Accidental Intrarectal Administration of Alcohol Enema Induces Proctocolitis and Fecal Incontinence
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gastroenterology and the Elderly
3 Gastroenterology and the Elderly Thomas W. Sheehy 3.1. Esophagus 3.1.1. Dysphagia Esophageal disorders, such as esophageal motility disorders, infections, tumors, and other diseases, are common in the elderly. In the elderly, dysphagia usually implies organic disease. There are two types: (1) pre-esophageal and (2) esophageal. Both are further subdivided into motor (neuromuscular) or structural (intrinsic and extrinsic) lesions.! 3.1.2. Pre-esophageal Dysphagia Pre-esophageal dysphagia (PED) usually implies neuromuscular disease and may be caused by pseudobular palsy, multiple sclerosis, amy trophic lateral scle rosis, Parkinson's disease, bulbar poliomyelitis, lesions of the glossopharyngeal nerve, myasthenia gravis, and muscular dystrophies. Since PED is due to inability to initiate the swallowing mechanism, food cannot escape from the oropharynx into the esophagus. Such patients usually have more difficulty swallowing liquid THOMAS W. SHEEHY • The University of Alabama in Birmingham, School of Medicine, Department of Medicine; and Medical Services, Veterans Administration Medical Center, Birming ham, Alabama 35233. 87 S. R. Gambert (ed.), Contemporary Geriatric Medicine © Plenum Publishing Corporation 1983 88 THOMAS W. SHEEHY than solids. They sputter or cough during attempts to swallow and often have nasal regurgitation or aspiration of food. 3.1.3. Dysfunction of the Cricopharyngeus Muscle In the elderly, this is one of the more common forms of PED.2 These patients have the sensation of an obstruction in their throat when they attempt to swallow. This is due to incoordination of the cricopharyngeus muscle. When this muscle fails to relax quickly enough during swallowing, food cannot pass freely into the esophagus. If the muscle relaxes promptly but closes too quickly, food is trapped as it attempts to enter the esophagus. -

CDHO Factsheet Ulcerative Colitis
Disease/Medical Condition ULCERATIVE COLITIS Date of Publication: June 14, 2013 (also referred to as “UC”, “idiopathic proctocolitis”, “pancolitis”, and “inflammatory bowel disease” [IBD]; IBD is an umbrella term that also includes Crohn’s disease and indeterminate/undifferentiated IBD) Is the initiation of non-invasive dental hygiene procedures* contra-indicated? No Is medical consult advised? ...................................... No (assuming patient/client is already under medical care for ulcerative colitis). Is the initiation of invasive dental hygiene procedures contra-indicated?** Possibly, but not typically Is medical consult advised? ....................................... Possibly (depends on severity and level of control of the disease, including the presence/absence of oral lesions). Is medical clearance required? .................................. Possibly (e.g., if the disease is unstable — flare-up — and/or there are active oral lesions). Also, medical clearance may be required if patient/client is being treated with medications associated with immunosuppression +/- increased risk of infection (e.g., corticosteroids [e.g., prednisone], azathioprine, 6-mercaptopurine, methotrexate, cyclosporine, sulfasalazine, biologic response modifier drugs [e.g., anti-tumour necrosis factor drugs — anti-TNFs — such as infliximab, adalimumab, certoluzimab, and golimumab, as well as monoclonal antibody drugs such as vedoluzimab], JAK1 inhibitors [e.g., tofacitinib], etc.). Is antibiotic prophylaxis required? ............................. -

