Annual Report, 2017-2018
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Proposed Emergency Health Services and Community Paramedicine Legislation
PROPOSED EMERGENCY HEALTH SERVICES AND COMMUNITY PARAMEDICINE LEGISLATION Discussion Guide 1 Introduction The Department of Health and Community Services is in the process of drafting legislation to govern the Provincial Road Ambulance Program (the program). Input from stakeholders and the public is an essential element in drafting this legislation as it will ensure it meets the needs of the ambulance industry and residents of the province. This document provides a brief overview of the program and the components that are being considered for inclusion in the new legislation. The document includes six areas for consideration, including the current state and changes being proposed. As we are inviting feedback, each section also includes specific questions and spaces for a response. There is also an opportunity for respondents to indicate any additional feedback at the end of the document. A glossary of terms used in this document can be found in Annex 1. Background Newfoundland and Labrador is the only jurisdiction in Canada without legislation governing the delivery of ambulance services. In 2012, the Department engaged an external consultant, Fitch and Associates, to conduct a review of the program, which involved stakeholder consultations both during and following the review. In the 2013 report, Fitch indicated numerous issues with the program, among them, a lack of consolidated legislation. Fitch expressed concern that multiple pieces of legislation and multiple organizations were responsible for different elements of the program. Fitch made 10 recommendations to government to transform the program into an efficient and effective ambulance service. One of the key recommendations was the development of dedicated emergency medical services legislation, so that one organization has the responsibility for ambulance service delivery and the authority to make changes necessary to improve the program. -

August 10, 2016 8701 Arliss Street Building Explosion And
8701 Arliss Street August 10, 2016 Post Incident Analysis Montgomery County Fire & Rescue Service POST INCIDENT ANALYSIS 8701 Arliss Street Silver Spring, MD 20910 August 10, 2016 Submitted by: Battalion Chief Tracy McDonald Battalion 1, C Shift Contributors Battalion Chief Mike Leigh Captain Jason Masters Lieutenant Jason Smith Lieutenant Shawn Goodbrod 1 8701 Arliss Street August 10, 2016 Post Incident Analysis Table of Contents TABLE OF CONTENTS ....................................................................................................................... 2 INTRODUCTION ............................................................................................................................... 4 BUILDING STRUCTURE / SITE LAYOUT .............................................................................................. 6 FIREGROUND OPERATIONS .............................................................................................................. 8 Overview .................................................................................................................................................. 8 Operations ............................................................................................................................................... 8 Initial EMS Operations ........................................................................................................................... 14 Command Team Operations ................................................................................................................. -

Critical Care Transport in the Time of COVID-19
ORNGE SUPPLEMENT Critical care transport in the time of COVID-19 Homer Tien, MD, MSc*†; Bruce Sawadsky, MD*; Michael Lewell, MD*; Michael Peddle, MD*; Wade Durham, A-EMCA, ACP(F)* Critical care transport organizations are nimble, oper- developing surge capacity, and responding to urgent, ationally focused institutions that can aid in managing unconventional requests for assistance. crises.1 Ornge provides air ambulance and critical care transport services to Ontario. From 12 bases, Ornge MAINTAINING OPERATIONAL READINESS BY ENSURING operates four PC-12 Next Generation fixed wing (FW) STAFF SAFETY aircraft, eight AW-139 rotary wing (RW) aircraft, and four critical care land ambulances (CCLA) on a 24/7 Northern communities are relatively isolated from basis. Ornge also contracts with private air carriers to COVID-19. To mitigate the risk of spread to northern provide lower acuity air ambulance services. Ornge per- communities and northern Ornge bases from the south, forms over 20,000 patient-related transports annually. we instituted a strict travel ban. We instituted a work from ’ We discuss Ornge s approach to preparing for the cor- home program for non–front-line staff, and split our Oper- onavirus disease 2019 (COVID-19) pandemic, and iden- ational Communications Centre (OCC) staff into two sep- tify potential unconventional roles. arate groups that worked out of two different locations. 1. Protecting staff physical health ORNGE DURING COVID-19 A. COVID-19 screening and personal protective pquipment As of April 30, 2020, Ornge has organized transport for and/or transported 325 patients with either a confirmed Protecting our staff has been our top priority. -
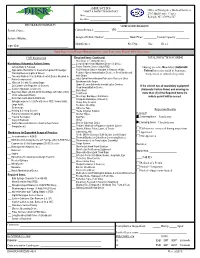
AMBULANCE BUS VEHICLE INSPECTION REPORT Office of Emergency Medical Services 2707 Mail Service Center Date: ______Raleigh, NC 27699-2707 Location: ______
AMBULANCE BUS VEHICLE INSPECTION REPORT Office of Emergency Medical Services 2707 Mail Service Center Date: ___________________________ Raleigh, NC 27699-2707 Location: ________________________ PROVIDER INFORMATION VEHICLE INFORMATION Provider Name: ______________________________ Current Permit #: _________ VIN: _________________________________________ System Affiliation: ____________________________ Assigned Vehicle Number: _______________ Model Year: ________ Patient Capacity: ________ Manufacturer: ______________________ Fuel Type: _____ Gas _____ Diesel _____ Viper ID #: ____________________________________ Ramp Inspections Require Mandatory Items; Spot Inspections Require A Full Inspection EMT Inspection Required Items Continued: TOTAL INSPECTION SCORING ___ Stair Chair or Folding Stretcher Mandatory (Automatic Failure) Items: ___ Cervical Spine Immobilization Device (S,M & L) ___ Vehicle Body & Function ___ Femur Traction Device (Adult/PED) Missing an entire Mandatory (Automatic ___ Appropriate Restraints for Crew & Non-patient Passenger ___ PED Restraint Device Available to Restrain <40lbs. Failure) Item may result in Summary ___ Warning Devices (Lights & Sirens) ___ Pediatric Spinal Immobilization Device or Short Backboard Suspension or refusal of a permit. ___ Two-way Radio in Front & Radio Control Device Mounted in with Straps Patient compartment ___ Adult Spinal Immobilization Extrication Device or Short ___ Wheeled Cot with Securing Straps Backboard with Straps ___ O2 Cylinder with Regulator (2 Sources) ___ Upper & Lower -

