Loss and Grief Manual
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tethered a COMPANION BOOK for the Tethered Album
Tethered A COMPANION BOOK for the Tethered Album Letters to You From Jesus To Give You HOPE and INSTRUCTION as given to Clare And Ezekiel Du Bois as well as Carol Jennings Edited and Compiled by Carol Jennings Cover Illustration courtesy of: Ain Vares, The Parable of the Ten Virgins www.ainvaresart.com Copyright © 2016 Clare And Ezekiel Du Bois Published by Heartdwellers.org All Rights Reserved. 2 NOTICE: You are encouraged to distribute copies of this document through any means, electronic or in printed form. You may post this material, in whole or in part, on your website or anywhere else. But we do request that you include this notice so others may know they can copy and distribute as well. This book is available as a free ebook at the website: http://www.HeartDwellers.org Other Still Small Voice venues are: Still Small Voice Youtube channel: https://www.youtube.com/user/claredubois/featured Still Small Voice Facebook: Heartdwellers Blog: https://heartdwellingwithjesus.wordpress.com/ Blog: www.stillsmallvoicetriage.org 3 Foreword…………………………………………..………………………………………..………….pg 6 What Just Happened?............................................................................................................................pg 8 What Jesus wants you to know from Him………………………………………………………....pg 10 Some questions you might have……………………………………………………….....................pg 11 *The question is burning in your mind, ‘But why?’…………………....pg 11 *What do I need to do now? …………………………………………...pg 11 *You ask of Me (Jesus) – ‘What now?’ ………………………….….....pg -

Billboard #1 Records
THE BILLBOARD #1 ALBUMS COUNTRY ALBUM SALES DEBUTPEAK ARTIST TITLE LABEL SEL# (1) 5/11/19 1 1. SCOTT, Dylan Nothing To Do Town (EP) Curb HEATSEEKER ALBUMS DEBUTPEAK ARTIST TITLE LABEL SEL# (1) 7/8/95 1 1. PERFECT STRANGER You Have The Right To Remain Silent Curb 77799 (1) 11/3/01 1 2. HOLY, Steve Blue Moon Curb 77972 (1) 5/21/11 1 3. AUGUST, Chris No Far Away Fervent/Curb-Word 888065 MUSIC VIDEO SALES DEBUTPEAK ARTIST TITLE LABEL SEL# (28) 5/8/93 1 1. STEVENS, Ray Comedy Video Classics Curb 77703 (6) 5/7/94 1 2. STEVENS, Ray Live Curb 77706 TOP CATALOG COUNTRY ALBUMS DEBUTPEAK ARTIST TITLE LABEL SEL# (1) 6/15/91 1 1. WILLIAMS, Hank Jr. Greatest Hits Elektra/Curb 60193 (2) 8/21/93 1 2. JUDDS, The Greatest Hits RCA/Curb 8318 (26) 6/19/99 1 3. MCGRAW, Tim Everywhere Curb 77886 (18) 4/1/00 1 4. MESSINA, Jo Dee I'm Alright Curb 77904 (1) 8/17/02 1 5. SOUNDTRACK Coyote Ugly Curb 78703 (54) 12/7/02 1 6. MCGRAW, Tim Greatest Hits Curb 77978 (2) 1/19/08 1 7. MCGRAW, Tim Greatest Hits, Vol. 2: Reflected Curb 78891 (4) 6/16/11 1 8. MCGRAW, Tim Number One Hits Curb 79205 TOP CHRISTIAN ALBUMS DEBUTPEAK ARTIST TITLE LABEL SEL# (35) 9/27/97 1 1. RIMES, LeAnn You Light Up My Life: The Inspirational Album Curb 77885 (35) 10/7/01 1 2. P.O.D. Satellite Atlant/Curb-Word 83496 (5) 6/8/02 1 3. -
Cost University $2 Million by '88 of the Student Code of by Dave Urbanski Conduct
Today's - weather: Cloudy and NON PROfiT ORG US POSTAGE cold. Chance PAID of snow. Newark. Del ., Permtt No 26 Highs in the 30s. ' Vot 111 No. 40 Student Center, University of Delaware, Newark, Delaware 19716 Friday, March 7, 1986 r '~Budget cuts to · cost university $2 million by '88 of the Student Code of by Dave Urbanski Conduct. Assistant-News Editor The new policy. which was The university is slated to created in response to the lose as much as $2 million in harassment of gay and lesbian federal funding for building students in the past two years. maintenance, utility and other broadens the scope of the administrative costs over the policy, Dean of Students next two years. Timothy Brooks said. The proposed cuts, part of The revised code redefines the Gramm-Rudman deficit harassment as "deliberately reduction plan. are scheduled acting with intent to harass to begin April 1, Provost L. any