Recurrent Massive Upper Gastrointestinal Bleeding - Complication of Cystogastrostomy for Pancreatic Pseudocyst Following Blunt Trauma to the Abdomen: a Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Audit on Management of Hematemesis in Children Admitted to Pediatric Gastroenterology and Hepatology Unit of Assiut
Med. J. Cairo Univ., Vol. 86, No. 8, December: 4531-4536, 2018 www.medicaljournalofcairouniversity.net Clinical Audit on Management of Hematemesis in Children Admitted to Pediatric Gastroenterology and Hepatology Unit of Assiut University Children Hospital ESRAA T. AHMED, M.Sc.; FATMA A. ALI, M.D. and NAGLA H. ABU FADDAN, M.D. The Department of Pediatrics, Faculty of Medicine, Assiut University, Assiut, Egypt Abstract Hematemesis: Indicates that the bleeding origin is above the Treitz angle, i.e., that it constitutes an Background: Hematemesis is an uncommon but potentially Upper Gastrointestinal Bleeding (UGIB) [3] . serious and life-threatening clinical condition in children. It indicates that the bleeding origin is above the Treitz angle, The etiology of upper GI bleeding varies by i.e., that it constitutes an Upper Gastrointestinal Bleeding (UGIB). age. The pathophysiology of upper GI bleeding is related to the source of the bleeding. Most clinically Aim of Study: To assess for how much the adopted proto- significant causes of upper GI bleeds are associated cols of management of children with upper gastrointestinal bleeding were applied at Gastroenterology & Hepatology Unit with ulcers, erosive esophagitis, gastritis, varices, of Assiut University Children Hospital. and/or Mallory-Weiss tears. While Physiologic Patients and Methods: This study is a an audit on man- stress, NSAIDs such as aspirin and ibuprofen, and agement of children with upper gastrointestinal bleeding infection with Helicobacter pylori are few of the admitted to pediatric Gastroenterology and Hepatology Unit, factors contributing to the imbalance leading to Assiut University Children Hospital during the period from ulcers and erosions in the GI tract [4] . -

Hemosuccus Pancreaticus: a Rare Cause of Upper Gastrointestinal Bleeding During Pregnancy Rani Akhil Bhat,1 Vani Ramkumar,1 K
Hemosuccus Pancreaticus: A Rare Cause Of Upper Gastrointestinal Bleeding During Pregnancy Rani Akhil Bhat,1 Vani Ramkumar,1 K. Akhil Krishnanand Bhat, 2 Rajgopal Shenoy2 Abstract Upper gastrointestinal bleeding is most commonly caused by From the 1Department of Department of Obstetrics and Gynaecology, Oman Medical 2 lesions in the esophagus, stomach or duodenum. Bleeding which College, Sohar, Sultanate of Oman, Department of Surgery, Oman Medical College, Sohar, Sultanate of Oma. originates from the pancreatic duct is known as hemosuccus pancreaticus. Only a few scattered case reports of hemosuccus Received: 06 Nov 2009 pancreaticus during pregnancy have been recorded in literature. Accepted: 31 Dec 2009 This is a case of a primigravida with 37 weeks of gestation Address correspondence and reprint request to: Dr. Rani A. Bhat,Department of with hemosuccus pancreaticus and silent chronic pancreatitis. Obstetrics and Gynaecology, Oman Medical College, P. O. Box 391, P. C. 321, Al- Evaluating pregnant women with upper gastrointestinal Tareef, Sohar, Sultanate of Oman. bleeding differs from that of non pregnant women as diagnostic E-mail: [email protected] modalities using radiation cannot be used. Therefore, Esophagogastroduodenoscopy should be performed at the time of active bleeding to diagnose hemosuccus pancreaticus. Bhat RA, et al. OMJ. 25 (2010); doi:10.5001/omj.2010.21 Introduction examination showed a combination of dark red blood and melena. Laboratory investigations revealed hemoglobin of 6.3 grams/dL, Hemosuccus pancreaticus is the term used to describe the liver function tests, serum amylase, glucose and prothrombin time syndrome of gastrointestinal bleeding into the pancreatic duct were within the normal range. -

