An Evolving Comprehensive Team Approach Juan Duchesne Kenji
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Proposed Emergency Health Services and Community Paramedicine Legislation
PROPOSED EMERGENCY HEALTH SERVICES AND COMMUNITY PARAMEDICINE LEGISLATION Discussion Guide 1 Introduction The Department of Health and Community Services is in the process of drafting legislation to govern the Provincial Road Ambulance Program (the program). Input from stakeholders and the public is an essential element in drafting this legislation as it will ensure it meets the needs of the ambulance industry and residents of the province. This document provides a brief overview of the program and the components that are being considered for inclusion in the new legislation. The document includes six areas for consideration, including the current state and changes being proposed. As we are inviting feedback, each section also includes specific questions and spaces for a response. There is also an opportunity for respondents to indicate any additional feedback at the end of the document. A glossary of terms used in this document can be found in Annex 1. Background Newfoundland and Labrador is the only jurisdiction in Canada without legislation governing the delivery of ambulance services. In 2012, the Department engaged an external consultant, Fitch and Associates, to conduct a review of the program, which involved stakeholder consultations both during and following the review. In the 2013 report, Fitch indicated numerous issues with the program, among them, a lack of consolidated legislation. Fitch expressed concern that multiple pieces of legislation and multiple organizations were responsible for different elements of the program. Fitch made 10 recommendations to government to transform the program into an efficient and effective ambulance service. One of the key recommendations was the development of dedicated emergency medical services legislation, so that one organization has the responsibility for ambulance service delivery and the authority to make changes necessary to improve the program. -

August 10, 2016 8701 Arliss Street Building Explosion And
8701 Arliss Street August 10, 2016 Post Incident Analysis Montgomery County Fire & Rescue Service POST INCIDENT ANALYSIS 8701 Arliss Street Silver Spring, MD 20910 August 10, 2016 Submitted by: Battalion Chief Tracy McDonald Battalion 1, C Shift Contributors Battalion Chief Mike Leigh Captain Jason Masters Lieutenant Jason Smith Lieutenant Shawn Goodbrod 1 8701 Arliss Street August 10, 2016 Post Incident Analysis Table of Contents TABLE OF CONTENTS ....................................................................................................................... 2 INTRODUCTION ............................................................................................................................... 4 BUILDING STRUCTURE / SITE LAYOUT .............................................................................................. 6 FIREGROUND OPERATIONS .............................................................................................................. 8 Overview .................................................................................................................................................. 8 Operations ............................................................................................................................................... 8 Initial EMS Operations ........................................................................................................................... 14 Command Team Operations ................................................................................................................. -