Advice Note: Infant Proctocolitis – Fresh Blood PR in a Thriving Infant
Advice Note: Infant proctocolitis – Fresh blood PR in a thriving infant Dear GP, Thank you for your referral. The most common cause for small amounts of fresh blood PR in a well, thriving infant is infant proctocolitis. This is a benign condition in vast majority of cases and does not require a secondary care input. This is a food protein related reaction most commonly caused by cow’s milk protein (CMP) but other common causes include soy, egg, corn and cereal grains. Rarely other foods can trigger a reaction. Typically infants can tolerate the previously causative proteins by 1 year of age. It does not increase the risk of IgE mediated food allergy. It is common in both breast and formula fed babies. There are no diagnostic tests and the diagnosis relies on exclusion of other causes and resolution of symptoms with dietary manipulations. Features of a typical presentation include: Mucousy loose stools with spots or streaks of bright red blood in a well thriving infant Age at presentation: 1 week to 5 months (although can present earlier and later) It can be associated with mild to moderate diarrhea, excessive crying / fussiness/ sleep disturbance, apparent pain on defecation. It may also be associated with mild anemia, hypoalbuminaemia, mild peripheral eosinophilia and family history of same. Features indicating other disorders include: No IM vitamin K at birth Severe bleeding Abdominal distension / tenderness on examination Faltering growth Signs / symptoms of malabsorption Severe diarrhea Vomiting Anaphylaxis Rash, including petechiae, purpura or urticarial Significant anaemia Persistent perianal dermatitis Anal fissures Management: Referral to ED if the infant : o is unwell and or febrile o is haemodynamically unstable o has a history of severe bleeding o has significant vomiting o has abdominal distension or tenderness on examination o has features of anaphylaxis o has severe anaemia Management in the community if the child is well and there are no worrying features on history or examination: o Investigations: . -
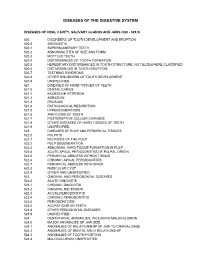
Diagnostic Codes
DISEASES OF THE DIGESTIVE SYSTEM DISEASES OF ORAL CAVITY, SALIVARY GLANDS AND JAWS (520 - 529.9) 520 DISORDERS OF TOOTH DEVELOPMENT AND ERUPTION 520.0 ANODONTIA 520.1 SUPERNUMERARY TEETH 520.2 ABNORMALITIES OF SIZE AND FORM 520.3 MOTTLED TEETH 520.4 DISTURBANCES OF TOOTH FORMATION 520.5 HEREDITARY DISTURBANCES IN TOOTH STRUCTURE, NOT ELSEWHERE CLASSIFIED 520.6 DISTURBANCES IN TOOTH ERUPTION 520.7 TEETHING SYNDROME 520.8 OTHER DISORDERS OF TOOTH DEVELOPMENT 520.9 UNSPECIFIED 521 DISEASES OF HARD TISSUES OF TEETH 521.0 DENTAL CARIES 521.1 EXCESSIVE ATTRITION 521.2 ABRASION 521.3 EROSION 521.4 PATHOLOGICAL RESORPTION 521.5 HYPERCEMENTOSIS 521.6 ANKYLOSIS OF TEETH 521.7 POSTERUPTIVE COLOUR CHANGES 521.8 OTHER DISEASES OF HARD TISSUES OF TEETH 521.9 UNSPECIFIED 522 DISEASES OF PULP AND PERIAPICAL TISSUES 522.0 PULPITIS 522.1 NECROSIS OF THE PULP 522.2 PULP DEGENERATION 522.3 ABNORMAL HARD TISSUE FORMATION IN PULP 522.4 ACUTE APICAL PERIODONTITIS OF PULPAL ORIGIN 522.5 PERIAPICAL ABSCESS WITHOUT SINUS 522.6 CHRONIC APICAL PERIODONTITIS 522.7 PERIAPICAL ABSCESS WITH SINUS 522.8 RADICULAR CYST 522.9 OTHER AND UNSPECIFIED 523 GINGIVAL AND PERIODONTAL DISEASES 523.0 ACUTE GINGIVITIS 523.1 CHRONIC GINGIVITIS 523.2 GINGIVAL RECESSION 523.3 ACUTE PERIODONTITIS 523.4 CHRONIC PERIODONTITIS 523.5 PERIODONTOSIS 523.6 ACCRETIONS ON TEETH 523.8 OTHER PERIODONTAL DISEASES 523.9 UNSPECIFIED 524 DENTOFACIAL ANOMALIES, INCLUDING MALOCCLUSION 524.0 MAJOR ANOMALIES OF JAW SIZE 524.1 ANOMALIES OF RELATIONSHIP OF JAW TO CRANIAL BASE 524.2 ANOMALIES OF DENTAL ARCH -