Acronyms Abbreviations &Terms
Acronyms Abbreviations &Terms A Capability Assurance Job Aid FEMA P-524 / July 2009 FEMA Acronyms Abbreviations and Terms Produced by the National Preparedness Directorate, National Integration Center, Incident Management Systems Integration Division Please direct requests for additional copies to: FEMA Publications (800) 480-2520 Or download the document from the Web: www.fema.gov/plan/prepare/faat.shtm U.S. Department of Homeland Security Federal Emergency Management Agency The FEMA Acronyms, Abbreviations & Terms (FAAT) List is not designed to be an authoritative source, merely a handy reference and a living document subject to periodic updating. Inclusion recognizes terminology existence, not legitimacy. Entries known to be obsolete (see new “Obsolete or Replaced” section near end of this document) are included because they may still appear in extant publications and correspondence. Your comments and recommendations are welcome. Please electronically forward your input or direct your questions to: [email protected] Please direct requests for additional copies to: FEMA Publications (800) 480-2520 Or download the document from the Web: www.fema.gov/plan/prepare/faat.shtm 2SR Second Stage Review ABEL Agent Based Economic Laboratory 4Wd Four Wheel Drive ABF Automatic Broadcast Feed A 1) Activity of Isotope ABHS Alcohol Based Hand Sanitizer 2) Ampere ABI Automated Broker Interface 3) Atomic Mass ABIH American Board of Industrial Hygiene A&E Architectural and Engineering ABIS see IDENT A&FM Aviation and Fire Management ABM Anti-Ballistic Missile -