Critical Care Transport in the Time of COVID-19
ORNGE SUPPLEMENT Critical care transport in the time of COVID-19 Homer Tien, MD, MSc*†; Bruce Sawadsky, MD*; Michael Lewell, MD*; Michael Peddle, MD*; Wade Durham, A-EMCA, ACP(F)* Critical care transport organizations are nimble, oper- developing surge capacity, and responding to urgent, ationally focused institutions that can aid in managing unconventional requests for assistance. crises.1 Ornge provides air ambulance and critical care transport services to Ontario. From 12 bases, Ornge MAINTAINING OPERATIONAL READINESS BY ENSURING operates four PC-12 Next Generation fixed wing (FW) STAFF SAFETY aircraft, eight AW-139 rotary wing (RW) aircraft, and four critical care land ambulances (CCLA) on a 24/7 Northern communities are relatively isolated from basis. Ornge also contracts with private air carriers to COVID-19. To mitigate the risk of spread to northern provide lower acuity air ambulance services. Ornge per- communities and northern Ornge bases from the south, forms over 20,000 patient-related transports annually. we instituted a strict travel ban. We instituted a work from ’ We discuss Ornge s approach to preparing for the cor- home program for non–front-line staff, and split our Oper- onavirus disease 2019 (COVID-19) pandemic, and iden- ational Communications Centre (OCC) staff into two sep- tify potential unconventional roles. arate groups that worked out of two different locations. 1. Protecting staff physical health ORNGE DURING COVID-19 A. COVID-19 screening and personal protective pquipment As of April 30, 2020, Ornge has organized transport for and/or transported 325 patients with either a confirmed Protecting our staff has been our top priority. -
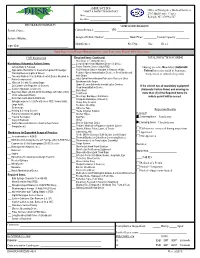
AMBULANCE BUS VEHICLE INSPECTION REPORT Office of Emergency Medical Services 2707 Mail Service Center Date: ______Raleigh, NC 27699-2707 Location: ______
AMBULANCE BUS VEHICLE INSPECTION REPORT Office of Emergency Medical Services 2707 Mail Service Center Date: ___________________________ Raleigh, NC 27699-2707 Location: ________________________ PROVIDER INFORMATION VEHICLE INFORMATION Provider Name: ______________________________ Current Permit #: _________ VIN: _________________________________________ System Affiliation: ____________________________ Assigned Vehicle Number: _______________ Model Year: ________ Patient Capacity: ________ Manufacturer: ______________________ Fuel Type: _____ Gas _____ Diesel _____ Viper ID #: ____________________________________ Ramp Inspections Require Mandatory Items; Spot Inspections Require A Full Inspection EMT Inspection Required Items Continued: TOTAL INSPECTION SCORING ___ Stair Chair or Folding Stretcher Mandatory (Automatic Failure) Items: ___ Cervical Spine Immobilization Device (S,M & L) ___ Vehicle Body & Function ___ Femur Traction Device (Adult/PED) Missing an entire Mandatory (Automatic ___ Appropriate Restraints for Crew & Non-patient Passenger ___ PED Restraint Device Available to Restrain <40lbs. Failure) Item may result in Summary ___ Warning Devices (Lights & Sirens) ___ Pediatric Spinal Immobilization Device or Short Backboard Suspension or refusal of a permit. ___ Two-way Radio in Front & Radio Control Device Mounted in with Straps Patient compartment ___ Adult Spinal Immobilization Extrication Device or Short ___ Wheeled Cot with Securing Straps Backboard with Straps ___ O2 Cylinder with Regulator (2 Sources) ___ Upper & Lower -

1 SUPPLEMENTAL MATERIAL Use of Non-Indicated Cardiac
SUPPLEMENTAL MATERIAL Use of Non-Indicated Cardiac Testing in Low-Risk Patients: Choosing Wisely METHODS SUPPLEMENT Data Source and Study Population Using the Medicare 40% denominator file, we identified all fee-for-service Medicare beneficiaries enrolled in Medicare Parts A, B, and D (inpatient, outpatient and prescription coverage), 2006-2011, and created six annual enrollment cohorts. We excluded beneficiaries with a gap of one or more months in fee-for-service Medicare Parts A, B, or D enrollment during a calendar year. We limited our analysis to beneficiaries aged 66-80. Beneficiary characteristics, including age, sex, race/ethnicity (black, Hispanic, other), and Medicaid enrollment, were obtained from the Medicare denominator file. Residential ZIP Codes were used to assign each beneficiary to one of 306 Dartmouth Atlas of Health Care hospital referral regions (HRRs). Information on regional physician workforce in 2006 was obtained from the Dartmouth Atlas of Health Care. Defining Low- and High-Risk Cohorts To identify annual cohorts of low-risk patients, each beneficiary was annually assigned a cardiovascular disease risk status (low or high) based on records in Medicare Carrier, Outpatient, MedPAR, Hospice and Prescription Drug Event files. For each annual enrollment cohort, beneficiaries with no evidence of significant cardiovascular disease or cardiovascular disease risk were deemed low-risk and those with such conditions were deemed high-risk. Using Hierarchical Condition Category International Classification of Disease, Ninth Revision, code lists, the following diagnoses (appearing in two physician claims or one hospital claim) were considered evidence of high cardiovascular disease risk: HIV/AIDS, diabetes, drug or alcohol abuse/dependence, shock, cardiac disease (e.g. -