member or guest of the Leon Campbell told the univer university community" based sity Faculty Senate during its on the person's race, sex, meeting Monday. religion, political beliefs, sex "We cannot accept this ual orienlation or disability. change," university Treasurer The original policy specified Robert Harrison said. only racism, sexism and anti The Federal Office of Semitism a~ harassment. Management and Budget is in Todd Christie <AS 86), a charge of reducing the funds, Delaware Undergraduate Stu which are known as indirect dent Congress•representative costs, Harrison said. to the Faculty Senate, said he The university . faculty was pleased with the policy favors the cuts in indirect change. -

Idioms-And-Expressions.Pdf
Idioms and Expressions by David Holmes A method for learning and remembering idioms and expressions I wrote this model as a teaching device during the time I was working in Bangkok, Thai- land, as a legal editor and language consultant, with one of the Big Four Legal and Tax companies, KPMG (during my afternoon job) after teaching at the university. When I had no legal documents to edit and no individual advising to do (which was quite frequently) I would sit at my desk, (like some old character out of a Charles Dickens’ novel) and prepare language materials to be used for helping professionals who had learned English as a second language—for even up to fifteen years in school—but who were still unable to follow a movie in English, understand the World News on TV, or converse in a colloquial style, because they’d never had a chance to hear and learn com- mon, everyday expressions such as, “It’s a done deal!” or “Drop whatever you’re doing.” Because misunderstandings of such idioms and expressions frequently caused miscom- munication between our management teams and foreign clients, I was asked to try to as- sist. I am happy to be able to share the materials that follow, such as they are, in the hope that they may be of some use and benefit to others. The simple teaching device I used was three-fold: 1. Make a note of an idiom/expression 2. Define and explain it in understandable words (including synonyms.) 3. Give at least three sample sentences to illustrate how the expression is used in context. -

Skillet Hero Download Mp3
Skillet Hero Download Mp3 Skillet Hero Download Mp3 1 / 3 2 / 3 Skillet Hero The Legion Of Doom Remix Awake And Remixed EP VIDEO HD Official New Song 2011. play. download. Skillet Hero Official Video mp3.. mp3 download. 4.7M . skillet sick of it official video.mp3 . Hero Mp3 Lagu Video Mp4 Hero hero skillet mp3 ﺗﻨﺰﻳﻞ - Mp3 (6.40 MB) Download. Lirik lagu serta video hero mp4 atau 3gp.. hero skillet mp3 download mp3 Download Skillet Hero Ringtone submitted by Tushar in Music ringtones category. Total downloads so ..ﺩﻧﺪﻧﻬﺎ , download mp4 far: 1933.. Skillet - Awake download free mp3 flac. , Skillet, Awake (CD, Album, Enh), Atlantic, Ardent Records, , US, , Skillet. Download I Can Be Your Hero Baby Mp3 Download Skull Mp3. Song Details. Title: Skillet - Hero (Official Video); Uploader: Atlantic Records; Duration: 03:17 .... ... Gta San Andreas Cleo Pc Download, Download Guitar Hero 5 Skillet Ps2 Via ... Line input jack les you connect your laptop, tablet, smartphone, or MP3 player ... skillet hero skillet hero, skillet hero lyrics, skillet hero mp3 download, skillet hero female singer, skillet hero chords, skillet hero tab, skillet hero live, skillet hero roblox id, skillet heroes never die, skillet hero 1 hour Hero (Skillet song) Download Lagu Skillet Burn It Down mp3 for free (03:17). ... Skillet skillet hero, download audio mp3 skillet hero, 128kbps skillet hero, full hq ... skillet hero mp3 download Skillet Monster (Official Video) - Download MP3 Online - Convert Youtube Video to mp3 instantly #mp3converter #mp3download #downloadmp3 - Skillet ... skillet hero chords Listen to Skillet - Hero Instrumental and write some lyrics on RapPad - featuring a lyrics editor with built in syllable counter, rhyming dictionary ... -