York Region’S Response to the Ontario Ministry of Health’S Discussion Paper on Emergency Health Services Modernization
From: Switzer, Barbara on behalf of Regional Clerk Monday, March 2, 2020 3:32 PM Subject: Regional Council Decision - Response to Ontario Ministry of Health's Discussion Paper on Emergency Health Services Modernization Attachments: Original Staff Report - Response to Ontario Ministry of Health's Discuss....pdf CAUTION: This email originated from a source outside the City of Markham. DO NOT CLICK on any links or attachments, or reply unless you recognize the sender and know the content is safe. On February 27, 2020 Regional Council made the following decision: 1. Council approve Attachment 1 as York Region’s response to the Ontario Ministry of Health’s Discussion Paper on Emergency Health Services Modernization. 2. The Regional Clerk circulate the Region’s response to the following: Ministry of Health, Members of Provincial Parliament in York Region, Clerks of the nine local municipalities, Southlake Community Ontario Health Team, Eastern York Region and North Durham Ontario Health Team, Mackenzie Health Hospital, Association of Municipalities of Ontario, Ontario Association of Paramedic Chiefs and CUPE 905 — York Region Unit. The original staff report is attached for your information. Please contact Lisa Gonsalves, General Manager, Paramedic and Seniors Services at 1-877-464-9675 ext.72090 if you have any questions with respect to this matter. Regards, Christopher Raynor | Regional Clerk, Regional Clerk’s Office, Corporate Services ------------------------------------------------------------------------------------------------------------------------ The Regional Municipality of York | 17250 Yonge Street | Newmarket, ON L3Y 6Z1 O: 1-877-464-9675 ext. 71300 | [email protected] | www.york.ca Our Mission: Working together to serve our thriving communities – today and tomorrow 1 The Regional Municipality of York Regional Council Community and Health Services February 27, 2020 Report of the Commissioner of Community and Health Services Response to Ontario Ministry of Health’s Discussion Paper on Emergency Health Services Modernization 1. -
Download the Amburesponse Overview
KIT A TURNKEY SOLUTION FOR MASS CASUALTY TRANSPORT AND RESPONSE The AmbuBus® Kit, available exclusively from First Line Technology, is an effective and efficient solution for mass evacuation, shelter-in-place, firefighter rehab, and transport of special needs patients, casualties, and those who require non- ambulatory transport. The AmbuBus® Kit will quickly and easily retrofit vehicles of opportunity (like school or metro buses) into mass patient transport vehicles, or it can be used free-standing to bunk patients or responders. The modular design of a standard AmbuBus® consists of a two-frame kit that can be configured to carry up to 18 non-ambulatory patients. The all- inclusive AmbuBus® Stretcher Conversion Kit contains everything needed to assemble the frames – no power tools required – and is both ruggedized and palletized to allow for quick, simple logistics for pre-positioning and emergency response. Users: Mass Casualty Transport, Mortuary Response, Surge Capacity, Special Needs Evacuation, Firefighter Rehab AMBUBUS® HIGHLIGHTS • Installs around seats, vents, and wheel wells • Accommodates NATO Regular or Oversized Stretchers • Illustrated Instructions • Assembles in Two Hours • Ruggedized Transport Kit • Minimal Maintenance • Adjustable to Fit Most Vehicles of Opportunity • Use Free-Standing or in Transport Vehicles • Multiple Configurations • Includes all Installation Tools MASS CASUALTY TRANSPORT INFORMATION All-Hazards Response As cities prepared for the 2005 hurricane season (which included Hurricanes Katrina and Rita), many found it difficult or impossible to evacuate the special needs population from hospitals and other long-term care facilities. In New Orleans, hundreds of buses that could have been converted were left in the flood plain and were eventually ruined due to water damage. -

The Hyattsville Volunteer Fire Department
The Hyattsville Volunteer Fire Department Company Rookie Manual Last Revision Summer 2013 Edited by Matthew Leonard Contribution from Summer 2009 Rookie Book & Spring 2013 Live-ins Introduction Welcome to the Hyattsville Volunteer Fire Department. Whether you are new to the fire service or have been with other companies in the past the HVFD is a unique fire company in a unique fire department. The HVFD has a strong sense of pride and tradition that dates back to 1888 with a sincere dedication to serig the itizes of the Cit of Hattsille ad Prie George’s County, Maryland. One thing you will be doing regardless of the prior experience you have is serving as a volunteer in a busy metropolitan fire department. Our fire company responds annually to thousands of emergencies including medical emergencies, vehicle accidents, technical rescues, structural fires, and general calls for assistae to the people e sere. The HVFD is oe of ol to opaies i Prie George’s County that operates all 3 primary suppression and rescue services as well as a BLS ambulance. Because of the diversity of our tasks the HVFD must maintain a high level of discipline and a high level of competence in its members. This book is designed to assist you with becoming a well-trained and knowledgeable volunteer and will help you attain any goals you wish to achieve whether it is in fire or EMS. There is a basic level study material as well as benchmarks within these pages and exams to help you gauge you proficiency and obtain various statuses as you move through your probation and rookie hood. -

Technical Specification TORSUS TERRASTORM AMBULANCE 4X4
Technical specification TORSUS TERRASTORM AMBULANCE 4x4 based on Volkswagen Crafter 35 4Motion TORSUS TERRASTORM AMBULANCE – best European ambulance bus designed for the emergency, safe transportation and rescue of people life in the off-road conditions. Specification Wheelbase: L3 3640 mm Body height (passenger compartment): H3 1861 mm Engine: 2,0l biTDI 130 kW/177 h.p. Transmission: 6-MT, 4x4 (automatic 8-speed, 4х4 -optional) Vehicle dimensions (L3H3 base): Base equipment: Body: • High roof Н3, body color • Body trimming according to regulations color scheme and TORSUS design solution • Special protective underbody covering (below the tornado line) • Protective arc footboards along the left and right sides • Heat-insulating windshield made of laminated glass • Reinforced front bumper, increased approach angles • Two-leaves rear doors with the possibility to open inside • Sliding right doors in the medical compartment with middle fixation • Left exterior mirror, convex, with integrated LED turn signal and wide viewing angle • Right exterior mirror, convex, with integrated LED turn signal and wide viewing angle • Exterior mirrors, electronically adjustable and heated • Cabin doors, reinforced driver's door hinges Protective body elements • Reinforced metal protection for the engine, transmission and rear differential • Side steps on the left and right sideboards Transmission, drive: • All-wheel drive, 4х4 • Gearbox: 6-speed • Mechanical differential lock of rear axle Suspension and wheels: • HEAVY DUTY SUSPENSION WITH OFF ROAD RIMS AND -