A Case of Thoracic Aortic Injury Caused by Multiple Rib Fractures
3 Case Report Page 1 of 3 A case of thoracic aortic injury caused by multiple rib fractures Weigang Zhao#, Weiwei He#, Yi Yang, Yonghong Zhao Department of Thoracic Surgery, Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Shanghai, China #These authors contributed equally to this work. Correspondence to: Yonghong Zhao. Department of Thoracic Surgery, Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, 600 Yishanlu Road, Shanghai 200233, China. Email: [email protected]. Abstract: Thoracic aortic injury is fatal but rare in blunt chest trauma, which usually requires urgent surgical treatment. It is mostly caused by posterior rib fractures. Chest wall stabilization (CWS) has been widely performed in patients with multiple rib fractures all over the world in the past two decades with satisfactory outcomes. However, the surgical treatment of posterior rib fracture within 2–3 cm from transverse process is still a difficult problem for thoracic surgeons. Under this circumstance, rib-transverse process internal fixation method was developed and widely performed for above patients at present. In this article, we presented a case of thoracic aortic injury caused by multiple rib fractures. A 54-year-old female was admitted to our hospital with dyspnea and severe chest pain caused by a falling object. Thoracic aortic injury with multiple rib fractures were diagnosed basing on image date and emergency CWS was performed for this patient. Rib-transverse process internal fixation was not performed in this case since the patients combined with transverse process fracture. We firstly performed transverse process resection combined with CWS for this patient. The results of our study showed this method is safe and feasible for patients with multiple rib fractures combined with transverse process fracture. -

Vertical Perspective Medical Assistance Program
Kansas Vertical Perspective Medical Assistance Program December 2006 Provider Bulletin Number 688 General Providers Emergent and Nonemergent Diagnosis Code List Attached is a list of diagnosis codes and whether the Kansas Medical Assistance Program (KMAP) considers the code to be emergent or nonemergent. Providers are responsible for validating whether a particular diagnosis code is covered by KMAP under the beneficiary’s benefit plan and that all program requirements are met. This list does not imply or guarantee payment for listed diagnosis codes. Information about the Kansas Medical Assistance Program as well as provider manuals and other publications are on the KMAP Web site at https://www.kmap-state-ks.us. If you have any questions, please contact the KMAP Customer Service Center at 1-800-933-6593 (in-state providers) or (785) 274-5990 between 7:30 a.m. and 5:30 p.m., Monday through Friday. EDS is the fiscal agent and administrator of the Kansas Medical Assistance Program for the Kansas Health Policy Authority. Page 1 of 347 Emergency Indicators as noted by KMAP: N – Never considered emergent S – Sometimes considered emergent (through supporting medical documentation) Y – Always considered emergent Diagnosis Emergency Diagnosis Code Description Code Indicator 0010 Cholera due to Vibrio Cholerae S 0011 Cholera due to Vibrio Cholerae El Tor S 0019 Unspecified Cholera S 019 Late Effects of Tuberculosis N 0020 Typhoid Fever S 0021 Paratyphoid Fever A S 0022 Paratyphoid Fever B S 0023 Paratyphoid Fever C S 024 Glanders Y 025 Melioidosis -

2012-2013 Research Abstracts CASE SURGERY a Compilation of Investigations Made by Case Surgery Physicians, Research Scientists and Distinguished Colleagues
2012-2013 Research Abstracts CASE SURGERY A compilation of investigations made by Case Surgery physicians, research scientists and distinguished colleagues. 12-13Abstracts.indd 1 10/22/13 12:51 PM Dear Colleague: I am pleased to share with you our 2012-2013 research abstracts. The Department of Surgery provides a multi-specialty academic environment where ideas are exchanged and cooperative research programs are planned. The 2012-13 academic year has been a productive one for the Department and its members. The work produced has been presented at national and international forums and published in prestigious journals. The Department of Surgery will continue to expand its research and educational endeavors in the coming year. We welcome your interest in our Department’s research and clinical studies. If you would like additional information, please call 216.844.3209 or visit our website at www.casesurgery.com. Sincerely, Jeffrey L. Ponsky, MD Oliver H. Payne Professor and Chair 12-13Abstracts.indd 2 10/22/13 12:51 PM Special thanks to the Case School of Medicine Biologic Research Unit for their continued support. Section 1: Cardiac Surgery CONCURRENT ASYMPTOMATIC CARDIAC MYXOMA AND RENAL CELL CARCINOMA ......................................................................................................................... 3 Vineeta Gahlawat, MD, Yakov Elgudin, MD Table of Contents Table Section 2: Colorectal Surgery PROCESS IMPROVEMENT IN COLORECTAL SURGERY: MODIFICATIONS TO AN ESTABLISHED ENHANCED RECOVERY PROTOCOL ................................................... -