Non-Alcoholic Steatohepatitis (NASH) in Non-Obese Children
Tropical Gastroenterology 2016;37(2):133-135 133 collection then follow the path along the lesser omentum References or gastrohepatic ligament toward the liver leading to the formation of left lobe subcapsular collections. Second 1. Mofredj A, Cadranel JF, Dautreaux Met al. Pancreatic mechanism, likely in our second case, is tracking of pseudocyst located in the liver: a case report and literature review. J Clin Gastroenterol. 2000;30:813. pancreatic juice along the hepatoduodenal ligament 2. Okuda K, Sugita S, Tsukada E, Sakuma Yet al. Pancreatic from the head of pancreas to the portahepatis resulting pseudocyst in the left hepatic lobe: a report of two cases. in formation of intrahepatic parenchymal collections. Hepatology. 1991;13:359-63. Pseudocysts, which form as per the first mechanism, 3. Kralik J, Pesula E. A pancreatic pseudocyst in the liver. are mainly subcapsular in location and are biconvex in Rozhl Chir. 1993;72:913. shape. Intra parenchymal pseudocysts formed as a result 4. Bhasin DK, Rana SS, Chandail VS et al. An intrahepatic pancreatic pseudocyst successfully treated endoscopic of the second mechanism are located away from the liver transpapillary drainage alone. JOP. 2005;6:5937. capsule and are located near branches of porta hepatis. 5. Atia A, Kalra S, Rogers M et al. A wayward cyst. JOP. J Intrahepatic pseudocysts pose a diagnostic challenge Pancreas (Online) 2009;10:4214. because they are rarely considered in the differential diagnosis of cystic hepatic lesions. Amylase rich fluid on aspiration and communication of pseudocyst with disrupted pancreatic duct on imaging is indicative of diagnosis. However, neither of pseudocysts in our two Non-alcoholic steatohepatitis cases had communication with pancreatic duct. -

Case Report: a Patient with Severe Peritonitis
Malawi Medical Journal; 25(3): 86-87 September 2013 Severe Peritonitis 86 Case Report: A patient with severe peritonitis J C Samuel1*, E K Ludzu2, B A Cairns1, What is the likely diagnosis? 2 1 What may explain the small white nodules on the C Varela , and A G Charles transverse mesocolon? 1 Department of Surgery, University of North Carolina, Chapel Hill NC USA 2 Department of Surgery, Kamuzu Central Hospital, Lilongwe Malawi Corresponding author: [email protected] 4011 Burnett Womack Figure1. Intraoperative photograph showing the transverse mesolon Bldg CB 7228, Chapel Hill NC 27599 (1a) and the pancreas (1b). Presentation of the case A 42 year-old male presented to Kamuzu Central Hospital for evaluation of worsening abdominal pain, nausea and vomiting starting 3 days prior to presentation. On admission, his history was remarkable for four similar prior episodes over the previous five years that lasted between 3 and 5 days. He denied any constipation, obstipation or associated hematemesis, fevers, chills or urinary symptoms. During the first episode five years ago, he was evaluated at an outlying health centre and diagnosed with peptic ulcer disease and was managed with omeprazole intermittently . His past medical and surgical history was non contributory and he had no allergies and he denied alcohol intake or tobacco use. His HIV serostatus was negative approximately one year prior to presentation. On examination he was afebrile, with a heart rate of 120 (Fig 1B) beats/min, blood pressure 135/78 mmHg and respiratory rate of 22/min. Abdominal examination revealed mild distension with generalized guarding and marked rebound tenderness in the epigastrium. -

Esophageal Varices
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Crossref Hindawi Publishing Corporation Case Reports in Critical Care Volume 2016, Article ID 2370109, 4 pages http://dx.doi.org/10.1155/2016/2370109 Case Report A Rare but Reversible Cause of Hematemesis: (Downhill) Esophageal Varices Lam-Phuong Nguyen,1,2,3 Narin Sriratanaviriyakul,1,2,3 and Christian Sandrock1,2,3 1 Division of Pulmonary, Critical Care, and Sleep Medicine, University of California, Davis, Suite #3400, 4150 V Street, Sacramento, CA 95817, USA 2Department of Internal Medicine, University of California, Davis, Sacramento, USA 3VA Northern California Health Care System, Mather, USA Correspondence should be addressed to Lam-Phuong Nguyen; [email protected] Received 12 December 2015; Accepted 1 February 2016 Academic Editor: Kurt Lenz Copyright © 2016 Lam-Phuong Nguyen et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. “Downhill” varices are a rare cause of acute upper gastrointestinal bleeding and are generally due to obstruction of the superior vena cava (SVC). Often these cases of “downhill” varices are missed diagnoses as portal hypertension but fail to improve with medical treatment to reduce portal pressure. We report a similar case where recurrent variceal bleeding was initially diagnosed as portal hypertension but later found to have SVC thrombosis presenting with recurrent hematemesis. A 39-year-old female with history of end-stage renal disease presented with recurrent hematemesis. Esophagogastroduodenoscopy (EGD) revealed multiple varices. -

Intrahepatic Pancreatic Pseudocyst: Case Series
JOP. J Pancreas (Online) 2016 Jul 08; 17(4):410-413. CASE SERIES Intrahepatic Pancreatic Pseudocyst: Case Series Dhaval Gupta, Nirav Pipaliya, Nilesh Pandav, Kaivan Shah, Meghraj Ingle, Prabha Sawant Department of Gastroenterology, Lokmanya Tilak Municipal Medical College &Hospital, Sion, Mumbai, India ABSTRACT Intrahepatic pseudocyst is a very rare complication of pancreatitis. Lack of experience and literature makes diagnosis and management of intrahepatic pseudocyst very difficult. Majority of published cases were managed by either percutaneous or surgical drainage. Less than 30 cases of intrahepatic pseudocysts have been reported in the literature and there is not a single report of endoscopic ultrasound guided management of intrahepatic pseudocysts. Here we report a case series of 2 patients who presented with intrahepatic pseudocysts and out of which first case was successfully managed by EUS guided drainage. Our second case is also the youngest patient presented with intrahepatic pseudocyst till now. INTRODUCTION abdominal distention since last 1 month. However he did located in or around t not have significant weight loss, gastrointestinal bleeding, A pancreatic pseudocyst is a collection of pancreatic fluid pedal edema, jaundice, fever. His past medical history and he pancreas. Pancreatic pseudocysts family history was not significant. He was chronic alcoholic are encased by a non-epithelial lining of fibrous, necrotic since last 15 years with intake of approximately 90 gram and granulation tissue secondary to pancreatic injury. -
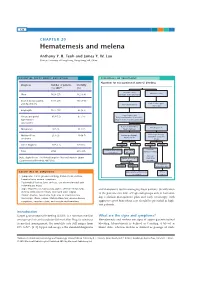
Hematemesis and Melena Chapter
126 CHAPTER 20 Hematemesis and melena Anthony Y. B. Teoh and James Y. W. Lau Chinese University of Hong Kong, Hong Kong SAR, China ESSENTIAL FACTS ABOUT CAUSATION ESSENTIALS OF TREATMENT Algorithm for management of acute GI bleeding Diagnosis Number of patients Mortality (%) 200716 (%) Major bleeding Minor bleeding Ulcer 1826 (27) 162 (8.9) (unstable hemodynamics) Erosive disease (gastric 1731 (26) 195 (14.1) Early elective upper and duodenum) Active resuscitation endoscopy Esophagitis 1177 (17) 65 (5.5) Urgent endoscopy Varices and portal 819 (12) 87 (14) Early administration of vasoactive hypertensive drugs in suspected variceal bleeding gastropathy Active ulcer bleeding Bleeding varices Malignancy 187 (3) 31 (17) Major stigmata Mallory-Weiss 213 (3) 10 (4.7) Endoscopic therapy Endoscopic therapy Adjunctive PPI Adjunctive vasoactive syndrome drugs Other diagnosis 797 (12) 125 (16) Success Failure Success Failure Continue Continue ulcer healing Recurrent Total 6750 675 (10) vasoactive drugs medications bleeding Variceal Data adapted from The United Kingdom National Audit in Upper Repeat endoscopic eradication Gastrointestinal Bleeding 2007 [16]. therapy program Sengstaken- Success Failure Blakemore tube ESSENTIALS OF DIAGNOSIS Angiographic embolization TIPS vs vs. surgery surgery • Symptoms: Coffee ground vomiting, hematemesis, melena, hematochezia, anemic symptoms • Past medical history: Liver cirrhosis, use of non-steroidal anti- inflammatory drugs • Signs: Hypotension, tachycardia, pallor, altered mental status, and therapeutic tool in managing these patients. Stratification melena or blood per rectum, decreased urine output of the patients into low- or high-risk groups aids in formulat- • Bloods: Anemia, raised urea, high urea to creatinine ratio • Endoscopy: Ulcers, varices, Mallory-Weiss tear, erosive disease, ing a clinical management plan and early endoscopy with neoplasms, vascular ectasia, and vascular malformations aggressive post-hemostasis care should be provided in high- risk patients. -