XS March 2020 Update
XS March 2020 Update Artist Song Title Artist Song Title 3 Seconds of Summer Teeth What I Know Now 311 Creatures (For A While) Beyonce Spirit AJR Sober Up Bieber, Justin Yummy Alaina, Lauren Other Side, The Blue, Jonas & Theresa Rex What I Like About You Other Side, The Bridges, Leon Beyond (Instrumental Version) Brightman, Sarah & Hot I Lost My Heart to a Aldean, Jason Camouflage Hat Gossip Starship Trooper Camouflage Hat Brothers Osbourne 21 Summer (Instrumental Version) Brown, James Payback, The Got What I Got Brown, Kane For My Daughter Got What I Got For My Daughter (Instrumental Version) (Instrumental Version) Andress, Ingrid Both Bryan, Luke Cold Beer Drinker Both (Instrumental What She Wants Tonight Version) What She Wants Tonight Lady Lake (Instrumental Version) Lady Lake (Instrumental Buble, Michael Fever Version) Cabello, Camila Living Proof Arizona Zervas Roxanne Cabello, Camilla Shameless Arthur, James You Deserve Better Capaldi, Lewis Before You Go Ballerini, Kelsea Better Luck Next Time Someone You Loved Club Cash, Johnny I Won't Back Down Club (Instrumental Cassidy, Eva & David Gray You Don't Know Me Version) Cave, Nick & the Bad Henry Lee Banderas, Antonio Cancion Del Mariachi Seeds & PJ Harvey Bareilles, Sara I Choose You Celeste Strange Sweet as Whole Chesney, Kenny Tip of my Tongue Barrett, Gabby I Hope Cinnamon, Gerry Bonny, The Bastille Quarter Past Midnight Clarkson, Kelly Underneath the Tree Bastille & Alessia Cara Another Place Clean Bandit & Demi Solo Batey, Joey Toss a Coin to Your Lovato Witcher Clemmons, Riley -

The Role of Music in the Lives of Homeless Young People
Tuned Souls: The Role of Music in the Lives of Homeless Young People Jill P. Woelfer A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Washington 2014 Reading Committee: David Hendry, Chair Susan Kemp Batya Friedman Julie A. Hersberger Program Authorized to Offer Degree: The Information School ©Copyright 2014 Jill P. Woelfer University of Washington Abstract Tuned Souls: The Role of Music is the Lives of Homeless Young People Jill P. Woelfer Chair of the Supervisory Committee: Associate Professor, David G. Hendry The Information School Although music is considered to be an important part of adolescence and young adulthood, little is known about music and homeless youth. Accordingly, this dissertation research investigated the role of music in the lives of homeless young people, aged 15-25. The study was conducted in Seattle, Washington and Vancouver, British Columbia and engaged homeless young people (n=202) and service providers staff who work at agencies that provide support for homeless young people (n=24). Homeless young people completed surveys (n=202), design activities, which included drawing and story writing (n=149), and semi-structured interviews (n=40). Service providers completed semi-structured interviews (n=24). Data analysis included descriptive analysis of survey data and qualitative coding of the design activities and interview responses. Findings indicated that music was an important part of everyday life for homeless young people, who listened to music daily (98%), owned music players (89%), and had wide- ranging and eclectic tastes in music which did not vary based on location. -
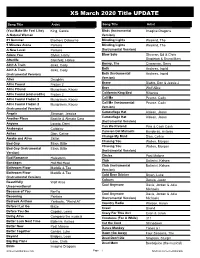
XS March 2020 Title UPDATE
XS March 2020 Title UPDATE Song Title Artist Song Title Artist (You Make Me Feel Like) King, Carole Birds (Instrumental Imagine Dragons A Natural Woman Version) 21 Summer Brothers Osbourne Blinding Lights Weeknd, The 5 Minutes Alone Pantera Blinding Lights Weeknd, The A New Level Pantera (Instrumental Version) Adore You Styles, Harry Blow Solo Sheeran, Ed & Chris Afterlife Steinfeld, Hailee Stapleton & Bruno Mars Bonny, The Ain't A Train Jinks, Cody Cinnamon, Gerry Both Ain't A Train Jinks, Cody Andress, Ingrid (Instrumental Version) Both (Instrumental Andress, Ingrid Version) Alive Daughtry Brave