The British Society of Gastroenterology
Gut: first published as 10.1136/gut.16.10.821 on 1 October 1975. Downloaded from Gut, 1975, 16, 821-845 The British Society of Gastroenterology The 36th annual meeting was held in Oxford on 25-27 September under the Presidency of Dr S. C. Truelove. The meeting proper was preceded by a teaching day on 24 September when there were two sessions, one on liver disease (Chairman: Dr J. Badenoch), and the other on gastrointestinal disorders (Chairman: Sir Francis Avery Jones). There were 14 sessions each allocated to a different subject, and in addition there was a plenary session and panel discussion on 'The management of ulcerative colitis'. The Sir Arthur Hurst Memorial Lecture, 'Towards an artificial liver', was given on this occasion by Dr Roger Williams. Abstracts of the scientific papers follow and a more general report of the meeting and of the social events can be found on page 846. Distribution of gut hormones monkeys though some variation in total influx mechanism is inhibited by cAMP, amount was seen due to different organ this model also satisfies the paradoxical S. R. BLOOM, M. G. BRYANT, AND J. M. weights. Immunocytochemical data on effect of bile acids in congenital chlor- POLAK (Departments of Medicine and hormone distribution were in substantial idorrhoea. Subsequently, a clinical trial Histochemistry, The Royal Postgraduate agreement. was done. Following oral administration Medical School, Hammersmith Hospital, These hormone maps provide baseline of coated theophylline the frequency and London) Although several new gut hor- data for physiological studies. the volume of the diarrhoeas decreased mones have recently been described there significantly. -

Accidental Intrarectal Administration of Alcohol Enema Induces Proctocolitis and Fecal Incontinence
UCTN nnnnnnnnnnnnnnnnnnnnnnnnnn Unusual Cases and Technical Notes 641 Accidental Intrarectal Administration of Alcohol Enema Induces Proctocolitis and Fecal Incontinence At 2 hours before an elective colonoscopy indicated for abdominal pain in a 67-year- old woman, the patients sister wrongly administered 250 cm3 of ªcleansing ene- maº containing ethyl alcohol 96%. The patient experienced a perineal and anorec- tal burning pain, severe abdominal pain, profuse and involuntary diarrhea, tenes- mus, rectal bleeding, and the emission of numerous white plaques mixed with and all over the liquid feces. We diagnosed a Figure 1 Colonoscopy revealed confluent Figure 2 Proximal rectal mucosa showed a white plaques adherent to underlying distal rectal severe erythema and mucosal denudation, prob- severe colonic mucosal sloughing with a mucosa and covering partially the anal canal and ably as a result of the rectal bleeding and the possible secondary perforation. A conser- perianal epidermis. The fecal incontinence was detachment of fibrin white plaques overlying a vative treatment was prescribed of intrave- extremely severe, and occurring when the pa- few hours before nous fluids and electrolytes, and intrave- tient was upright nous cefotaxime, metronidazole, and anal- gesics. We had no evidence-based reasons cleansing enema. We think endoscopic 3 Herrerias JM, Muniain MA, Sanchez S, to prescribe her steroids, so we treated our follow-up should not take place until at Garrido M. Alcohol-induced colitis. En- patients acute proctocolitis as an ischemic least 3 weeks after alcohol instillation, as a doscopy 1983; 15: 121±122 colitis. perforation could occur if a colonoscopy is 4 Bhalotra R. Alcohol-induced proctitis in done with normal insufflation. -

Allergic Proctocolitis in the Exclusively Breastfed Infant
BREASTFEEDING MEDICINE Volume 6, Number 6, 2011 ABM Protocol ª Mary Ann Liebert, Inc. DOI: 10.1089/bfm.2011.9977 ABM Clinical Protocol #24: Allergic Proctocolitis in the Exclusively Breastfed Infant The Academy of Breastfeeding Medicine A central goal of The Academy of Breastfeeding Medicine is the development of clinical protocols for managing common medical problems that may impact breastfeeding success. These protocols serve only as guidelines for the care of breast- feeding mothers and infants and do not delineate an exclusive course of treatment or serve as standards of medical care. Variations in treatment may be appropriate according to the needs of an individual patient. These guidelines are not intended to be all-inclusive, but to provide a basic framework for physician education regarding breastfeeding. Purpose data indicate approximately 0.5–1% of exclusively breastfed infants develop allergic reactions to cow’s milk proteins ex- he purpose of this clinical protocol is to explore the creted in the mother’s milk.5 Given that cow’s milk protein is Tscientific basis, pathologic aspects, and clinical manage- the offending antigen in 50–65% of cases,4,6 the total incidence ment of allergic proctocolitis in the breastfed infant as we of food allergy in the exclusively breastfed infant appears currently understand the condition and to define needs for slightly higher than 0.5–1%. Comparatively, infants fed further research in this area. Although there can be a variety of human milk appear to have a lower incidence of allergic re- allergic responses to given foods, this protocol will focus on actions to cow’s milk protein than those fed cow’s milk–based those that occur in the gastrointestinal tract of the breastfed formula.7 This may be attributable to the relatively low infant, specifically allergic proctocolitis. -