Abdominal Pain
10 Abdominal Pain Adrian Miranda Acute abdominal pain is usually a self-limiting, benign condition that irritation, and lateralizes to one of four quadrants. Because of the is commonly caused by gastroenteritis, constipation, or a viral illness. relative localization of the noxious stimulation to the underlying The challenge is to identify children who require immediate evaluation peritoneum and the more anatomically specific and unilateral inner- for potentially life-threatening conditions. Chronic abdominal pain is vation (peripheral-nonautonomic nerves) of the peritoneum, it is also a common complaint in pediatric practices, as it comprises 2-4% usually easier to identify the precise anatomic location that is produc- of pediatric visits. At least 20% of children seek attention for chronic ing parietal pain (Fig. 10.2). abdominal pain by the age of 15 years. Up to 28% of children complain of abdominal pain at least once per week and only 2% seek medical ACUTE ABDOMINAL PAIN attention. The primary care physician, pediatrician, emergency physi- cian, and surgeon must be able to distinguish serious and potentially The clinician evaluating the child with abdominal pain of acute onset life-threatening diseases from more benign problems (Table 10.1). must decide quickly whether the child has a “surgical abdomen” (a Abdominal pain may be a single acute event (Tables 10.2 and 10.3), a serious medical problem necessitating treatment and admission to the recurring acute problem (as in abdominal migraine), or a chronic hospital) or a process that can be managed on an outpatient basis. problem (Table 10.4). The differential diagnosis is lengthy, differs from Even though surgical diagnoses are fewer than 10% of all causes of that in adults, and varies by age group. -

Esophageal Varices
World Gastroenterology Organisation Global Guidelines Esophageal varices JANUARY 2014 Revision authors Prof. D. LaBrecque (USA) Prof. A.G. Khan (Pakistan) Prof. S.K. Sarin (India) Drs. A.W. Le Mair (Netherlands) Original Review team Prof. D. LaBrecque (Chair, USA) Prof. P. Dite (Co-Chair, Czech Republic) Prof. Michael Fried (Switzerland) Prof. A. Gangl (Austria) Prof. A.G. Khan (Pakistan) Prof. D. Bjorkman (USA) Prof. R. Eliakim (Israel) Prof. R. Bektaeva (Kazakhstan) Prof. S.K. Sarin (India) Prof. S. Fedail (Sudan) Drs. J.H. Krabshuis (France) Drs. A.W. Le Mair (Netherlands) © World Gastroenterology Organisation, 2013 WGO Practice Guideline Esophageal Varices 2 Contents 1 INTRODUCTION ESOPHAGEAL VARICES............................................................. 2 1.1 WGO CASCADES – A RESOURCE -SENSITIVE APPROACH ............................................. 2 1.2 EPIDEMIOLOGY ............................................................................................................ 2 1.3 NATURAL HISTORY ...................................................................................................... 3 1.4 RISK FACTORS .............................................................................................................. 4 2 DIAGNOSIS AND DIFFERENTIAL DIAGNOSIS...................................................... 5 2.1 DIFFERENTIAL DIAGNOSIS OF ESOPHAGEAL VARICES /HEMORRHAGE ......................... 5 2.2 EXAMPLE FROM AFRICA — ESOPHAGEAL VARICES CAUSED BY SCHISTOSOMIASIS .. 6 2.3 OTHER CONSIDERATIONS ............................................................................................ -

ACR Appropriateness Criteria® Nonvariceal Upper Gastrointestinal Bleeding
Revised 2016 American College of Radiology ACR Appropriateness Criteria® Nonvariceal Upper Gastrointestinal Bleeding Variant 1: Endoscopy reveals nonvariceal upper gastrointestinal arterial bleeding source. Radiologic Procedure Rating Comments RRL* Arteriography visceral 9 This procedure is comparable to CTA. ☢☢☢ This procedure is comparable to CTA abdomen with IV contrast 7 arteriography. ☢☢☢ CT enterography 5 ☢☢☢☢ CT abdomen without IV contrast 4 ☢☢☢ CT abdomen with IV contrast 2 ☢☢☢ CT abdomen without and with IV contrast 2 ☢☢☢☢ RBC scan abdomen and pelvis 2 ☢☢☢ X-ray upper GI series 1 ☢☢☢ *Relative Rating Scale: 1,2,3 Usually not appropriate; 4,5,6 May be appropriate; 7,8,9 Usually appropriate Radiation Level Variant 2: Endoscopy confirms nonvariceal upper gastrointestinal bleeding without a clear source. Radiologic Procedure Rating Comments RRL* Arteriography visceral 9 This procedure is comparable to CTA. ☢☢☢ This procedure is comparable to CTA abdomen with IV contrast 8 arteriography. ☢☢☢ CT enterography 5 ☢☢☢☢ RBC scan abdomen and pelvis 5 ☢☢☢ CT abdomen without IV contrast 4 ☢☢☢ CT abdomen with IV contrast 3 ☢☢☢ CT abdomen without and with IV contrast 3 ☢☢☢☢ X-ray upper GI series 1 ☢☢☢ *Relative Rating Scale: 1,2,3 Usually not appropriate; 4,5,6 May be appropriate; 7,8,9 Usually appropriate Radiation Level ACR Appropriateness Criteria® 1 Nonvariceal Upper Gastrointestinal Bleeding Variant 3: Nonvariceal upper gastrointestinal bleeding; negative endoscopy. Radiologic Procedure Rating Comments RRL* This procedure is comparable to CTA and Arteriography visceral 8 CT enterography. ☢☢☢ This procedure is comparable to CTA abdomen with IV contrast 8 arteriography and is an alternative to CT ☢☢☢ enterography. This procedure is comparable to CT enterography 7 arteriography and is an alternative to ☢☢☢☢ CTA. -

Hematemesis Melena Due to Helicobacter Pylori Infection in Duodenal Ulcer: a Case Report and Literature Review
International Journal of Science and Research (IJSR) ISSN (Online): 2319-7064 Index Copernicus Value (2016): 79.57 | Impact Factor (2017): 7.296 Hematemesis Melena due to Helicobacter Pylori Infection In Duodenal Ulcer: A Case Report and Literature Review Ayu Budhi Trisna Dewi Rahayu Sutanto1, I Made Suma Wirawan2 1General Practitioner Wangaya Hospital Denpasar Bali Indonesia 2 Endoscopy Unit of Internal Medicine Wangaya Hospital Denpasar Bali Indoensia Abstract: A Balinese woman, 60 years old complaint of hematemesis and melena. Esophagogastroduodenoscopy performed one day after admission and revealed a soliter ulcer at duodenum bulb. Histopathology examination revealed a spherical like organism suspected Helicobacter pylori (H. pylori) infection. Eradication of H. pylori by triple drug consisting of omeprazole, amoxicillin and chlarythromycin as the standard protocol of eradication within 14 days. Reevaluation by esophagogastroduodenoscopy examination will perform in the next 3 months to evaluate the treatment succesfull. Keywords: peptic ulcer, duodenum, H. pylori 1. Background also normal. The patient diagnosed with hematemesis suspect peptic ulcer. The patient was then admitted to ward Approximately 500,000 persons develop peptic ulcer disease and giving infusion ringer lactat, proton pump inhibitor in the United States each year. in 70 percent of patients it esomeprazole bolus 40 mg intravenous and continuous with occurs between the ages of 25 and 64 years. The annual 8 mg/ hours and planned for esofagogastroduodenoscopy to direct and indirect health care costs of the disease are evaluate the source of hematemesis. estimated at about $10 billion. However, the incidence of peptic ulcers is declining, possibly as a result of the increasing use of proton pump inhibitors and decreasing rates of Helicobacter pylori (H. -

Pancreatic Ascites in a Patient with Cirrhosis and Pancreatic Duct Leak Philip Montemuro, MD Thomas Jefferson University
The Medicine Forum Volume 13 Article 11 2012 Not Your Typical Case Of Ascites: Pancreatic Ascites In A Patient With Cirrhosis And Pancreatic Duct Leak Philip Montemuro, MD Thomas Jefferson University Abhik Roy, MD Thomas Jefferson University Follow this and additional works at: https://jdc.jefferson.edu/tmf Part of the Medicine and Health Sciences Commons Let us know how access to this document benefits ouy Recommended Citation Montemuro, MD, Philip and Roy, MD, Abhik (2012) "Not Your Typical Case Of Ascites: Pancreatic Ascites In A Patient With Cirrhosis And Pancreatic Duct Leak," The Medicine Forum: Vol. 13 , Article 11. DOI: https://doi.org/10.29046/TMF.013.1.012 Available at: https://jdc.jefferson.edu/tmf/vol13/iss1/11 This Article is brought to you for free and open access by the Jefferson Digital Commons. The effeJ rson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The ommonC s is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The effeJ rson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in The eM dicine Forum by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Montemuro, MD and Roy, MD: Not Your Typical Case Of Ascites: Pancreatic Ascites In A Patient With Cirrhosis And Pancreatic Duct Leak The Medicine Forum Not Your Typical Case Of Ascites: Pancreatic Ascites In A Patient With Cirrhosis And Pancreatic Duct Leak Philip Montemuro, MD and Abhik Roy, MD Case A 55-year-old male with a history of hepatic cirrhosis secondary to Hepatitis C and alcohol abuse presented to an outside hospital with progressive abdominal pain and distension.