All is Found Frozen 2 Diablo, Don & Jessie J Bros All is FOund Musgraves, Kacey Wolf Alice California King Bed All is Found (end credits) Frozen 2 Rihanna Call Me All is Found Frozen 2 Musgraves, Kacey Pearce, Carly Call Me (Instrumental All is Found Frozen 2 Musgraves, Kacey Pearce, Carly (Instrumental Version) Version) Camouflage Hat Angels Simpson, Jessica Aldean, Jason Camouflage Hat Another Place Bastille & Alessia Cara Aldean, Jason (Instrumental Version) Anyone Lovato, Demi Can We Pretend Pink & Cash Cash Arabesque Coldplay Cancion Del Mariachi Banderas, Antonio Ashes Dion, Celine Change My Mind Dion, Celine Awake and Alive Skillet Chasing You Wallen, Morgan Bad Guy Eilish, Billie Chasing You Wallen, Morgan Bad Guy (Instrumental Eilish, Billie (Instrumental Version) Version) Circles Post Malone Bad Romance Halestorm Club Ballerini, Kelsea Bandages Hot Hot Heat Club (Instrumental Ballerini, Kelsea Bathroom Floor Maddie & Tae Version) Bathroom -
Maximum Ride T H E ANGEL EXPERIMENT
Maximum Ride T H E ANGEL EXPERIMENT James Patterson WARNER BOOKS NEW YORK BOSTON Copyright © 2005 by Suejack, Inc. All rights reserved. No part of this book may be reproduced in any form or by any electronic or mechanical means, including information storage and retrieval systems, without permission in writing from the publisher, except by a reviewer who may quote brief passages in a review. Warner Vision and the Warner Vision logo are registered trademarks of Time Warner Book Group Inc. Time Warner Book Group 1271 Avenue of the Americas, New York, NY 10020 Visit our Web site at www.twbookmark.com First Mass Market Edition: May 2006 First published in hardcover by Little, Brown and Company in April 2005 The characters and events portrayed in this book are fictitious. Any similarity to real persons, living or dead, is coincidental and not intended by the author. Cover design by Gail Doobinin Cover image of girl © Kamil Vojnar/Photonica, city © Roger Wood/Corbis Logo design by Jon Valk Produced in cooperation with Alloy Entertainment Library of Congress Cataloguing-in-Publication Data Maximum Ride : the angel experiment / by James Patterson. — 1st ed. p.cm. Summary: After the mutant Erasers abduct the youngest member of their group, the "bird kids," who are the result of genetic experimentation, take off in pursuit and find themselves struggling to understand their own origins and purpose. ISBN: 0-316-15556-X(HC) ISBN: 0-446-61779-2 (MM) [1. Genetic engineering — Fiction. 2. Adventure and adventurers — Fiction.] 1. Title. 10 9876543 2 1 Q-BF Printed in the United States of America For Jennifer Rudolph Walsh; Hadley, Griffin, and Wyatt Zangwill Gabrielle Charbonnet; Monina and Piera Varela Suzie and Jack MaryEllen and Andrew Carole, Brigid, and Meredith Fly, babies, fly! To the reader: The idea for Maximum Ride comes from earlier books of mine called When the Wind Blows and The Lake House, which also feature a character named Max who escapes from a quite despicable School. -

Karaoke with a Message – August 16, 2019 – 8:30PM
Another Protest Song: Karaoke with a Message – August 16, 2019 – 8:30PM a project of Angel Nevarez and Valerie Tevere for SOMA Summer 2019 at La Morenita Canta Bar (Puente de la Morena 50, 11870 Ciudad de México, MX) karaoke provided by La Morenita Canta Bar songbook edited by Angel Nevarez and Valerie Tevere ( ) 18840 (Ghost) Riders In The Sky Johnny Cash 10274 (I Am Not A) Robot Marina & Diamonds 00005 (I Can't Get No) Satisfaction Rolling Stones 17636 (I Hate) Everything About You Three Days Grace 15910 (I Want To) Thank You Freddie Jackson 05545 (I'm Not Your) Steppin' Stone Monkees 06305 (It's) A Beautiful Mornin' Rascals 19116 (Just Like) Starting Over John Lennon 15128 (Keep Feeling) Fascination Human League 04132 (Reach Up For The) Sunrise Duran Duran 05241 (Sittin' On) The Dock Of The Bay Otis Redding 17305 (Taking My) Life Away Default 15437 (Who Says) You Can't Have It All Alan Jackson # 07630 18 'til I Die