Osseous Metaplasia of the Gallbladder: Report of Two Cases
DOI: 10.14744/ejmo.2017.32042 EJMO 2017;1(2):108–110 Case Report Osseous Metaplasia of the Gallbladder: Report of Two Cases Semra Dogan,1 Asiye Safak Bulut2 1Department of General Surgery, TOBB University of Economics and Technology Faculty of Medicine, Ankara, Turkey 2Department of Pathology, TOBB University of Economics and Technology Faculty of Medicine, Ankara, Turkey Abstract Osseous metaplasia is rarely seen in the gastrointestinal tract. Its occurrence in the gallbladder is even more rare; only 7 cases have been reported thus far. Two additional cases are described herein: one was an incidental finding and the other simulated an intramural gallstone in a chronically inflamed, calculi-containing gallbladder. The patients were a 32-year-old man and a 52-year-old man who presented with abdominal pain. Ultrasonography revealed small gall- stones in 1 patient. Laparoscopic cholecystectomies were performed and histologies were consistent with chronic cholecystitis and cholelithiasis with intramucosal bone formations. One of the patients also had an adenomyoma in the fundus. Osseous metaplasia of the gallbladder is a rare event. It is mostly incidental and although its etiology and clinical significance are unknown, it may mimic a gallstone, which could affect treatment options. The pathogenesis could be osteogenic stimulation as a result of the inflammatory process. Keywords: Bone metaplasia, gallbladder, heterotopic bone, heterotopic ossification, osseous metaplasia Cite This Article: Dogan S, Bulut A. Osseous Metaplasia of the Gallbladder: Report of Two Cases. EJMO. 2017; 1(2): 108-110 sseous metaplasia, which is also known as heterotop- Case Report ic bone, heterotopic ossification, bone metaplasia, is O Case 1 rarely reported in gallbladder and its clinical significance is A 37-year-old male presented to the department of inter- unknown. -

Schistosoma Mansoni Proctocolitis with Polyposis
CASE REPORT Schistosoma Mansoni Proctocolitis with Polyposis Fridah Bosire, Ian Orwa, Michael Mwachiro, Robert Parker, Russell White Tenwek Hospital Correspondence to: Dr. Fridah Bosire, P.O. Box 39 Bomet, Kenya. Email: [email protected] Summary mansoni. He was successfully managed with medical Schistosoma proctocolitis is a rare disease entity, with therapy. limited literature on its occurrence. We report the case of a 17 year old male from an endemic area around Key words: Schistosomiasis, Helminthiasis, Neglected Lake Victoria, Western Kenya, where detailed disease Diseases, Colonoscopy, Colonic Polyps mapping of Schistosomiasis has been carried out. The Ann Afr Surg. 2018; 15(2):81-85 DOI: http://dx.doi.org/10.4314/aas.v15i2.11 patient presented with a seven year history of a © 2018 Author. This work is licensed under the protruding rectal mass and occasional hematochezia. Creative Commons Attribution 4.0 International Colonoscopy revealed multiple polyps involving the License. entire colon to the anus, and pathology showed Conflicts of Interest: None inflammatory polyps secondary to Schistosoma Funding: None Introduction Schistosomiasis or Bilharziasis is a chronic infection schistosomiasis, but only 1 million people were treated caused by blood flukes. This parasitic disease in 2013. This makes up only 15% of the population in constitutes significant public health challenges, and is need. School-age children make up nearly half of the associated with great morbidity and mortality with infected population in Kenya. millions of people being affected worldwide. Globally, Schistosomiasis frequently impacts impoverished rural at least 230 million people are infected (1, 2, 14). communities near fresh water bodies, with poor hygiene According to a World Health Organization (WHO) standards (2, 12). -

Sexually Transmitted Diseases Treatment Guidelines, 2015
Morbidity and Mortality Weekly Report Recommendations and Reports / Vol. 64 / No. 3 June 5, 2015 Sexually Transmitted Diseases Treatment Guidelines, 2015 U.S. Department of Health and Human Services Centers for Disease Control and Prevention Recommendations and Reports CONTENTS CONTENTS (Continued) Introduction ............................................................................................................1 Gonococcal Infections ...................................................................................... 60 Methods ....................................................................................................................1 Diseases Characterized by Vaginal Discharge .......................................... 69 Clinical Prevention Guidance ............................................................................2 Bacterial Vaginosis .......................................................................................... 69 Special Populations ..............................................................................................9 Trichomoniasis ................................................................................................. 72 Emerging Issues .................................................................................................. 17 Vulvovaginal Candidiasis ............................................................................. 75 Hepatitis C ......................................................................................................... 17 Pelvic Inflammatory -