Bucks County Ehs Annual Report Annex Fiscal Year 2019-2020
BUCKS COUNTY EHS ANNUAL REPORT ANNEX FISCAL YEAR 2019-2020 Authority Report are due within 30 calendar days of the end of each state fiscal year (June 30th) Jeryl L. DeGideo, Director [email protected] Ver 1. 06 Jun 2020 TABLE OF CONTENTS Other Reportable Areas of Interest ANNEX A – Regional Council Position Descriptions ANNEX B – Conflict of Interest Policy ANNEX C – Comprehensive Regional EMS System Plan Comprehensive Regional EMS System Plan ANNEX D – Meeting and Minutes ANNEX E – Continuity of Operations Plan (COOP) ANNEX F – Regional Mass Casualty Plan ANNEX G – Cumulative Equipment Inventory Ver 1. 06 Jun 2020 OTHER REPORTABLE AREAS OF INTEREST Work Force Development - NIMS Percentage of staff completing NIMS Training (ICS) 90% Indicate the number of staff members who completed the following NIMS Courses 5.5 total staff IS-100 5.5 IS-700 5.5 IS-800 5.5 IS-200 5.5 IS-703 5. ICS-300 4. ICS-400 3. Workforce Development Narrative: Currently looking for an ICS-400 for one staff member. EMS Agency Mergers or Acquisitions Number of EMS Agency Mergers or Acquisitions 0 Mergers or Acquisitions Narrative: We had no mergers or acquisitions nor is there any talk of any in the works. ‐ 1 ‐ ANNEX A Regional Council Position Descriptions Position Descriptions shall include: • Position Title • Responsibilities/Duties • Number of Hours per Week Worked • Percentage of Work Time Allocated to the Contract • Line of Supervision • Education/Training Requirements • Work Experience/Qualifications ‐ 2 ‐ COUNTY OF BUCKS JOB TITLE: Director of Emergency Health JOB CODE: 0038 Services DEPARTMENT: Emergency Health Services UNION: 11 FLSA STATUS: Exempt GRADE: REVISION 08/2019 DATE: POSITION SUMMARY: Responsible for planning, organizing, implementing and directing an emergency medical services system through the County Office of Emergency Health Services. -

North Carolina Ambulance Strike Team
North Carolina Ambulance Strike Team Mission Plan Version 1--September 2014 1 | P a g e Table of Contents INTRODUCTION ....................................................................................................................................................... 3 PURPOSE, SCOPE, SITUATION, AND ASSUMPTIONS ..................................................................................... 4 CONCEPT OF OPERATIONS .................................................................................................................................. 6 ROLES AND RESPONSIBILITIES ........................................................................................................................ 10 AST PROGRAM STANDARDS .............................................................................................................................. 14 APPENDIX A: ACRONYMS ................................................................................................................................... 16 APPENDIX B: AST/ATF CODE OF CONDUCT .................................................................................................. 17 APPENDIX C: RECOMMENDED STANDARDS FOR AST/ATF LEADERS ................................................. 19 APPENDIX D: RECOMMENDED STANDARDS FOR AST/ATF PACKAGES .............................................. 21 APPENDIX E: RECOMMENDED STANDARD EQUIPMENT AND SUPPLIES ............................................ 22 APPENDIX F: STANDARD POLICIES AND OPERATING GUIDANCE FOR AST/ATF UNITS ............... 24 -

An Evolving Comprehensive Team Approach Juan Duchesne Kenji
Damage Control in Trauma Care An Evolving Comprehensive Team Approach Juan Duchesne Kenji Inaba Mansoor Ali Khan Editors https://t.me/MedicalBooksStore 123 Damage Control in Trauma Care Juan Duchesne • Kenji Inaba Mansoor Ali Khan Editors Damage Control in Trauma Care An Evolving Comprehensive Team Approach Editors Juan Duchesne Kenji Inaba Tulane School of Medicine LAC+USC Medical Center New Orleans University of Southern California Louisiana Los Angeles USA California USA Mansoor Ali Khan St Mary’s Hospital Imperial College Healthcare NHS Trust London United Kingdom ISBN 978-3-319-72606-9 ISBN 978-3-319-72607-6 (eBook) https://doi.org/10.1007/978-3-319-72607-6 Library of Congress Control Number: 2018937983 © Springer International Publishing AG, part of Springer Nature 2018 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication.