partnering with and supporting GPFE Acknowledgements EvalColombo2018 Conference Co-chairs The Global Forum for Parliamentarians on Evaluation (GPFE) recognises the significant contribution of the Sri Lankan Government, the Office of the Prime Minister, Parliament of Sri Lanka, Sri Lanka Parliamentarians Forum for Evaluation, UNICEF, Strengthening Democratic Governance and Accountability Project (SDGAP) of USAID, EvalPartners, the World Bank, the Asian Development Bank, Sri Lanka Evaluation Association, development partners and public sector, private sector, multi-lateral, and bi-lateral sponsors in sup- porting EvalColombo2018. Our sincere gratitude to national parliaments who extended great support by sending members to the event. In particular, special thanks go to the following leaders for their excellent leadership and Hon. Kabir Hashim, support to make the event a success: Minister of Highways & Road Development and • His Excellency Maithripala Sirisena, the President of the Democratic Socialist Petroleum Resources Republic of Sri Lanka Development, Sri Lanka and the Chair of the • Hon. Ranil Wickremesinghe, Prime Minister of the Democratic Socialist Republic Global Parliamentarians of Sri Lanka Forum for Evaluation • Hon. Karu Jayasuriya, Speaker of the Parliament of Sri Lanka • Hon. Kabir Hashim, Minister of Highways & Road Development and Petroleum Resources development, Sri Lanka and the Chair of the Global Parliamentarians Forum for Evaluation • Hon. Ananda Kumarasiri, Deputy Speaker of the Parliament of Sri Lanka and the Chair of the Sri Lanka Parliamentarians Forum for Evaluation • Hon. -
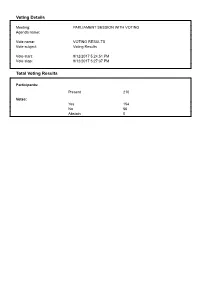
Voting Details Total Voting Results
Voting Details Meeting: PARLIAMENT SESSION WITH VOTING Agenda name: Vote name: VOTING RESULTS Vote subject: Voting Results Vote start: 9/12/2017 5:24:51 PM Vote stop: 9/12/2017 5:27:37 PM Total Voting Results Participants: Present 210 Votes: Yes 154 No 56 Abstain 0 Individual Voting Results GOVERNMENT SIDE G 001. Mangala Samaraweera Yes G 002. S.B. Dissanayake Yes G 003. Nimal Siripala de Silva Yes G 004. Gamini Jayawickrama Perera Yes G 005. John Amaratunga Yes G 006. Lakshman Kiriella Yes G 007. Ranil Wickremesinghe Yes G 009. Gayantha Karunatileka Yes G 010. W.D.J. Senewiratne Yes G 011. Sarath Amunugama Yes G 012. Rauff Hakeem Yes G 013. Rajitha Senaratne Yes G 014. Rishad Bathiudeen Yes G 015. Kabir Hashim Yes G 016. Sajith Premadasa Yes G 017. Malik Samarawickrama Yes G 018. Mano Ganesan Yes G 019. Anura Priyadharshana Yapa Yes G 020. Ven. Athuraliye Rathana Thero Yes G 021. Thilanga Sumathipala Yes G 022. A.D. Susil Premajayantha Yes G 023.Tilak Marapana Yes G 024. Mahinda Samarasinghe Yes G 025. Wajira Abeywardana Yes G 026. S.B. Nawinne Yes G 028. Patali Champika Ranawaka Yes G 029. Mahinda Amaraweera Yes G 030. Navin Dissanayake Yes G 031. Ranjith Siyambalapitiya Yes G 032. Duminda Dissanayake Yes G 033. Wijith Wijayamuni Zoysa Yes G 034. P. Harrison Yes G 035. R.M. Ranjith Madduma Bandara Yes G 036. Arjuna Ranatunga Yes G 037. Palany Thigambaram Yes G 038. Chandrani Bandara Yes G 039. Thalatha Atukorale Yes G 040. Akila Viraj Kariyawasam Yes G 041. -

Select Committee Report
PARLIAMENTARY SERIES NO. 281 OF The Seventh Parliament of the Democratic Socialist Republic of Sri Lanka (First Session) REPORT OF SELECT COMMITTEE OF PARLIAMENT TO DISCUSS THE HEADS OF EXPENDITURE OF MINISTRIES SELECTED FROM THE BUDGET ESTIMATES OF 2014 Presented by Hon. Nimal Siripala de Silva Chairman of the Committee Ordered by the Parliament of Sri Lanka to be printed on 14 December 2013 PRINTED AT THE DEPARTMENT OF GOVERNMENT PRINTING, SRI LANKA TO BE PURCHASED AT THE GOVERNMENT PUBLICATIONS BUREAU, COLOMBO Select Committee to discuss the Heads of Expenditure of Ministries selected from the Budget Estimates of 2014 Committee: Hon. Nimal Siripala de Silva (Chairman) Hon. W. D. J. Senewiratne Hon. (Dr.) Sarath Amunugama Hon. Dinesh Gunawardena Hon. Rauf Hakeem Hon. Athauda Seneviratne Hon. Chandrasiri Gajadeera Hon. Muthu Sivalingam Hon. Lasantha Alagiyawanna Hon. M. Joseph Michael Perera Hon. John Amaratunga Hon. Sunil Handunnetti Hon. Suresh K. Premachandran Hon. Pon. Selvarasa Hon. R. Yogarajan Hon. Akila Viraj Kariyawasam Hon. Silvastrie Alantin Hon. (Dr.) Harsha De Silva Hon. (Dr.) (Mrs.) Sudarshini Fernandopulle Hon. (Mrs.) Rosy Senanayake Hon. Hunais Farook ( 2 ) REPORT The following motion moved by the Leader of the House of Parliament on 22 November 2013 was approved by the House. The Leader of the House of Parliament,— Select Committee of Parliament to discuss the Heads of Expenditure of the Ministries selected from the Budget Estimates of the year 2014,— Whereas the period of time allocated to the Committee stage programme