Bryan Adams 20759 1994 Jason Aldean 03370 1999 Prince 07147 2 Legit 2 Quit MC Hammer 18961 21 Guns Green Day 004-m 21st Century Digital Boy Bad Religion 08057 21 Questions 50 Cent & Nate Dogg 00714 24 Hours At A Time Marshall Tucker Band 01379 25 Or 6 To 4 Chicago 14375 3 Strange Days School Of Fish 08711 4 Minutes Madonna 08867 4 Minutes Madonna & Justin Timberlake 09981 4 Minutes Avant 18883 5 Miles To Empty Brownstone 13317 500 Miles Peter Paul & Mary 00082 59th Street Bridge Song Simon & Garfunkel 00384 9 To 5 Dolly Parton 08937 99 Luftballons Nena 03637 99 Problems Jay-Z 03855 99 Red Balloons Nena 22405 1-800-273-8255 -

Skillet Bio 2013
SKILLET RISE Skillet recently made headlines when their last album, Awake, became one of just three rock albums to be certified platinum in 2012, forming an improbable triumvirate with the Black Keys’ El Camino and Mumford & Sons’ Babel. The news that Skillet had sold more than a million albums in the U.S. came as a shock to all but the band’s wildly diverse horde of fans, male and female, young and old—known as Panheads—whose still-swelling ranks now officially number in the seven-digit range. This remarkable achievement was announced just as Skillet was putting the finishing touches on their eagerly awaited follow-up album, Rise (Atlantic/Word). Unwilling to stand pat or rest on their laurels, the band—lead vocalist/bassist John Cooper, guitarist/keyboardist Korey Cooper (John’s wife), drummer/duet partner Jen Ledger and lead guitarist Seth Morrison, making his first appearance on record with Skillet—continue to explore new terrain on Rise, expertly produced by Howard Benson, who previously helmed the mega- successful Awake. Eager for new challenges, Cooper threw himself into collaborative songwriting to a far greater degree than ever before, co-writing the uplifting title song and the lacerating first single “Sick of it” with Scott Stevens, founder/leader of the L.A.-based Exies, while teaming with Nashville songsmiths Tom Douglas and Zac Maloy on the timely and anthemic “American Noise,” which Cooper considers to be the strongest song Skillet has yet recorded. On “American Noise” and the joyous “Good to Be Alive,” the band explores new stylistic territory, bringing an element of heartland rock into their aggressive, theatrical approach. -

Skillet Collide Album Download Collide
skillet collide album download Collide. John L. Cooper has finally hit his stride with Skillet. Collide is a disc that chugs along with guitars out front, screaming vocals, and a raw intensity that strips the band of its electronic nuances. Opting for a much more aggressive sound, the band leans on guitar riffs while synths are more tastefully added. Songs like "Forsaken" and "Savior" are perfect examples of unadulterated rock bliss. Even when the band veers away from the heaviness à la the well-placed orchestration on "Collide," the meat of the tune still ends up rocking out. With this disc, Skillet takes a firm stance toward honing a sound that is marketed to Generation X. With cuts to back it, they may have found the right vehicle to reach those ears. Skillet collide album download. In an age of re-releases and "special editions" galore, Skillet is the latest to join the throes of album revisitations, offering a CD/DVD "Deluxe Edition" of their hit 2006 record Comatose . For this particular second time around, Comatose is given an additional song to its original eleven- song tracklisting that had been recorded too late to make it onto the original release last year. And in addition to these twelve studio songs, five "acoustic" renditions of tracks featured herein are tacked on at the end. Finally, to round out this re-release, a DVD is added as a second disc that includes four music videos. As a whole, the packaging for Comatose: Deluxe Edition , which boasted new artwork, merely offers a slip cover with new artwork on the front and back, and the actual CD case retains its previous back and front cover.