Endovascular Stent in Traumatic Thoracic Aortic Dissection
Case Report http://dx.doi.org/10.4070/kcj.2012.42.5.341 Print ISSN 1738-5520 • On-line ISSN 1738-5555 Korean Circulation Journal Endovascular Stent in Traumatic Thoracic Aortic Dissection Mi Ok Jang, MD, Ju Han Kim, MD, Sang Ki Oh, MD, Min Goo Lee, MD, Keun Ho Park, MD, Doo Sun Sim, MD, Young Joon Hong, MD, Youngkeun Ahn, MD, and Myung Ho Jeong, MD The Heart Center of Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea Traumatic thoracic aortic injury is typically fatal. However, recent improvements in pre-hospital care and diagnostic modalities have re- sulted in an increased number of patients with traumatic aortic injury arriving alive at the hospital. Also, the morbidity and mortality as- sociated with endovascular repair are significantly lower than with conventional open surgery in traumatic thoracic aorta injury. We expe- rienced two cases of successful management of traumatic thoracic aortic dissection with endovascular stents caused by traffic accidents. (Korean Circ J 2012;42:341-344) KEY WORDS: Aorta, thoracic; Dissection; Aortography; Multidetector computed tomography. Introduction Cases Patients with blunt traumatic thoracic aorta injuries are increas- Case 1 ingly admitted to hospital due to the increasing number of traffic A 28-year-old male suffered from a traffic accident while in a car. accidents per day. Traumatic thoracic aortic injury is typically fatal. His mental status was confused but brain CT revealed non-specific The thoracic aorta wall ruptures after blunt thorax trauma and if not findings. He had no known history of hypertension, diabetes, hep- treated, has very poor outcome with an initial survival rate ranging atitis, and pulmonary tuberculosis. -

Early Appropriate Care of Orthopaedic Injuries in Elderly Multiple-Trauma Patients Michael S
Scientific Poster #115 Polytrauma OTA 2014 Early Appropriate Care of Orthopaedic Injuries in Elderly Multiple-Trauma Patients Michael S. Reich, MD; Andrea J. Dolenc, BS; Timothy A. Moore, MD; Heather A. Vallier, MD; MetroHealth Medical Center, Cleveland, Ohio, USA Background/Purpose: This study was designed to evaluate clinical predictors of complications in multiply injured elderly trauma patients with orthopaedic injuries. Previous work from our institution has established resuscitation parameters that minimize complications with early fracture management. Protocol recommendations included definitive management of mechanically unstable fractures of the pelvis, acetabulum, spine, and femur within 36 hours, provided the patient demonstrated a positive response to resuscitative efforts, including lactate <4.0, pH ≥7.25, or base excess (BE) ≥–5.5 mmol/L. This protocol has been applied to all skeletally mature patients, but patients with advanced age or preexisting medical issues may require unique parameters to mitigate risk of complications and mortality. Methods: Between October 2010 and March 2013, 376 skeletally mature patients with 426 unstable fractures of the pelvis (n = 73), acetabulum (n = 58), spine (n = 112), and/or proximal or diaphyseal femur fractures (n = 183) were treated at a Level I trauma center and were prospectively studied. Subgroups of patients age ≤30 years (n = 114) and ≥60 years (n = 37), treated within 36 hours of injury, were compared. Low-energy fractures were excluded. The ISS, Glasgow Coma Score (GCS), and American Society of Anesthesiologists (ASA) classification were determined. Lactate, pH, and BE were measured at 8-hour intervals and perioperatively. Complications included pneumonia, pulmonary embolism (PE), acute renal failure (ARF), acute respiratory distress syndrome (ARDS), multiple organ failure (MOF), deep vein thrombosis (DVT), infection, sepsis, and death. -