EN GAST IND.Pdf
EN_GAST_IND.QXD 08/31/2005 11:31 AM Page 825 Index The bold letter t or f following a page reference indicates that the information appears on that page only in a table or figure, respectively. abdomen: examination of, 41–8; regions, 43f acetylcholine, 145, 190t abdominal aortic reconstruction, 275t acetyl-CoA, 53 abdominal mass: about, 37–40; with colon N-acetylcysteine, 582 cancer, 365t; and constipation, 386; with achalasia, 118f; about, 121–2; Crohn’s disease, 314, 342t; with cystic cricopharyngeal, 117t, 118; esophageal, fibrosis, 456; GI tract, 307, 373, 375, 379; 6–8, 14, 96, 118f, 120f; and gas, 14; and with hepatocellular carcinoma, 647; in Hirschsprung’s disease, 388; vigorous, pancreas, 434, 445; with ulcerative colitis, 121–2 342t achlorhydria, 57t, 217, 245t, 451 abetalipoproteinemia, 194, 201t acid perfusion test, 98, 106t abscesses: amebic, 392; anorectal, 397, 399, acid suppressants, 145 406–7; appendiceal, 320t; colonic, 391; acidosis: children, 687t, 689, 698, 715, 727t, crypt, 285, 331, 332f; diverticuler, 253; 729; cirrhosis, 571, 591; ischemia, 253, and diverticulitis, 373; eosinophilic, 114; 266; liver transplantation, 641; pancreatitis, horseshoe, 406; liver, 474; lung, 113; 433t; ulcerative colitis, 335 pancreatic, 434; pararectal, 316t; perianal, acids (chemicals), 115 344t acinar cells, 56, 418–19, 422 absorption: of carbohydrates, 194–9, 227–8; acquired immunodeficiency syndrome. see in colon, 360, 362–4; of electrolytes, AIDS 185–92, 333; of fat, 192–4; of glucose, acrodermatitis enteropathica, 205t 194f; principles of, 178; of protein, actinomycosis, 149 199–202; of vitamins and minerals, acute abdomen, 24–7 178–83; of water, 183–5, 360 acute mesenteric ischemia, 252–4 acanthosis, glycogen, esophageal, 126t acyclovir, 294t, 301, 653 acanthosis nigricans, 126 acyclovir treatment, 114 ACE inhibitors. -

Abdominal Pain - Enterocolitis and Genito-Urinary Etiologies
ACS/ASE Medical Student Core Curriculum Abdominal Pain - Enterocolitis and Genito-Urinary Etiologies ABDOMINAL PAIN - ENTEROCOLITIS AND GENITO-URINARY ETIOLOGIES ENTEROCOLITIS Diarrhea is the characteristic feature of enterocolitis, and can be related to several causes. Infectious (bacterial or viral), radiation-induced, and chemotherapy-associated enterocolitis are all possible. The cause, and, therefore, the treatment, is largely based upon obtaining a detailed patient history. Onset and duration of diarrhea, vomiting, fever or abdominal pain, as well as prior exposure to particular food sources, water, animals, and travel abroad are all keys to narrowing the differential diagnosis. Physical examination may reveal abdominal tenderness and distension, borborygmus (a rumbling or gurgling noise made by the movement of fluid and gas in the intestines), and signs of dehydration. In patients with profuse diarrhea, perianal skin breakdown may occur. In patients with severe or prolonged symptoms, work-up is required. This typically begins with basic laboratory tests to determine if electrolyte abnormalities exist. Additionally, stool studies are frequently performed. Clostridium difficile infection is common in geriatric and institutionalized patients, and specific testing should be considered for select patients. Stool cultures may provide diagnostic benefit in order to determine infectious causes, and aid in treatment decisions. Plain abdominal radiographs are less useful than computed tomography (CT) scanning. Many patients will have abdominal distension and bowel dilation, and, therefore, plain film evaluation has limited diagnostic capability. CT images may show specific segments of inflammation, along with more detailed information regarding potential need for surgery, such as pneumatosis or small amounts of free intraperitoneal air. Approximately 10% of patients with enterocolitis will present with symptoms requiring medical evaluation.