Critical Care Management of Traumatic Brain Injury
Critical care management of traumatic brain injury Handbook of Clinical Neurology 2017 Final submitted version corrected for changes during editorial processing (with the permission of the publishers) DK Menon1,* and A Ercole1 1Division of Anaesthesia, University of Cambridge and Neurosciences/Trauma Critical Care Unit, Addenbrooke's Hospital,Cambridge, UK *Corresponding author. Email [email protected] Abstract Traumatic brain injury (TBI) is a growing global problem, which is responsible for a substantial burden of disability and death, and which generates substantial healthcare costs. High-quality intensive care can save lives and improve the quality of outcome. TBI is extremely heterogeneous in terms of clinical presentation, pathophysiology, and outcome. Current approaches to the critical care management of TBI are not underpinned by high-quality evidence, and many of the current therapies in use have not shown benefit in randomized control trials. However, observational studies have informed the development of authoritative international guidelines, and the use of multimodality monitoring may facilitate rational approaches to optimizing acute physiology, allowing clinicians to optimize the balance between benefit and risk from these interventions in individual patients. Such approaches, along with the emerging impact of advanced neuroimaging, genomics, and protein biomarkers, could lead to the development of precision medicine approaches to the intensive care management of TBI. 1 Introduction Traumatic brain injury (TBI) is an important cause for admission to intensive care units (ICUs) in general, and to neurocritical care units in particular. National population-based figures for ICU caseload (as opposed to more specific stratification into mild, moderate, or severe TBI) are difficult to find, but the UK Intensive Care National Audit and Research Centre (ICNARC, 2015) reported that in 2014{2015, approximately 2% of all ICU admissions and about 10% of admissions to neurocritical care units were due to TBI. -

Complications Are Reduced with a Protocol to Standardize Timing of Fixation Based on Response to Resuscitation Heather A
Vallier et al. Journal of Orthopaedic Surgery and Research (2015) 10:155 DOI 10.1186/s13018-015-0298-1 RESEARCH ARTICLE Open Access Complications are reduced with a protocol to standardize timing of fixation based on response to resuscitation Heather A. Vallier1*, Timothy A. Moore1,2, John J. Como3, Patricia A. Wilczewski3, Michael P. Steinmetz4, Karl G. Wagner5, Charles E. Smith5, Xiao-Feng Wang1 and Andrea J. Dolenc1 Abstract Background: Our group developed a protocol, entitled Early Appropriate Care (EAC), to determine timing of definitive fracture fixation based on presence and severity of metabolic acidosis. We hypothesized that utilization of EAC would result in fewer complications than a historical cohort and that EAC patients with definitive fixation within 36 h would have fewer complications than those treated at a later time. Methods: Three hundred thirty-five patients with mean age 39.2 years and mean Injury Severity Score (ISS) 26.9 and 380 fractures of the femur (n = 173), pelvic ring (n = 71), acetabulum (n = 57), and/or spine (n = 79) were prospectively evaluated. The EAC protocol recommended definitive fixation within 36 h if lactate <4.0 mmol/L, pH ≥7.25, or base excess (BE) ≥−5.5 mmol/L. Complications including infections, sepsis, DVT, organ failure, pneumonia, acute respiratory distress syndrome (ARDS), and pulmonary embolism (PE) were identified and compared for early and delayed patients and with a historical cohort. Results: All 335 patients achieved the desired level of resuscitation within 36 h of injury. Two hundred sixty-nine (80 %) were treated within 36 h, and 66 had protocol violations, treated on a delayed basis, due to surgeon choice in 71 %.